Can a Tight Saree Wear Cause Cancer? – A Rare Case Report
Subathira Balasundaram1, Rathnadevi Ramadas2, Janos Stumpf3, Khader A K Hussain4, Karthikeyan Perumal5
1 Consultant, Department of Radiation Oncology, Apollo Speciality Hospital, Apollo Speciality Hospital, Chennai, India.
2 Consultant, Department of Radiation Oncology, Apollo Speciality Hospital, Apollo Speciality Hospital, Chennai, India.
3 Advisor, Cyberknife and Oncology Services, Department of Radiation Oncology, Apollo Speciality Hospital, Apollo Speciality Hospital, Chennai, India.
4 Senior Resident, Department of Surgical Oncology, Apollo Speciality Hospital, Apollo Speciality Hospital, Chennai, India.
5 Senior Resident, Department of Radiation Oncology, Apollo Speciality Hospital, Apollo Speciality Hospital, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Karthikeyan Perumal, C/o Dr. Ratna Devi, Department of Radiation Oncology, Apollo Specialty Hospital, Chennai, India. Phone : 8807128231, E-mail : sindash@yahoo.com
Skin cancer is rare in India with an incidence of about less than 1% of all cancers. Saree Cancer, a kind of skin cancer is rarer entity, which arises from the frequent abrasion over skin caused by tying the rope in inskirts, often tied tightly so that the saree does not slip. This causes hyperpigmented abrasion, ulcer and then may lead to cancer.
This report is about a 40-year-old female with non-healing ulcer of six months duration with rapid increase in size over the past one month. The ulcer measured 4x2 cm in size. The patient underwent excision of the tumour and the margins were positive. Re-excision was done for positive margins and re-growth of the tumour. This is one the first few reports on saree cancer.
Dhoti cancer, Marjolin’s ulcer, Saree cancer, Waist dermatoses
Case Report
A 40-year-old pleasant lady presented with complaints of non-healing ulcer in the right hip region of six months duration. There was a history of recurrent ulcer over the right hip region exactly on the place where she ties the saree. Ulcer had increased in size for the past one month and associated with pain.
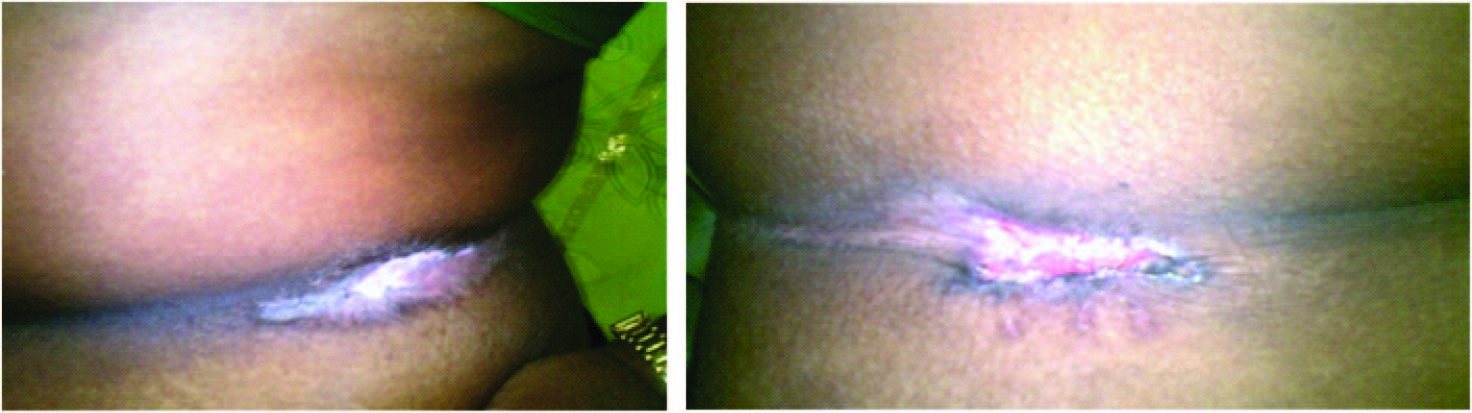
Clinical examination revealed an ulcer 4x2 cm in the right hip region with pale granulation tissue with sloping edges with thick indurated base and 1x1 cm proliferating growth was seen. No nodes were palpable in the inguinal region. Similar hyperpigmentation and peeling of skin of the left side hip was also present [Table/Fig-1a & b].
(a)Hypopigmentation and Excoriation in Left Hip (b) Ulcer in Right Hip region
Excision biopsy showed well differentiated squamous cell carcinoma. Gross Pathological examination showed an ulceroproliferative growth measuring 2.2x1.6 cm extending upto lateral resected margin. Microscopic pathological examination showed skin with keratin pearl formation suggestive of well differentiated squamous cell carcinoma with the surgical resected margin involved by the tumour.
The patient reported to us one month later with an ulcer about 3x4 cm in the right hip region, possibly due to re-growth and left hip showed hypopigmentation with skin excoriation. This patient was treated by wide local excision in the right lateral hip and left hip.
Gross Pathological examination revealed a lesion measuring 3.5x2.5x0.8 cm. Microscopic features showed an infiltrating carcinoma with the tumour cells forming small clusters and nodules composed of cells with high nuclear to cytoplasmic ratio and hyperchromatic nuclei. The center of some of these cell cluster were squamous eddies while at the periphery there was palisading of the tumour nuclei; mitotic features were consistent with moderately differentiated grade II squamous cell carcinoma; tumour invading to a depth of 3 mm. All resected margins were free of tumour.
Sections from the left waist showed a vascular lesion centered in the papillary dermis and mid-dermis. The lesion was composed of ecstatic and dilated thin caliber vascular channels lined by flattened endothelial cells and lumen showed red cell. The overlying dermis was hyperkeratotic. The histomorphology was that of a vascular malformation suggestive of angiokeratoma.
She was followed up for two years without recurrence.
Discussion
Marjolin described malignant degeneration of a chronic wound synonymous with a variety of cancers which arise in any scar tissue or chronic ulcers in 1828 [1]. Usually, the ulcers are SCCs that occur at sites of previous burns, scars, sinuses, pressure ulcers, trauma, sites of osteomyelitis, chronic friction [2] and prolonged heat exposure (Kangri contact) [3].
Khanolkar and Suryabai first described ‘dhoti cancer’ in 1945 [4]. Saree is the traditional female costume in south Asian countries, worn with an in-skirt fastened to the waist by a cord, which can induce waist-line dermatosis in female [2]. Waist dermatoses due to saree can degenerate as malignancy [5,6].
The incidence of malignancy in scar tissues is 0.1-2.5%. Saree is a type of female costume and dhoti is a male costume which is unique to the Indian subcontinent [4]. The persistent and the long term wearing of this costume results in depigmentation and glazing of the skin, acanthosis, scar and ulceration and subsequent, but very slow, malignant changes [4].
“Saree Cancer” is the term used for malignancy arising from waist dermatosis. Very few papers have been published on saree cancer and no article on this topic is available in Pubmed. Search Term “Saree Cancer” yields only one related article in Pubmed.
One study of 140 cases of waist-line lesions associated with saree wearing did not report any malignant change in these [2]. Dermatoses like allergic and non-allergic contact dermatitis [7] and dermatophytoses [8] are more commonly seen in body-folds and in areas where there is sweating and perspiration. A study conducted in India could not find any association with factors, which are commonly accompanied by flexural dermatosis [3] like diabetes, obesity and atopy [5].
Mechanism
Several hypotheses have been postulated for malignant degeneration of chronic scar. They are summarized in [Table/Fig-2].
Hypothesis for malignant degeneration of chronic scar
| S. No. | Author | Mechanism |
|---|
| 1) | Glover et al., [9] | continuous irritation has an increased potential for malignant degeneration |
| 2) | Copcu et al., [10] | cycle of damage, irritation, and repair can lead to a malignant transformation |
| 3) | Castillo et al., [11] | depressed immunologic state which is produced by the surrounding scar tissue |
| 4) | Fishman et al., [12] | absence of lymphatic drainage from the scar allows a significant delay in the host immunologic recognition, and the antitumor immunologic response |
Conclusion
Saree has been worn by Indian women for centuries and the waist cancer is rather a rare phenomenon. However, chronic abrasion caused by the tight inskirts of saree causes dermatosis, which if unattended can degenerate to cancer in rare cases. Loose inskirt and awareness among physicians and patients as well on the existence of such condition can avoid the progression of waist dermatosis to cancer.
[1]. Trent JT, Kirsner RS, Wounds and malignancyAdv Skin Wound Care 2003 16(1):31-34. [Google Scholar]
[2]. Eapen BR, Shabana S, Anandan S, Waist dermatoses in Indian women wearing sareeIndian J Dermatol Venereol Leprol 2003 69(2):88-89. [Google Scholar]
[3]. Sibbald RG, Landolt SJ, Toth D, Skin and diabetesEndocrinol Metab Clin North Am 1996 25(2):463-72. [Google Scholar]
[4]. Lal S, Bain Jayanta, Singh AK, Shukla PK, Saree cancer: the malignant changes in chronic irritationJournal of Clinical and Diagnostic Research [serial online] 2012 6:896-98.Available from http://www.jcdr.net/back_issues.asp?issn=0973-709x&year=2012&month=June&volume=6&issue=5&page=896-898&id=2248 [Google Scholar]
[5]. Bakhshi GD, Borisa A, Tayade MB, Waist cancer: report of two casesJ Indian Med Assoc 2011 109(11):829-831. [Google Scholar]
[6]. Patil AS, Bakhshi GD, Puri YS, Gedham MC, Naik AV, Joshi RK, Saree cancerBombay Hospital Journal 2005 47(3):302-03. [Google Scholar]
[7]. James C, Shaw M, Allergic and non allergic eczematous dermatitisImmunology and Allegry Clinics of North America 1996 16:119-35.Available from: http://www.immunology.theclinics.com/article/S0889-8561(05)70239-3/abstract [Google Scholar]
[8]. Rinaldi MG, Dermatophytosis: epidemiological and microbiological updateJ Am Acad Dermatol 2000 43(5 Suppl):S120-24. [Google Scholar]
[9]. Glover DM, Kiehn CL, Marjolin’s ulcer; a preventable threat to function and lifeAm J Surg 1949 78(5):772-80. [Google Scholar]
[10]. Copcu E, Aktas A, Siman N, Oztan Y, Thirty-one cases of Marjolin’s ulcerClin Exp Dermatol 2003 28(2):138-41. [Google Scholar]
[11]. Castillo J, Goldsmith HS, Burn scar carcinomaCA Cancer J Clin 1968 18(3):140-42. [Google Scholar]
[12]. Fishman JR, Parker MG, Malignancy and chronic wounds: Marjolin’s ulcerJ Burn Care Rehabil 1991 12(3):218-23. [Google Scholar]