Introduction: Unstable inter-trochanteric fracture in the geriatric population is a common injury and is associated with poor bone quality, excessive collapse, loss of fixation, and cut-out of the lag screw, are the common problems of attempts to fix these fractures. Present study is an attempt to evaluate the functional outcome of primary cemented bipolar hemiarthroplasty in unstable inter-trochanteric fractures in elderly patients.
Materials and Methods: This prospective study included 25 cases with unstable inter-trochanteric fracture of femur between 60 -75 y of age in whom primary Cemented Bipolar hemi - arthroplasty was performed. The patients were followed up at six week, three month, six month and one year postoperatively and assessed using Harris Hip Score (HHS), Lower Extremity Functional Scale (LEFS), Visual analogue scale (VAS) for evaluation of outcome.
Results: The mean HHS score was 78.86+8.13 by the end of one year. Similarly mean LEFS score was 34.36+7.01 by the end of one year, whereas the mean pain score on VAS Scale by the year end was 1.04+1.02.
Discussion: The changes in HHS, LEFS and VAS up to six months periods are much greater which starts showing a stable trend thereafter. Fair to good scores were observed in all the patients. We compared our results with those reported by other authors and our study gave quite comparable results. We also used lower extremity function status score (LEFS) for assessment of functional ability. The purpose of its use was that while Harris Hip Score (HHS) provides information on a multitude of factors, LEFS is more patient oriented and provides the correct information about the level of activities a patient can resume post-operatively and can be offered as a self assessment tool. No significant complication except for grade I pressure sores in four patients were seen in postoperative period but they all resolved with proper nursing care by six week follow up. No patient required revision surgery.
Conclusion: The authors believe that primary cemented bipolar hemiarthroplasty for unstable inter-trochanteric fractures of femur in elderly does provide early ambulation, good functional outcome, pain free joint with minimal complications without the need for revision surgery.
Introduction
In the geriatric population, fall is the leading cause of injuries and hospital admissions [1] . Femoral neck and inter-trochanteric fractures account for over 90% of hip fractures, occurring in approximately equal proportions [2] . Given our aging population, the number of inter-trochanteric fractures is expected to increase dramatically in the next decade [2,3] . Unstable inter-trochanteric fracture in the elderly patient is associated with around 20% mortality. Intertrochanteric femur fractures comprise approximately half of all hip fractures caused by a low-energy mechanism such as a fall from standing height. Poor bone quality, Excessive collapse, loss of fixation, and cut-out of the lag screw are the common problems of attempts to fix these fractures. Some surgeons have recommended prosthetic replacement in such fractures but this has not gained widespread support [4-7] . Present study is an attempt to evaluate the functional outcome of primary cemented bipolar hemiarthroplasty in unstable inter-trochanteric fractures in elderly patients.
Materials and Methods
This prospective study included 25 fresh cases with unstable inter-trochanteric fracture of femur between 60 -75 y of age presenting to us within a week of sustaining injury. The fracture had occurred due to a fall on level surface (18 cases) and less commonly due to road traffic accident (7 cases). The study was cleared by ethical committee of the institution. Informed written consent was taken from all cases. The fracture was graded as unstable if it was Evan’s classification type III, IV, V, Reverse oblique. Patients were excluded from the study if they were found a) unfit for anesthesia, b) refusal for consent, c) age less than 60 years, d) associated fractures or polytrauma, e) head injury, f) patients with stable fractures with an intact lesser trochanter, g) bilateral Intertrochanteric fractures, h) long recumbency period before injury and i) pathological fractures. There were Evan’s type III (5 cases), type IV (9 cases), type V (11 cases) & Reverse oblique type (0 case) respectively.The degree of Osteoporosis was assessed using Singh Index for Osteoporosis. There were 3 cases of Grade I Osteoporosis, 8 cases of Grade II, 6 cases of Grade III, 7 cases of Grade IV, 1 case of Grade V & no case of Grade IV Osteoporosis respectively. Time interval between injury and surgery was 3 d to 17 d (average 6.4 d). Imaging studies like CT scan or MRI was not required in any case.
Primary Cemented Bipolar hemi - arthroplasty was performed using Moore’s Southern approach in a lateral decubitus position. The capsule of the hip joint was exposed and “H” shaped or inverted “T” shaped capsulotomy of hip joint was done. Lesser trochanter reconstruction was done as required using stainless steel wires, ethibond sutures. At times when the lesser trochanter was comminuted, the trochanter pieces were left attached to the soft tissue and the medial defect was reconstructed using a cement mantle. We used the second-generation cementing technique and cement restrictor in all cases. In the final step of fixation the stem of prosthesis was sunk up to the previously marked point on stem and the rest of the canal was filled with a cement plug to equalise of the limb length. This technique is specifically used when lesser trochanter is separate from proximal neck portion. During distal fixation cement can also be used as a filler if the medullary is very wide. Trochanter and calcar were then retightened by wire cables after the prosthesis is fixed. Greater trochanter reconstruction was done if required with Tension Band Wiring/ K-Wires/ Screws. The soft tissue sleeve of greater trochanter along with gluteus medius and vastus medialis is attached back to the shaft. Short External rotators were then sutured back to greater trochanter. Hemostasis was achieved and then the wound was closed in layers over negative suction drain. Physiotherapy was started on the first postoperative day. Patients were allowed to sit on the side of the bed or upright in a chair. They were encouraged active movement in bed but excessive adduction and internal rotation or external rotation was avoided. Moderate flexion of both hips and knees and quadriceps strengthening exercises with a pillow between the legs was recommended. Weight bearing was permitted as early as tolerated and early gait training with the help of walker was done. Patients were instructed to use only western style commode for toilet activity. Activities involving squatting and cross legged sitting were restricted for the rest of their life. Two weeks after surgery regular medications for pain were discontinued, Sutures removed and the patient was discharged to home with a walking frame (Zimmer frame). The patients were followed up at six week, three month, six month and one year post-operatively. Parameters used for assessing functional status of the patient and for assessment of pain like Harris Hip Score (HHS), Lower Extremity Functional Scale (LEFS), Visual analogue scale (VAS) were used for evaluation of outcome [8-10]. The results were analysed using SPSS version 15.0 (statistical Analysis Software) and Wilcoxon signed rank statistics. The results were analysed with the aim to study the functional outcome of intervention.
Results
The present study included 25 cases (male 14, females 11; mean age 64.92 y). All cases were followed up till the end of one year. No case was lost to follow-up. In the first week after procedure mean HHS score was 38.34+6.55 which subsequently increased up to 78.86+8.13 by the end of one year [Table/Fig-1]. Similarly LEFS score was 6.04+1.54 in the first postoperative week and subsequently it gradually increased and reached up to 34.36+7.01 by the end of one year [Table/Fig-1]. In the first postoperative week (under adjunctive use of analgesics) the pain score on VAS Scale was 5.76+1.20 which decreased subsequently and by the year end it was 1.04+1.02 [Table/Fig-1].
Discussion
Over the years osteosynthesis has been indicated as the preferable mode of treatment for stable intertrochanteric fractures and has shown promising results but high rate of mortality, complications due to recumbency in initial postoperative year render this option impractical in unstable Intertrochanteric fracture cases. Primary cemented bipolar hemiarthroplasty has emerged as a valid choice for treatment of unstable inter-trochanteric fractures and has shown promising results with fewer complications. With this background, the present study was carried out with an aim to evaluate functional outcome in cemented bipolar hemi-arthroplasty as the primary treatment choice among elderly patients with unstable Intertrochanteric fracture.
All patients were managed using primary cemented bipolar hemiarthroplasty. In the first postoperative week the mean Harris Hip Score was 38.34±6.55, thus showing restoration of some functional activity immediately after the procedure. The patients were allowed to sit within 24 h. We encouraged the patients to sit, stand and supervised assisted full weight bearing walking with walking frame (Zimmer frame) after 24 h of surgery. The patients were able to bear weight on the involved limb within a week (mean: 4.96±18.12 days). Much longer duration of time has been reported by several studies. Yi et al., [11] reported average time to ambulate and attain full weight bearing to be 21 d. The reason for this difference could be higher mean age of patients (81 y as compared to 64.92 y in present study). After three months the mean HHS scores reached to 73.97±11.46 and mean LEFS was 30.64±6.71. By this time the patient was able to walk independently with support and was able to perform almost all their routine functions with little to moderate difficulty. Pain levels were also controlled to a remarkable extent (VAS 2.24±0.88) [Table/Fig-1]. Subsequent follow-up showed a gradual improvement in all parameters (HHS, LEFS, & VAS). Although the span of activities did not increase in subsequent follow ups yet the level of difficulty in performing the function continued to decrease. The LEFS showed a marginal improvement in next six months up to finally reach at 34.36±7.01 at the end of one year. The changes in the HHS and LEFS parameters between any two consecutive follow ups were statistically significant (p<0.05) except between six month and one year follow up [Table/Fig-2]. These findings imply that about 80–90% recovery in functional status is achieved by six months though the rest of the recovery keeps on occurring for further one year.
In present study we observed that the change in (HHS), (LEFS) and (VAS) up to 6 months periods is much greater which starts showing a stable trend thereafter [Table/Fig-2]. Thus the optimum results are obtained by 6 months itself. In our study, except for three patients showing poor Harris Hip Score at six month follow-up, fair to good scores were observed in all the patients. No patient with excellent results (Harris Hip Score>90) was observed. One of the reasons might be the shorter duration of follow up in present study. The maximum Harris Hip Score attained was 84.58 which are close to excellent. It is expected that in a longer duration of follow up these scores might increase further in view of the increasing trend in Harris Hip Score at all the scheduled follow ups.
We compared our results with those reported by other authors [11-15] and our study gave quite comparable results [Table/Fig-3]. The excellent results are rare to obtain. Elmorsy et al., [14] and Sancheti et al., [12] reported only four cases with excellent results in their series of 41 and 37 cases respectively. In a study with follow up period close to our study, Kiran Kumar et al., [15] , who followed their patients up to nine months, found mean Harris Hip Score of 75 with poor results in only two cases. We observed mean Harris Hip Scores in the fair to good range in patients and poor results in only three cases.
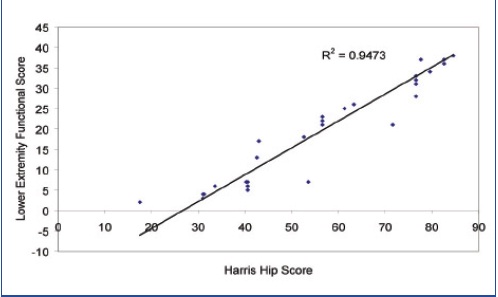
In present study, we also used lower extremity function status score (LEFS) for assessment of functional ability. On reviewing the literature, we could not find out a single study using this scale. To the best of our knowledge the present study is only one to report the use of LEFS in patients with unstable inter trochanteric fractures. The purpose of its use was that while Harris Hip Score (HHS) provides information on a multitude of factors including clinical and perceptional evaluations, while LEFS is more patient oriented and provides the correct information about the level of activities a patient can resume postoperatively. The limitation of LEFS in our study was a that none of the patients chose to respond on questions like “performing heavy activities around your home”, “walking a mile”, “running on even ground”, “running on uneven ground” and “Hopping” as being not relevant to the elderly age groups. However, despite this limitation, we found it useful as it assesses the functional ability, and gives a glimpse of the extent of improvement required to attain the functional utility. A strong correlations existed between HHS and LEFS postoperatively at different follow-up intervals (r2=0.9473) thus indicating that the two scales can be administered interchangeably [Table/Fig-4] . This finding is encouraging as it assesses the postoperative improvement of patients without using any clinical tools and can be offered as a self assessment tool.
In a study comparing between total hip replacement arthroplasty and cemented bipolar hemiarthroplasty, Walia et al., [16] reported the superiority of total hip replacement in terms of control of pain, however, they also highlighted certain drawbacks of total hip replacement arthroplasty in elderly patients such as instability, impaired reflexes, cognitive impairment, higher dislocation rates. Fan et al., [17] in their study reported bipolar hemiarthroplasty to provide comparable results with total hip arthroplasty in terms of hospitalization period, general complications, joint function, pain, rate of revision and mortality. Though the present study was not a comparative study, yet it provided promising results with achievement of remarkable functional ability and pain control. In literature, bipolar hemiarthroplasty has been shown to be similar to total hip replacement arthroplasty in terms of hospitalization period, pain severity and functional restoration [16,18] . In our opinion, given the low financial burden, possibilities of revision and overall cost-benefit situation, primary cemented bipolar arthroplasty is a viable choice giving comparable results.
In present study no significant complication except for grade I pressure sores in four patients were seen in postoperative period but they all resolved with proper nursing care by six week follow up. No patient required revision surgery. These results are similar to the results obtained by Sancheti et al., [12] who also reported only bed sore as a complication arising due to intervention. Need for revision surgery has been cited in only a few studies. Laffosse et al.,[19] reported revision surgery in only one patient. However, in a study by Elmrosy et al.,[14] both complication rates as well as revision rates were much higher. They reported need of revision surgery in four (9.8%) patients and complications such as stem loosening and subsidence, infection, dislocation, bleeding peptic ulcer and intraoperative fracture of the femur. The higher rate of complications and need for revision surgery might be dependent on skill level of the operating surgeon. In our opinion, the findings in present study suggests that primary cemented bipolar hemiarthroplasty is a good choice for unstable intertrochanteric fractures in elderly and saves time as well as cost, has no significant complications and provides sustainable functional outcomes[Table/Fig-5a-c,6a-c,7a-c], hence it should be offered as the first choice of treatment to the patient.
The limitation of present study is the short duration of follow up. There is scope for improvement in results as well as increase in complications with a longer follow up. The present study also showed that structured scales such as Lower Extremity Functional Scale can be used as efficiently as Harris Hip Score and should be used as a tool for assessment of functional status of the patient.
Harris Hip Score, LEFS and VAS at different time intervals
| Time Interval | Harris Hip Score | LEFS Score | VAVAS Score |
| Mean± SD | Mean± SD | Mean± SD |
| Postoperative | 38.34±6.55 | 6.04±1.54 | 5.76±1.02 |
| 6 week Follow up | 54.60±8.18 | 20.44±5.10 | 4.24±0.66 |
| 3 month Follow up | 73.97±11.46 | 30.64±6.71 | 2.24±0.88 |
| 6 month Follow up | 78.33±8.70 | 34.28±7.09 | 1.84±0.80 |
| 1 year Follow up | 78.86±8.13 | 34.36±7.01 | 1.04±1.02 |
Comparison of Change in Harris Hip Score, LEFS and VAS
| Time interval | Change in HHS | Change in LEFS | Change in VAVAS |
| Mean (SD) | p-value | Mean (SD) | p-value | Mean (SD) | p-value |
| Post op. – 6 week | 16.26(±3.29) | <0.001 | 14.40±3.88 | <0.001 | 1.52±0.87 | <0.001 |
| Post op. –3 month | 35.63(±5.12) | <0.001 | 24.60±5.48 | <0.001 | 3.52±0.87 | <0.001 |
| Post op. –6 month | 39.99(±3.11) | <0.001 | 28.24±5.78 | <0.001 | 3.92±1.08 | <0.001 |
| Post op –1 year | 40.52(±2.87) | <0.001 | 28.32±5.71 | <0.001 | 4.72±1.62 | <0.001 |
| 6 week – 3 month | 19.37(±4.95) | <0.001 | 10.20±2.10 | <0.001 | 2.00±0.58 | <0.001 |
| 6 week – 6 month | 23.73(±3.27) | <0.001 | 13.84±2.73 | <0.001 | 2.40±0.82 | <0.001 |
| 6 week – 1 year | 24.26(±3.73) | <0.001 | 13.92±2.61 | <0.001 | 3.20±.29 | <0.001 |
| | <0.001 | | <0.001 | | <0.001 |
| 3 month – 6 month | 4.36(±4.00) | <0.001 | 3.64±1.55 | <0.001 | 0.40±0.82 | 0.025 |
| | <0.001 | | <0.001 | | <0.001 |
| 3 month – 1 year | 4.89(±4.52) | <0.001 | 3.72±1.46 | <0.001 | 1.20±1.29 | <0.001 |
| 6 month – 1 year | 0.53(±2.66) | 0.317 | 0.08±0.40 | 0.317 | 0.80±1.00 | 0.002 |
Showing comparison of HHS in various studies
| STUDY | CASES | FOLLOW-UP (months) | HHS |
| Choy et al. | 40 | 40.5 | 80.6 |
| Sancheti et al., | 37 | 24.5 | 84.5 ± 9.72 |
| Yi et al., | 59 | 14 | 82.1 |
| Elmorsy et al., | 41 | 13.68 | 78.19 |
| Kumar K et al. | 20 | 9 | 75 |
| Singh S et al., | 25 | 12 | 78.86±8.13 |
Showing Correlation of HHS with LEFS
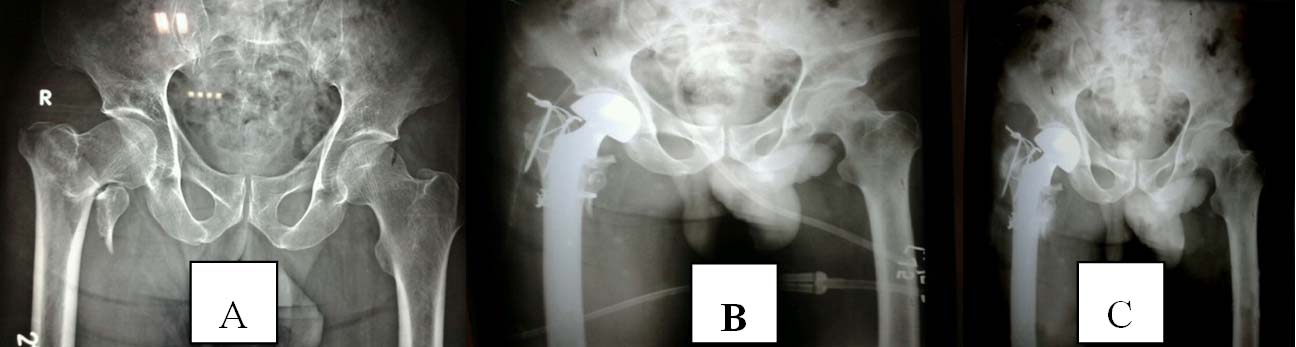
Case e.g. 1. Pre-Operative X-Ray B) Immediate Post Operative X-ray C) One Year Follow up showing union
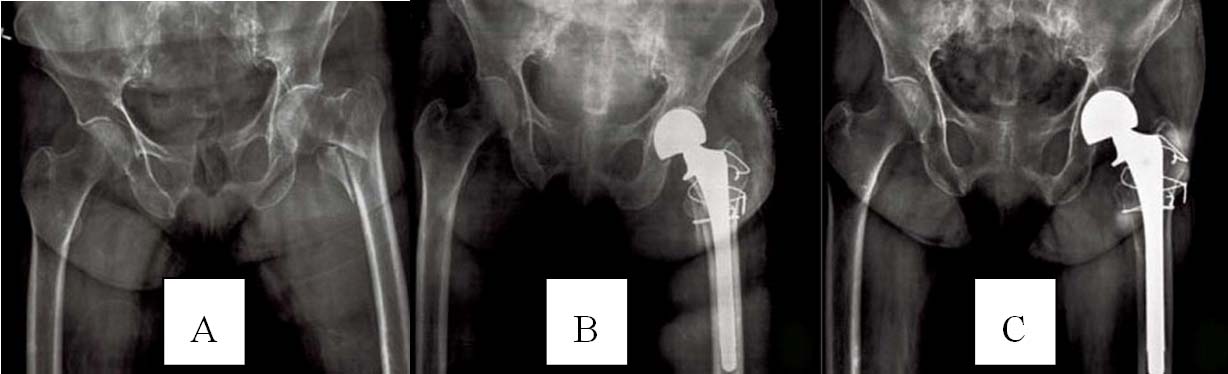
Case e.g. 2. A) Pre-Operative X-Ray B) Immediate Post Operative X-ray C) One Year Follow up showing union
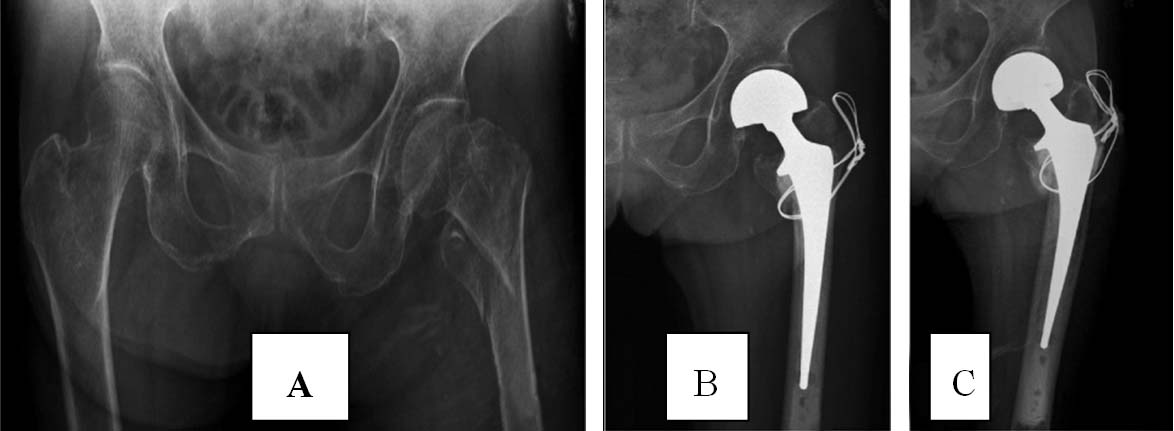
Case e.g. 3. A) Pre-Operative X-Ray B) Immediate Post Operative X-ray C) One Year Follow up showing union
Conclusion
The authors believe that primary cemented bipolar hemiarthroplasty for unstable inter-trochanteric fractures of femur in elderly does provide early ambulation, good functional outcome, pain free joint with minimal complications without the need for revision surgery
[1]. BH Alexander, FP Rivara, ME Wolfe, The cost and frequency of hospitalization for fall related injuries in older persons.Am J Public Health 1992 82:1020-23. [Google Scholar]
[2]. E Dahl, Mortality and life expectancy after hip fractures.Acta Orthop Scand. 1980 51(1):163-70. [Google Scholar]
[3]. JS Jensen, HP Golan, PJ Porter, EH Kass, Trochanteric Fractures. An Epidemiological, Clinical and Biomechanical StudyActa Orthop Scand 1981 188:11-19. [Google Scholar]
[4]. O Rodop, A Kiral, H Kaplan, I Akmaz, Primary bipolar hemiprosthesis for unstable intertrochanteric fractures. Int Orthop. 2002 26:233-37. [Google Scholar]
[5]. S Green, T Moore, F Proano, Bipolar prosthetic replacement for the management of unstable intertrochanteric hip fractures in the elderly. Clin Orthop Relat Res. 1987 224:169-77. [Google Scholar]
[6]. K Sinno, M Sakr, J Girard, H Khatib, The effectiveness of primary bipolar arthroplasty in treatment of unstable intertrochanteric fractures in elderly patients.N Am J Med Sci. 2010 2(12):561-68. [Google Scholar]
[7]. P Bonnevialle, D Saragaglia, M Ehlinger, J Tonetti, N Maisse, P Adam, French Hip and Knee Society (SFHG); Trauma Surgery Academy (GETRAUM). Trochanteric locking nail versus arthroplasty in unstable intertrochanteric fracture in patients aged over 75 years.Orthop Traumatol Surg Res. 2011 97(6 Suppl):S95-100. [Google Scholar]
[8]. WH Harris, Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation.J Bone Joint Surg Am 1969 51(4):737-55. [Google Scholar]
[9]. JM Binkley, PW Stratford, SA Lott, DL Riddle, The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther 1999 79(4):371-83. [Google Scholar]
[10]. ME Wewers, NK Lowe, A critical review of visual analogue scales in the measurement of clinical phenomena.Res Nurs Health 1990 13(4):227-36. [Google Scholar]
[11]. Z Yi, W Ze, G Zhi-yong, Treatment of Femoral Intertrochanteric Fractures With Hemi-hip Prosthesis Replacement in Elderly Patients.Journal of Occupational Health and Damage 2011 3:172-75. [Google Scholar]
[12]. KH Sancheti, PK Sancheti, AK Shyam, S Patil, Q Dhariwal, R Joshi, Primary hemiarthroplasty for unstable osteoporotic intertrochanteric fractures in the elderly: A retrospective case series.Indian J Orthop. 2010 44(4):428-34. [Google Scholar]
[13]. WS Choy, JH Ahn, JH Ko, BS Kam, DH Lee, Cementless Bipolar Hemiarthroplasty for Unstable Intertrochanteric Fractures in Elderly Patients. Clinics in Orthopedic Surgery. 2010 2:221-26. [Google Scholar]
[14]. A Elmorsy, M Saied, AA Allah, M Zaied, M Hafez, Primary Bipolar Arthroplasty in Unstable Intertrochanteric Fractures in Elderly.Open Journal of Orthopedics 2012 2:13-17. [Google Scholar]
[15]. GNK Kumar, S Meena, NV Kumar, MKV Raj, Bipolar hemiarthroplasty in unstable intertrochanteric fractures in elderly: a prospective study.J Clin Diagn Res 2013 7(8):1669-71. [Google Scholar]
[16]. JPS Walia, D Sansanwal, SK Walia, S Singh, AC Gupta, Role of primary bipolar arthroplasty or total hip arthroplasty for the treatment of intertrochanteric fracture femur in elderly.Pb Journal of Orthopaedics 2011 12(1):5-9. [Google Scholar]
[17]. L Fan, X Dang, K Wang, Comparison between Bipolar Hemiarthroplasty and Total Hip Arthroplasty for Unstable Intertrochanteric Fractures in Elderly Osteoporotic Patients.PLoS One. 2012 7(6):e39531 [Google Scholar]
[18]. RM Salunkhe, S Limaye, SK Biswas, RP Mehta, Cemented hemi-arthroplasty in proximal femoral fractures in elderly with severe osteoporosis: A case seriesMedical Journal of Dr. D.Y. Patil University 2012 5(1):36-42. [Google Scholar]
[19]. JM Laffosse, F Molinier, JL Tricoire, N Bonnevialle, P Chiron, J Puget, Cementless modular hip arthroplasty as a salvage operation for failed internal fixation of trochanteric fractures in elderly patients Acta Orthop.Belg 2007 73(6):729-36. [Google Scholar]