Pulmonary and Ileal Tuberculosis Presenting as Fever of Undetermined Origin
Gajanan Surewad1, Ivona Lobo2, Preeti Shanbag3
1 Fellow, Department of Neonatology, G S Medical College & KEM Hospital, Parel, Mumbai, India.
2 Professor & Head, Department of Pulmonary Medicine, ESI-PGIMSR & MGM Hospital, Parel, Mumbai, India.
3 Professor & Head, Department of Paediatrics, ESI-PGIMSR & MGM Hospital, Parel, Mumbai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Preeti Shanbag, 801, Yashowan, TH Kataria Marg, Mahim, Mumbai-400016, India. Phone : 9869128012, E-mail : pshanbag@gmail.com
A 12-year-old girl presented with prolonged fever with no obvious focus on either history or clinical examination. High-resolution computerized tomography of the chest revealed the ‘tree-in-bud’ sign in the right lung and necrotic mediastinal lymph nodes. Barium meal showed multiple ileal strictures. The child was treated with anti-tuberculous therapy for six months. At follow-up six months later, the child had gained weight and had no signs of intestinal obstruction. Tuberculosis is a common cause of fever of undetermined origin and should be investigated for especially in countries with a high prevalence.
Gastro-intestinal, Tuberculosis, Tree-in-bud sign
Case Report
A 12-year-old girl was referred to us in September 2012 with a one-month history of moderate-to-high grade fever. There was no history of cough, abdominal pain or alteration in bowel habits and no contact with tuberculosis. The child had received some treatment with a private practitioner but details were not available.
On examination, the child was febrile (temperature 38.6o C). Pulse rate was 128/minute, respiratory rate was 32/minute and blood pressure 110/72mmHg. Her height and weight were 128 cm and 25 kg respectively, both below the 3rd percentile for age and sex. There was no significant lymph node enlargement. Abdominal examination revealed hepatosplenomegaly.
Investigations showed haemoglobin of 13.3g/dL, total white blood cell count of 8800/cu.mm, and a differential count of neutrophils 68%, lymphocytes 30% and monocytes 2%. Peripheral smear was negative for malarial parasites. The erythrocyte sedimentation rate was 31 mm at one hour. The Mantoux test showed no induration and chest X-ray was normal. Liver and renal function tests were within normal limits. The urine and blood cultures were subsequently reported as sterile. Sputum for acid-fast bacilli was negative on two occasions.
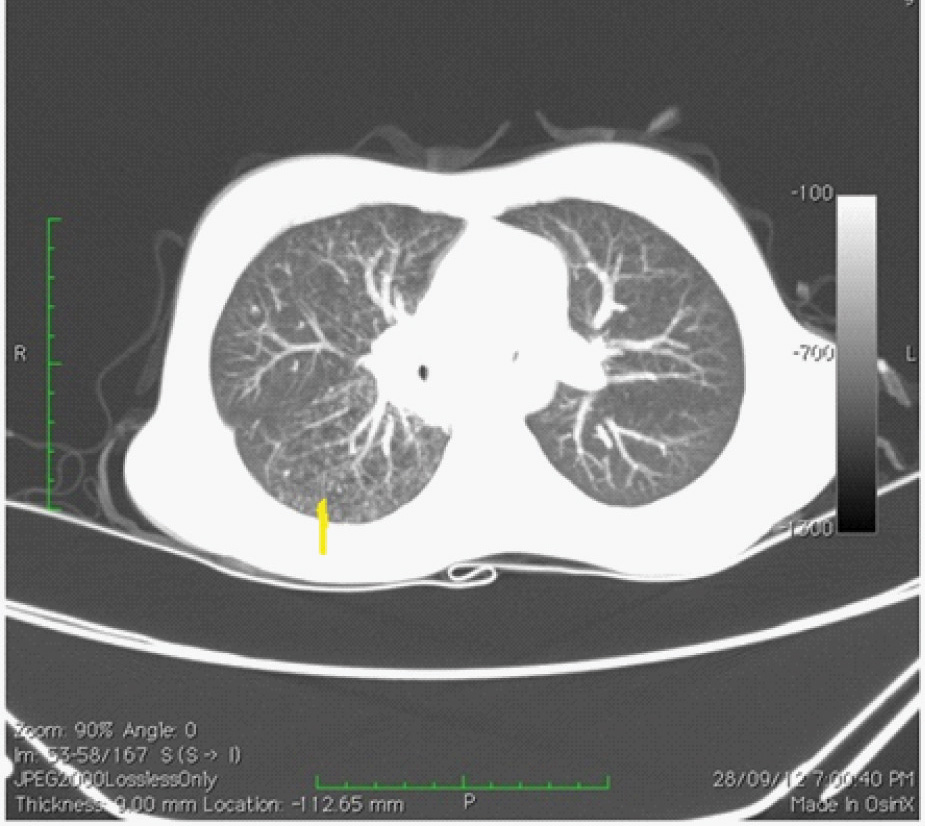
The child was started on intravenous ceftriaxone with a presumptive diagnosis of enteric fever pending the culture reports. However high grade fever continued despite 5 days of intravenous antibiotics, hence high-resolution computerized tomography (HRCT) of chest and abdominal ultrasonography (USG) were done. The HRCT of chest showed the classical “tree-in-bud” sign [Table/Fig-1] in the right lung with enlarged necrotic mediastinal lymph nodes. USG of the abdomen showed dilated ileal loops. Barium meal showed multiple ileal strictures [Table/Fig-2]. Enzyme-linked immunosorbent assay (ELISA) for HIV was negative.
High-resolution computerized tomography of chest (axial section) showing the classical “tree-in-bud” sign (arrow) in right lung
Barium meal showing multiple strictures (arrows) in the ileum

The child was started on anti-tuberculous therapy with isoniazide, rifampicin, pyrazinamide and ethambutol for two months followed by isoniazide and rifampicin for the remaining four months. At follow-up six months later, the child had gained weight (4kg) and had no symptoms of intestinal obstruction.
Discussion
Our patient presented with fever of undetermined origin and failure to thrive as evidenced by her height and weight parameters. HRCT of the chest showed the classical “tree-in-bud” sign in the right lung as well as necrotic mediastinal lymph nodes. Despite such extensive lesions on HRCT chest, the child had no cough or respiratory symptoms.
Though barium meal showed multiple strictures, our patient did not complain of abdominal pain or altered bowel habits. Shah I et al., studying abdominal tuberculosis in children in Mumbai, found fever and abdominal pain to be the most common presenting symptoms in their patients [1]. Also, Basu S et al., found abdominal pain and fever to be the commonest presenting symptoms (90% and 73% respectively) in their study of abdominal tuberculosis in Indian children. Abdominal distension was seen in 67% and alteration of bowel habits in 52% of their children [2]. In adults however, Saaiq M et al., from Pakistan, found that 67.4% of patients with abdominal tuberculosis presented with acute abdomen [3].
Our patient had concomitant pulmonary tuberculosis as seen in the HRCT scan of the chest. Basu S et al., found associated pulmonary tuberculosis in 40% of their children with abdominal tuberculosis, while the corresponding number in Pakistani adults was 9.9% [2,3].
Sputum for acid-fast bacilli was negative. We started anti-tuberculous therapy on a presumptive diagnosis of pulmonary and ileal tuberculosis and the patient responded well to it. In countries with a high prevalence of tuberculosis, a therapeutic trial of anti-tuberculous drugs may be given if the clinical picture is compatible [4].
Conclusion
Our patient presented with fever of undetermined origin and no specific localizing features. Investigations revealed extensive lesions suggestive of tuberculosis, both in the chest and abdomen. Tuberculosis is a common cause of fever of undetermined origin in both developing and developed countries and should always be considered in the differential diagnosis in such patients.
[1]. Shah I, Uppuluri R, Clinical profile of abdominal tuberculosis in childrenIndian J Med Sci 2010 64:204-09. [Google Scholar]
[2]. Basu S, Ganguly S, Chandra PK, Basu S, Clinical profile and outcome of abdominal tuberculosis in Indian childrenSingapore Med J 2007 48:900-05. [Google Scholar]
[3]. Saaiq M, Shah SA, Zubair M, Abdominal tuberculosis: epidemiologic profile and management experience of 233 casesJ Pak Med Assoc 2012 62:704-07. [Google Scholar]
[4]. Chow A, Robinson JL, Fever of unknown origin in children: a systematic reviewWorld J Pediatr 2011 7:5-10. [Google Scholar]