Tuberculosis is a major global health problem and ranks the second leading cause of death from an infectious disease worldwide [1]. India is the highest TB burden country accounting for more than one fifth of the global burden of tuberculosis. To tackle this problem, Revised National Tuberculosis Control Programme (RNTCP) based on the DOTS (Directly Observed Treatment-Short course) strategy has been made available in the entire country by March 2006. RNTCP has achieved improved cure rates and a success rate of 88% among new smear positive cases was reported in 2011[2,3].
The unfavourable outcomes under the RNTCP are death, default and failures. In 2011, death rate, default rate and failure rate among new smear positive cases was reported as 4%, 6% and 2% respectively [3]. Of these, default defined as interruption of treatment for more than two months; represents an important challenge for the control program. Default is considered as a potential cause of drug resistance [4]. Studies in India and other developing countries have focused on various causes and risk factors for default. Gender, alcoholism, treatment after default, poor knowledge of tuberculosis, irregular treatment and socioeconomic status are some of the factors which have been found to be associated with higher default rates [5,6]. Other factors related to the service providers like difficulty in accessing health facility, non-governmental DOT center and previous treatment from non-RNTCP providers have also been identified as reasons for non-completion of treatment [5,7]. Very few studies have been done in the recent past focusing on understanding the time of default. It is very important to correlate the reasons of default with time of default. This would help to identify specific issues in different phases of treatment that lead to default. The implementation of RNTCP has lowered the default rates, yet it has remained difficult to predict non-adherence to treatment.
This study describes the achievements under RNTCP in terms of conversion rates, treatment outcomes and pattern of time of default in patients on directly observed short-course treatment for Tuberculosis in Puducherry, South India.
Materials and Methods
Implementation of RNTCP in the Union Territory of Puducherry began in the year 2002. The Tuberculosis unit (TU) of Puducherry has a population of 9.49 lakhs with 21 designated microscopy centers (DMCs) including 8 medical colleges. It has an annual total case notification rate of 112 per lakh population and a cure rate of 85% among new smear positive cases [3].
In this record- based study, analysis of the cohort registered for treatment in the district tuberculosis center (DTC) of the TU Puducherry during the 1st and 2nd quarter of 2011 was done. This data was obtained from the TB treatment register maintained at the TU level. The information collected included age and gender of the patient, category of treatment, disease type, classification, date of initiation of treatment, sputum conversion at the end of intensive phase, outcome of treatment and date of outcome. Few patients registered under RNTCP but initiated on non-DOTS treatment were excluded from the study. As this study used only secondary data for analysis, ethical clearance was not obtained but necessary permission from the State Tuberculosis Officer was obtained. Retrospective calculation of the sample size was done using the formula: N= 4pq/d2. Taking p as proportion of default from previous report; p=6%; q= 1-p; d=50% of p; we obtained a sample size of 564, thus justifying the size of the cohort taken for analysis.
As per the RNCTP guidelines, category I included new patients with smear-positive pulmonary tuberculosis, new patients with extra-pulmonary tuberculosis and new patients with smear-negative pulmonary tuberculosis. Category II included patients who had been previously treated for tuberculosis and require re-treatment. This group included patients with relapse, treatment failure, defaulters and others. The intensive phase of treatment is for two months in categories I and for three months, in category II. The continuation phase is for four months in category I and for five months, in category II. The follow-up sputum smear examination is done at the end of two months of intensive phase, two months after starting the continuation phase and at the end of treatment. If the sputum smear remains positive during the first follow-up, the intensive phase is prolonged for one more month. Sputum conversion was assessed at the end of intensive phase or extended intensive phase in category I and at the end of three months for category II patients [8].
Outcome of treatment for a TB patient could be cured, treatment completed, defaulted, died, failure and transferred out [8]. Date of outcome was the date on which the last dose of drug was taken. A patient is declared cured if he was Initially sputum smear positive; has completed treatment and had negative sputum smears on two occasions, one of which was at the end of the treatment. Treatment completed was defined as a initially sputum smear positive patient who has completed treatment with negative smears at end of the intensive phase / two months in the continuation phase, but none at the end of the treatment is declared as treatment completed; or initially sputum smear negative patient who has received full course of treatment and has not become smear positive at the end of the treatment; or Extra pulmonary TB patient who has received full course of treatment and has not become smear positive during or at the end of treatment. Died was defined as a patient who died during the course of treatment regardless of any cause. Failure was any TB patient who is smear positive at five months or more after initiation of the treatment and not put on MDR-TB treatment. Default was a patient who had taken treatment for atleast one month and after treatment initiation has interrupted treatment consecutively for more than two months. Cure and treatment completion were considered as favorable outcomes, while default, death and failure were considered as unfavorable outcomes.
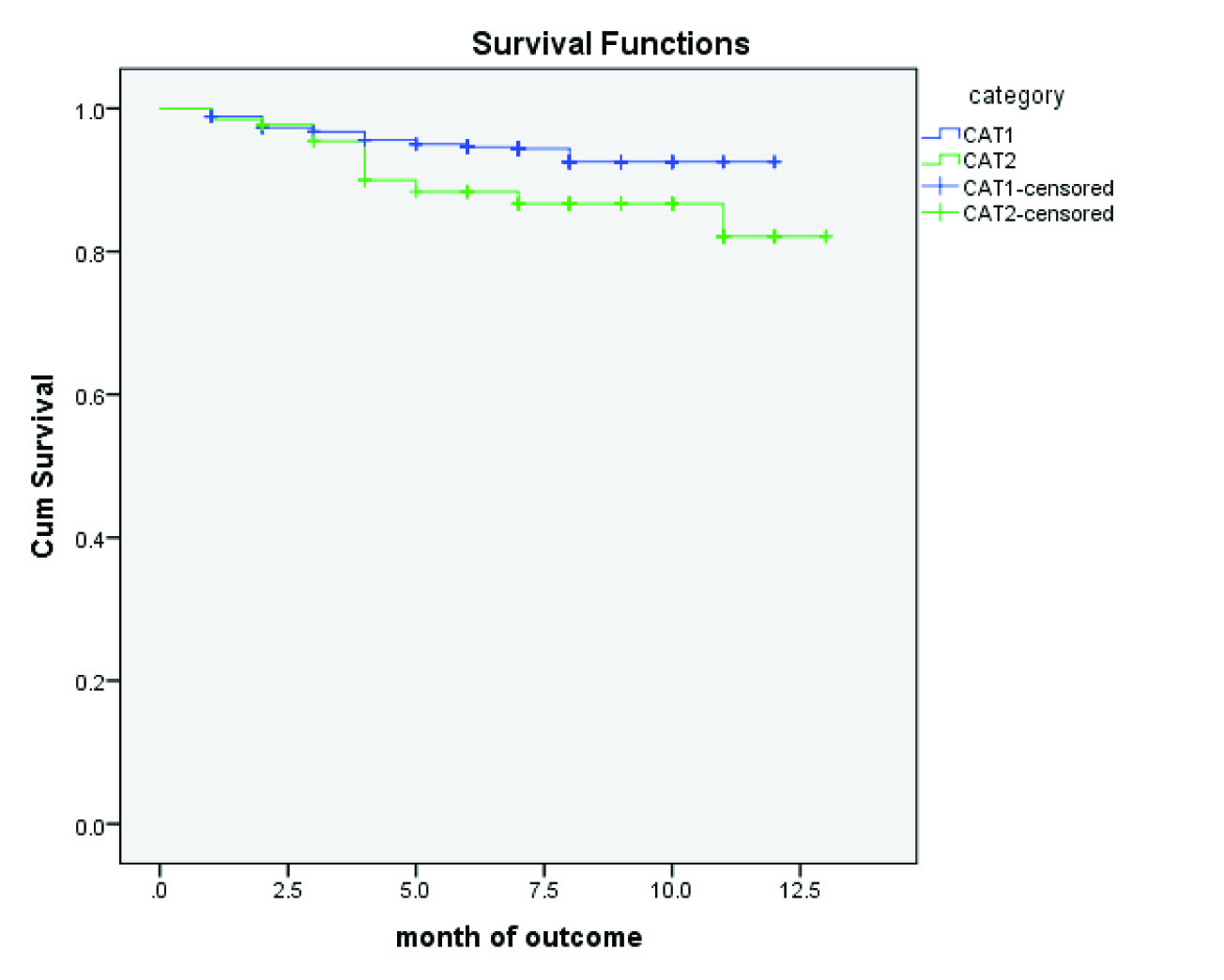
Default rate was calculated as the total number of patients who defaulted in each category divided by the total number of patients initiated on treatment in that particular category and was expressed as a proportion. Survival table for the data was generated from SPSS software. The cumulative probability of survival which is the conditional probability was used to draw the Kaplan Meiers plot. The Kaplan-Meier curve was drawn to make an overall estimate of patients continuing treatment at the end of each month in the two DOTS categories. The difference in the patterns of default over time between the groups was studied using the log rank test.
Analysis was done to study the time of default in smear-positive patients. The time of default was ascertained by calculating the difference between the date of initiation and date of outcome. The difference was divided by 30 to decide the month in which the event occurred. For example, if the difference was 100d, it was divided by 30 to get the number 3.33, which was inferred as ‘outcome (default) occurred in the fourth month.’ The events which were censored were death, treatment completion, cure, failure and transfer-out. Probability of default in each month was calculated. The cumulative default rate by the end of each month was calculated by adding the default rate in the particular month and the cumulative default rate in the previous month [4].
Statistical Analysis
Data entry was done by using Epidata software and analysed by using SPSS software v20. Categorical variables were expressed as proportions. The difference in the patterns of default over time between the two categories was studied using Kaplan-meiers analysis and log rank test. A p-value of 0.05 or less was taken as statistically significant.
Results
A total of 662 patients were registered for treatment in the TU in the first 2 quarters of the year 2011. Of these patients, 2 were started on RNTCP non-DOTS treatment and were excluded from the analysis. The annualized case notification rates for all TB cases were 141/lakh population and for new smear positive (NSP) cases was 61/lakh population. The annualized NSP case detection rate was estimated to be 81%.
Of the 660 registered patients, 31.2% were females and 68.8% were males. Pulmonary tuberculosis was reported in 74.1% patients and the rest 25.9% had extra-pulmonary forms of tuberculosis. Newly diagnosed TB cases comprised of 79.8% of the registered cases and 20.2% were retreatment cases. [Table/Fig-1] shows the distribution of the types of TB cases in each category.
Category-wise distribution of various types of TB cases.
| Category | Type of case | Number | Percentage |
|---|
| Category 1 | New smear positive | 286 | 54.2 |
| New smear negative | 80 | 15.2 |
| New extrapulmonary | 161 | 30.6 |
| Subtotal | 527 | 79.8 |
| Category 2 | Treatment after default | 44 | 33.2 |
| Failure | 16 | 12.0 |
| Relapse | 57 | 42.8 |
| Others | 16 | 12.0 |
| Subtotal | 133 | 20.2 |
| Total | 660 | 100.0 |
A total of 403 patients had smear-positive pulmonary tuberculosis of which 286(70.9%) were new cases. Amongst the 117(29.1%) smear-positive re-treatment tuberculosis patients in category II, 44 (37.6%) were patients put on re-treatment after default; 16 (13.7%), as a result of failure of previous treatment; and 57 (48.7%) had relapse.
Sputum conversion was assessed for the smear positive TB patients by doing a follow-up sputum examination at the end of intensive phase. Of the 403 smear positive TB patients 343 (85.1%) became sputum negative at the end of intensive phase. The sputum conversion rate for smear positive patients in category 1 and category 2 were 88.5% and 76.9% respectively.
Cure rate for NSP was 83.6% with a success rate of 85.7% among the new smear positive TB cases. The cure rate for retreatment smear positive TB cases was 65.4%. Unfavourable outcomes namely; death, default and failure in category 1 new cases was 2.7%, 5.9% and 2.1% respectively. Significantly higher rates of unfavourable outcomes were recorded in category 2 retreatment cases with a death rate, default rate and failure of 10.5%, 13.7% and 9% respectively.
[Table/Fig-2] lists the default rates over various periods (in months) after initiation of treatment amongst smear-positive patients in category I and category II. Maximum default is seen in the second month of treatment in category I, i.e., 1.5%; and in fourth month of treatment in category II, i.e. 5.8%. The cumulative default rate at the end of intensive phase (2 mnth) and at the end of treatment was 2.7% and 6.2% respectively for category 1 patients. For category 2 patients the cumulative default rate at the end of intensive phase (3 mnth) and at the end of treatment was 4.7% and 15.7% respectively. The overall default rate for all registered TB patients was 7.4%. The default rate was significantly higher in category 2(13.7%) when compared to category 1 (5.9%)
Default over time (in months) after initiation of treatment in smear positive TB patients on DOTS
| Category | Months | Patients initiated on treatment | Number of defaulters | Default rate in the month(%) | Cumulative default rate by the end of the month(%) |
|---|
| Category 1 | 1 | 527 | 6 | 1.13 | 1.13 |
| 2 | 517 | 8 | 1.54 | 2.68 |
| 3 | 504 | 3 | 0.59 | 3.27 |
| 4 | 496 | 6 | 1.20 | 4.47 |
| 5 | 486 | 3 | 0.61 | 5.09 |
| 6 | 479 | 2 | 0.42 | 5.50 |
| >6 | 430 | 3 | 0.69 | 6.20 |
| Category 2 | 1 | 131 | 2 | 1.53 | 1.53 |
| 2 | 129 | 1 | 0.78 | 2.30 |
| 3 | 125 | 3 | 2.40 | 4.70 |
| 4 | 120 | 7 | 5.83 | 10.54 |
| 5 | 110 | 2 | 1.82 | 12.35 |
| 6 | 107 | 0 | 0.00 | 12.35 |
| 7 | 103 | 2 | 1.94 | 14.30 |
| 8 | 96 | 0 | 0.00 | 14.30 |
| >8 | 71 | 1 | 1.41 | 15.70 |
[Table/Fig-3] provides the Kaplan-Meier analysis of default in the two DOTS categories and [Table/Fig-4] illustrates the Kaplan-Meier plot of default over time after initiation of treatment in the two DOTS categories. There was a significant difference in the default rate over time between the patients in the two DOTS categories [log rank statistic=6.534; d.f. =1; p=0.011]. In the second month of treatment, the default rates were similar in both categories, i.e., 2%. During the rest of the treatment period, the cumulative default rate was consistently higher in category II as compared to that in categories I. The dips seen in category II in [Table/Fig-4] indicate the higher default rates in this group throughout the treatment.
Kaplan-Meier analysis of default according to the DOTS categories.
| Category | Months | Patients initiated on treat-ment | No. of defaulters | No. censored | Probability of Default in the month (P) | Probability of survival (not Defaulting) in the month (1-P) | Cumulative Probability of survival (not Defaulting) in the month |
|---|
| Category 1 | 1 | 527 | 6 | 4 | 0.011 | 0.989 | 0.994 |
| 2 | 517 | 8 | 5 | 0.015 | 0.985 | 0.979 |
| 3 | 504 | 3 | 5 | 0.006 | 0.994 | 0.973 |
| 4 | 496 | 6 | 4 | 0.012 | 0.988 | 0.961 |
| 5 | 486 | 3 | 4 | 0.006 | 0.994 | 0.955 |
| 6 | 479 | 2 | 47 | 0.004 | 0.996 | 0.951 |
| >6 | 430 | 3 | 427 | 0.007 | 0.993 | 0.944 |
| Category 2 | 1 | 131 | 2 | 0 | 0.015 | 0.985 | 0.985 |
| 2 | 129 | 1 | 3 | 0.008 | 0.992 | 0.977 |
| 3 | 125 | 3 | 2 | 0.024 | 0.976 | 0.954 |
| 4 | 120 | 7 | 3 | 0.058 | 0.942 | 0.898 |
| 5 | 110 | 2 | 1 | 0.018 | 0.982 | 0.882 |
| 6 | 107 | 0 | 4 | 0.000 | 1.000 | 0.882 |
| 7 | 103 | 2 | 5 | 0.019 | 0.981 | 0.865 |
| 8 | 96 | 0 | 25 | 0.000 | 1.000 | 0.865 |
| >8 | 71 | 1 | 72 | 0.014 | 0.986 | 0.853 |
Kaplan-Meier plot of survival(not defaulting) probabilities in the two DOTS categories.
Discussion
The RNTCP in India has the objectives of achieving a case detection rate of 70% among the new sputum positive cases and a cure rate of 85% among the new sputum positive cases. It requires the sputum conversion at the end of intensive phase to be more than 90%; the adverse outcomes of death, default and failure to be less than 5%. This study shows that the TU has achieved the targets of the RNTCP with respect to cure rate, death rate and failure rate in new sputum positive. But the sputum conversion rate (88%) and default rate (5.9%) targets have not been achieved.
In the initial intensive phase of treatment under DOTS, four to five drugs are given to kill actively growing and semi-dormant bacilli, with an intention to bring about rapid smear conversion. The continuation phase eliminates most residual bacilli and reduces failure and relapses [4]. The use of four to five drug regimens in DOTS regime reduces the risk of development of drug resistance, failure and relapse. Poor compliance with treatment is also an important factor in the development of acquired drug resistance. A study by Johnson et al., demonstrated that among 48 isolates from patients with history of default; 45 showed drug resistance [9].
The earlier a patient defaults; more will be the chances of persistent smear-positive status and risk of drug resistance. In our study, 34% of the total default occurred in the second month of treatment; 47% in the third month and 73% in the fourth month of treatment. This transition between intensive phase and continuation phase appeared to be particularly vulnerable time for default. This period also coincides with improvement in the symptoms of the patient. This implies that greater supervision is required during this period. The DOTS provider should reinforce the need for taking complete treatment and should initiate early retrieval action, when the patient defaults. These findings are similar to that reported by other studies [2,5,10].
On analysing month-wise probability of default, the default rates were similar in both categories in the first 2 months, i.e., 2%. During the rest of the treatment period, the cumulative default rate was consistently higher in category II as compared to that in category I. The overall default rate for all registered TB patients was 7.4% and in those retreatment cases registered as treatment after default (N=44) the default rate was 9%. These findings are consistent with the findings of a study done by Jha et al.,[5] Paradesi et al.,[4] and Singh A et al.,[2] These findings suggest that more efforts are needed to promote adherence to treatment in the retreatment cases. Interruption of treatment among these retreatment patients should warrant retrieval of the patient on a priority basis.
The limitations of the study include the retrospective analysis using routine records which are subject to information bias. Categorization of the patients and their treatment outcomes as mentioned in the records were not independently validated, thus misclassification may not have been identified. But RNTCP maintains a system of ongoing internal programme evaluation and periodic reviews, so widespread misclassification would be unlikely. This study has not attempted to identify the risk factors for default in TB patients.
Conclusion
Defaulting from treatment is more common among the retreatment cases and usually occurs during the transition phase from intensive phase to continuation phase when symptoms improve. Health provider efforts like pre-treatment counseling and immediate retrieval of the treatment interrupters during the continuation phase would probably have an impact in lowering default rates.