Deroofing of Auricular Pseudocyst: Our Experience
Vinay S. Bhat1, Shilpa2, Nitha3, Ravi KS4
1Assistant Professor, Department of Ear, Nose and Throat, Adichunchanagiri Institute of Medical Sciences, B.G Nagara, Mandya District, Karnataka, India.
2Resident, Department of Ear, Nose and Throat, Adichunchanagiri Institute of Medical Sciences, B.G Nagara, Mandya District, Karnataka, India.
3Resident, Department of Ear, Nose and Throat, Adichunchanagiri Institute of Medical Sciences, B.G Nagara, Mandya District, Karnataka, India.
4Assistant Professor, Department of Ear, Nose and Throat, Adichunchanagiri Institute of Medical Sciences, B.G Nagara, Mandya District, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vinay S Bhat, Room No 11, Kalpataru Bhavan, AIMS Campus, B.G Nagara, Nagamangala Taluk, Mandya District, Karnataka, India. Phone : 8495945704,
E-mail: drvinaybhat@gmail.com
Aim: To ascertain a definitive treatment modality for a frequently recurring condition, pseudocyst of pinna in the form of deroofing and compression.
Materials and Methods: Thirty patients were diagnosed with pseudocyst of pinna from July 2011 to March 2013. All 30 patients underwent surgical deroofing of the pseudocyst along with compression by buttoning. The patients were followed up for a period of six months
Results: No recurrence was seen in 29 patients in the follow up period of six months (96.7%). One patient had recurrence 15 d following the procedure. The recurrence in the case could be attributed to the usage of improper buttons for compression.
Conclusion: Despite numerous treatment options for pseudocyst of pinna, there remains high recurrence rate in patients. Additionally, some treatments carry the risk of cartilage damage or visible distortion of the auricle. Surgical deroofing followed by compression using buttons can be considered as first line treatment of this entity as it is associated with very less rate of recurrence and gives a cosmetically acceptable result.
Auricle, Deroofing, Pseudocyst
Introduction
First reported by Hartmann in 1846 and first described in English literature by Engel in 1966, pseudocyst of the auricle is a benign, idiopathic, painless, spontaneous dome shaped cystic swelling on the anterior surface of the auricle [1-3]. Common sites are cymba concha [Table/Fig-1] scaphoid fossa and triangular fossa [Table/Fig-2,3] [4]. Size varies from 1 to 5 cm. It is predominantly found in males [5]. Right sided predominance is common [6]. It is also named endochondral pseudo cyst, intracartilaginous cyst and benign idiopathic cystic chondromalacia [7].
Histologically, it is an intracartilaginous cyst devoid of an epithelial lining(hence named pseudocyst). It contains straw or yellow coloured, viscous, albumin containing fluid with osmolarity, glucose and protein concentration similar to that of plasma [8].
It is a difficult condition to treat medically or surgically and a large number of treatment modalities have been described in the literature. Definitive treatment still remains controversial. Goal of the treatment should be to preserve or restore the normal architecture of the auricle with no recurrence [8] Surgical deroofing first described by Choi and modified by Lim using buttoning as a compression method has resulted in the significant decrease in recurrence rates with good cosmetic outcome in all patients [4]. Aim of our study was to prove the effectiveness of surgical deroofing with buttoning as a standard approach to treat this condition.
Materials and Methods
Thirty patients with clinical diagnosis of pseudocyst of pinna [Table/Fig-3] from July 2011 to March 2013 were included in this study. All 30 patients underwent surgical deroofing of the pseudocyst along with compression by buttoning. The patients were followed up for a period of six months.
Surgical Procedure
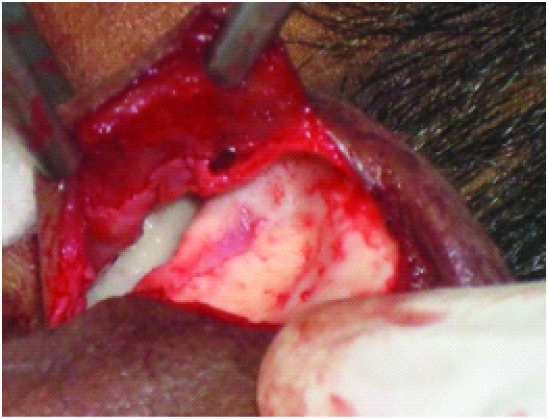
The procedure was performed under local anaesthesia using 2% xylocaine with 1:200 000 adrenaline. The entire pinna was anesthetized by infiltrating along the postauricular sulcus, the root of the helix, and the external auditory canal. A helical incision is made [Table/Fig-4] and the skin flap is elevated well beyond the anterior cartilage segment and the anterior wall of the cyst is excised along the margin with release of the straw coloured fluid [Table/Fig-5] . Curettage of the posterior wall of the pseudocyst is then done to remove any soft tissue debris. Two sterilized shirt buttons of appropriate size are then sutured on the anterior and posterior surfaces of the auricle using a 2/0 silk suture on a straight needle so as to compress the raised skin flap on to the cartilage [Table/Fig-6]. No external dressing is required. Postoperatively, antibiotics with anti-inflammatory drugs are given for one week. The sutures and the buttons are removed after one week.
Results
Thirty patients were diagnosed to have pseudocyst of the pinna from July 2011 to March 2013.The age distribution in our study ranged from 35 y to 50 y [Table/Fig-7]. Male preponderance of 96.7 % was seen [Table/Fig-8]. Right sided lesion (57%) was more common than the left (43%) [Table/Fig-9]. The lesion was seen more in the scaphoid fossa (56%) followed by the triangular fossa (27%) and cymba concha (17%) [Table/Fig-10]. Surgical deroofing with buttoning was done in all the patients. They were followed after one month, three months and six months. All (96.7%) except one patient had recurrence after 15 d for whom the reason could be attributed to the improper usage of buttons. The procedure was repeated again and he had no recurrence on follow up. The inference that surgical deroofing with buttoning is a reliable technique could be substantiated in our study.
Discussion
Pseudocyst of the pinna is a rare condition occurring commonly in young adults. Common sites of occurrence of this condition include Scaphoid fossa, followed by triangular fossa, and cymba concha.
The aetiology of this condition is obscure. Several hypothesis have been put forward for its pathogenesis. A hormonal influence modulating the inflammatory process explains the male preponderance [9,10]. Engel hypothesized that abnormal release of lysosomal enzymes from local chondrocytes caused progressive dilatation and formation of an intracartilaginous cavity [2]. Another theory proposed congenital embryonic dysplasia of the auricular cartilage with reopening of residual tissue planes resulting in the pseudocyst formation [11]. Another factor postulated in pathogenesis is chronic low grade trauma leading to overproduction of glycosaminoglycans resulting in formation of microcysts which coalesce to form a large lesion or pseudocyst with elevated isoenzymes LDH-4 and LDH-5 [12].
There has been no gold standard treatment till date. Various treatment modalities like simple aspiration, intralesional corticosteroids and aspiration in combination with bolstered pressure sutures, invasive techniques like incision and drainage followed by its obliteration by curettage and inserting a small drainage tube into the cavity with a guide wire have been tried [13-17]. Sclerosing agent like Minocycline and open deroofing have also been recommended [18,19]. Recently fibrin glue as a sealer between the 2 cartilaginous leaves as a mode of treatment has been reported by Tuncer [20]. In a study conducted by Ayaz Rehman et al., 22 patients underwent deroofing and compression procedure. None of the patients in study group had recurrence [21]. Similarly Nazir A Khan et al., showed 96% efficacy of deroofing procedure in their study [22]. Most of the treatment modalities have resulted in significant rates of recurrence as seen in study conducted by Ayaz Rehman et al., [21] where significant number of patients had recurrence following aspirations and incision and drainage of pseudocyst of pinna. Surgical deroofing with compression with buttons has shown promising results with least recurrence rates.
Pseudocyst involving concha

Pseudocyst in female patient involving triangular fossa

Pseudocyst involving triangular fossa (site of incision marked)

Incision made along the margins of the pseudocyst

Exposed cartilage after excision of ant wall of pseudocyst
compression by buttoning compression by buttoning

| Age Group | Number of Patients |
| <20 | 0 |
| 21-30 | 1 |
| 31-40 | 14 |
| 41-50 | 15 |
| >50 | 0 |
| Right Side | Left Side |
| 57% | 43% |
| Sites of Involvement | % of Patients |
| Scaphoid Fossa | 56% |
| Triangular Fossa | 27% |
| Concha | 17% |
Conclusion
In our study a total of 30 patients underwent surgical deroofing and buttoning and were followed up for six months. Barring a single case of recurrence which could be attributed to improper technique of buttoning there was no recurrence in rest of the patients. This rational approach to treatment of pseudocyst has accomplished the twin objectives of complete resolution of the condition and maintenance of normal architecture with avoidance of repeated drainage, pain, perichondritis and utmost cosmetic value. It could therefore be used as a standard approach to treat this rare condition.
[1]. K Beck, “Uber Zystenbildung am Nasenfl”ugel.European Archives of Oto-Rhino-Laryngology. 1911 85(4):304-07. [Google Scholar]
[2]. D Engel, Pseudocysts of the auricle in Chinese.Archives of Otolaryngology. 1966 83(3):197-202. [Google Scholar]
[3]. Q Chen, T Zhao, X Yang, The immunological cause of auricular pseudocyst.Zhonghua er bi yan hou ke za zhi. 1999 34(4):236-37. [Google Scholar]
[4]. S Choi, K Lam, K Chan, F Ghadially, A Ng, Endochondral pseudocyst of the auricle in Chinese.Archives of Otolaryngology. 1984 110(12):792-96. [Google Scholar]
[5]. P Cohen, M Grossman, Pseudocyst of the auricle: case report and world literature review.Archives of Otolaryngology-Head & Neck Surgery 1990 116(10):1202-04. [Google Scholar]
[6]. B Tan, P Hsu, Auricular pseudocyst in the tropics: a multi-racial Singapore experience.The Journal of Laryngology & Otology. 2004 118(03):185-88. [Google Scholar]
[7]. Q Chen, Y Fei, T Zhao, D Luo, B Wu, X Yang, Research on the immunological cause of auricular pseudocyst Lin chuang er bi yan hou ke za zhiJournal of clinical otorhinolaryngology 2001 15(7):304-05. [Google Scholar]
[8]. KW Schulte, NJ Neumann, T Ruzicka, Surgical pearl: the close-fitting ear cover cast—a noninvasive treatment for pseudocyst of the ear.J Am Acad Dermatol. 2001 44(2):285-86. [Google Scholar]
[9]. T Yamamoto, A Yokoyama, T Umeda, Cytokine profile of bilateral pseudocyst of the auricle {letter}.Acta Derm Venereol. 1996 76:92-93. [Google Scholar]
[10]. E Posma, H Moes, M Heineman, M Faas, The Effect of Testosterone on Cytokine Production in the Specific and Non-specific Immune Response.American Journal of Reproductive Immunology. 2004 52(4):237-43. [Google Scholar]
[11]. J Lee, A Panarese, Endochondral pseudocyst of the auricle.Journal of clinical pathology. 1994 47(10):961-63. [Google Scholar]
[12]. H Miyamoto, M Okajima, I Takahashi, Lactate dehydrogenase isozymes in and intralesional steroid injection therapy for pseudocyst of the auricle.Int J Dermatol. 2001 40:380-84. [Google Scholar]
[13]. C Lim, Y Goh, S Chao, L Lynne, Pseudocyst of the auricle.The Laryngoscope. 2002 112(11):2033-36. [Google Scholar]
[14]. C Chang, W Kuo, C Lin, L Wang, K Ho, K Tsai, Deroofing surgical treatment for pseudocyst of the auricle.The Journal of otolaryngology. 2004 33(3):177-80. [Google Scholar]
[15]. R Hegde, S Bhargava, K Bhargava, Pseudocyst of the auricle: a new method of treatment.The Journal of Laryngology & Otology. 1996 110(08):767-69. [Google Scholar]
[16]. D Ophir, G Marshak, Needle aspiration and pressure sutures for auricular pseudocyst.Plast Reconstr Surg. 1991 87:783-84. [Google Scholar]
[17]. LX Zhu, XY Wang, New technique for treating pseudocyst of the auricle. J Laryngo Otol 1990 104:31-32. [Google Scholar]
[18]. N Oyama, M Satoh, K Iwatsuki, F Kaneko, Treatment of recurrent auricle pseudocyst with intralesional injection of minocycline: a report of two cases.Journal of the American Academy of Dermatology. 2001 45(4):554-56. [Google Scholar]
[19]. M Harder, C Zachary, Pseudocyst of the ear : Surgical treatment.J Dermatol Surg Oncol. 1993 13:585-88. [Google Scholar]
[20]. S Tuncer, Y Basterzi, R Yavuzer, Recurrent auricular pseudocyst: a new treatment recommendation with curettage and fibrin glue.Dermatol Surg. 2003 29:1080-83. [Google Scholar]
[21]. K Rehman, M Sangoo, S Hamid, A Wani, N Khan, Recurrent Pseudocyst Pinna: A Rational Approach to Treatment.International Journal of Scientific and Research Publications. 2013 3(7):1-4. [Google Scholar]
[22]. NA Khan, M ul Islam, A ur Rehman, S Ahmad, Pseudocyst of pinna and its treatment with surgical Deroofing: An experience at tertiary hospitals.J Surg Tech Case Report. 2013 5:72-77. [Google Scholar]