The clinical spectrum of alcoholic liver disease (ALD) comprises of alcoholic fatty liver disease, alcoholic hepatitis, and cirrhosis [1]. Alcoholic fatty liver disease develops in about 90% of individuals who ingests alcohol more than 60 gm/day but this is completely reversible with abstinence [2]. However, 5-15% of them develop alcoholic hepatitis who continues drinking. As many as 50% of the patients among them eventually develop state of irreversible liver damage or cirrhosis which may complicate into portal hypertension leading to upper gastrointestinal haemorrhage, ascites, splenomegaly and other stigma of chronic liver disease [1,3]. Liver function tests may show increased aspartate tansaminase (AST) to alanine transaminase (ALT) ratio in alcoholic hepatitis to altered albumin globulin ratio and increased prothrombin time (PT) in cirrhosis [1]. Histology of liver has been implicated in predicting progression of disease such as with the cessation of drinking, steatosis rapidly disappears, probably within weeks, and this is followed by a subsidence of the inflammatory changes. On the other hand large mitochondria are associated with a milder form of alcoholic hepatitis and a lower chance of transformation into cirrhosis whereas polymorphonuclear leukocytosis and perivenular cholestasis carry poor prognosis [3].
In United States, it is estimated that 14 million Americans age 18 and older meet DSM-IV criteria for alcohol abuse and/or dependence. This corresponds to a prevalence of 7.4%, higher in men (11%) than in women (4%) [4]. Excessive alcohol consumption is the third leading preventable cause of death in the United States. For every 11% increase in per capita alcohol consumption there was a 14% increase in cirrhosis among men and 8% increase among women [4]. A recent study from Bangalore reported that one-fourth of adult men consumed alcohol. Surprisingly, the study also uncovered the hidden fact that 2% of women also regularly consume alcohol [5]. There are more than 200 million alcohol users estimated in India including 1.5 million deaths due to ALD. It is estimated that the Indian Government spends nearly Rs 244 billion every year to manage the consequences attributable to alcohol use [5]. Despite the enormity of the problem in India, systematic research are lacking on this aspect. The objectives of the present study is to correlate amount and duration of alcohol intake among Indian men to various stages of ALD clinically, biochemically and histologically.
Materials and Methods
Patients: Following ethical approval, a total of 200 patients with ALD, who were admitted to medical wards of Medical College and Hospital, Kolkata, were recruited in this cross-sectional study conducted between March 2011 and February 2012. The inclusion criterion of the cases was those with the history of consumption of alcohol ≥ 60 gram per day. Patients with established liver diseases due to non-alcoholic causes and with long-standing diabetes mellitus, dyslipidaemia or malignancy were excluded from the study. The aim was to detect cases of ALD early and halt its progression to cirrhosis. The objectives of our study were to explore the distribution of different stages of ALD, to look for any relation of clinical, biochemical and histological profile of ALD patients with the quantity and duration of alcohol intake and lastly to find out any association of clinical and biochemical parameters with histological staging of liver.
Research methods
After selection of cases, following written consent careful history-taking and physical examinations were carried out in each patient. The quantity and duration of alcohol consumption were noted and liver function tests (LFT) were done. All the cases underwent percutaneous needle biopsy of liver and stained with hematoxylin and eosin (H and E), Mason’s trichrome, reticulin, and periodic acid-Schiff (PAS) stains. The specimens were analyzed blindly by two experienced histopathologists who were unaware of the patient’s clinical or biochemical profile. The liver biopsy specimens were graded using the Ishak’s modified histological activity index (HAI) score which takes components of necrosis, inflammation and fibrosis into account [6]. Severity and disease activity are expressed by necro-inflammation and is referred as ‘grade’ which is influenced by therapy. Fibrosis and parenchymal or vascular remodelling are indicators of long-term disease progression and is referred as ‘stage’ which is not influenced by therapy [6].
Statistical Analysis
Categorical variables are expressed as number of patients (with percentages) and compared across groups using ANOVA. Continuous variables are expressed as mean ± standard deviation (SD) and are compared across the groups using unpaired t test. The statistical software SPSS version 16 has been used for the analysis. P value less than 0.05 was taken as significant.
Results
A total of 224 patients were approached initially but 21 of them did not meet the eligibility criteria and 3 patients were lost to follow up. Majority (32%) of the alcoholic liver disease (ALD) patients were in the age group of 40-49 years. All the cases studied were male. Age and sex were not seen to be correlated with quantity and duration of alcohol consumption. Majority of the patients consumed 81-90 grams (30%) of alcohol per day for duration of 9-12 years (32%). Intake of poor quality country liquor was noted among the study group. In our study histopathology confirmed fatty liver, hepatitis and cirrhosis cases in 18%, 30%, and 52% of ALD patients respectively [Table/Fig-1]. Anorexia was most common symptom and jaundice was the most common finding noted among the cases. Pattern of alcohol intake, clinical feature and liver function tests of ALD patients are described in [Table/Fig-2]. Clinical features like upper gastrointestinal bleeding, pedal swelling, ascites, heaptosplenomegaly and biochemical profile such as serum bilirubin, aspartate transaminase (AST), alanine aspartate (ALT), albumin, globulin, prothrombin time (PT) were significantly related to quantity as well as duration of alcohol [Table/Fig-3]. Significant correlations were noted with anorexia, hematemesis, melena, pedal oedema, ascites, jaundice, hepatosplenomegaly and signs of liver failure to histological profile (HAI stage) of alcoholic liver disease [Table 3]. There was a significant (p < 0.05 in ANOVA) correlation between HAI stages of ALD with duration as well as quantity of alcohol consumption [Table/Fig-4].
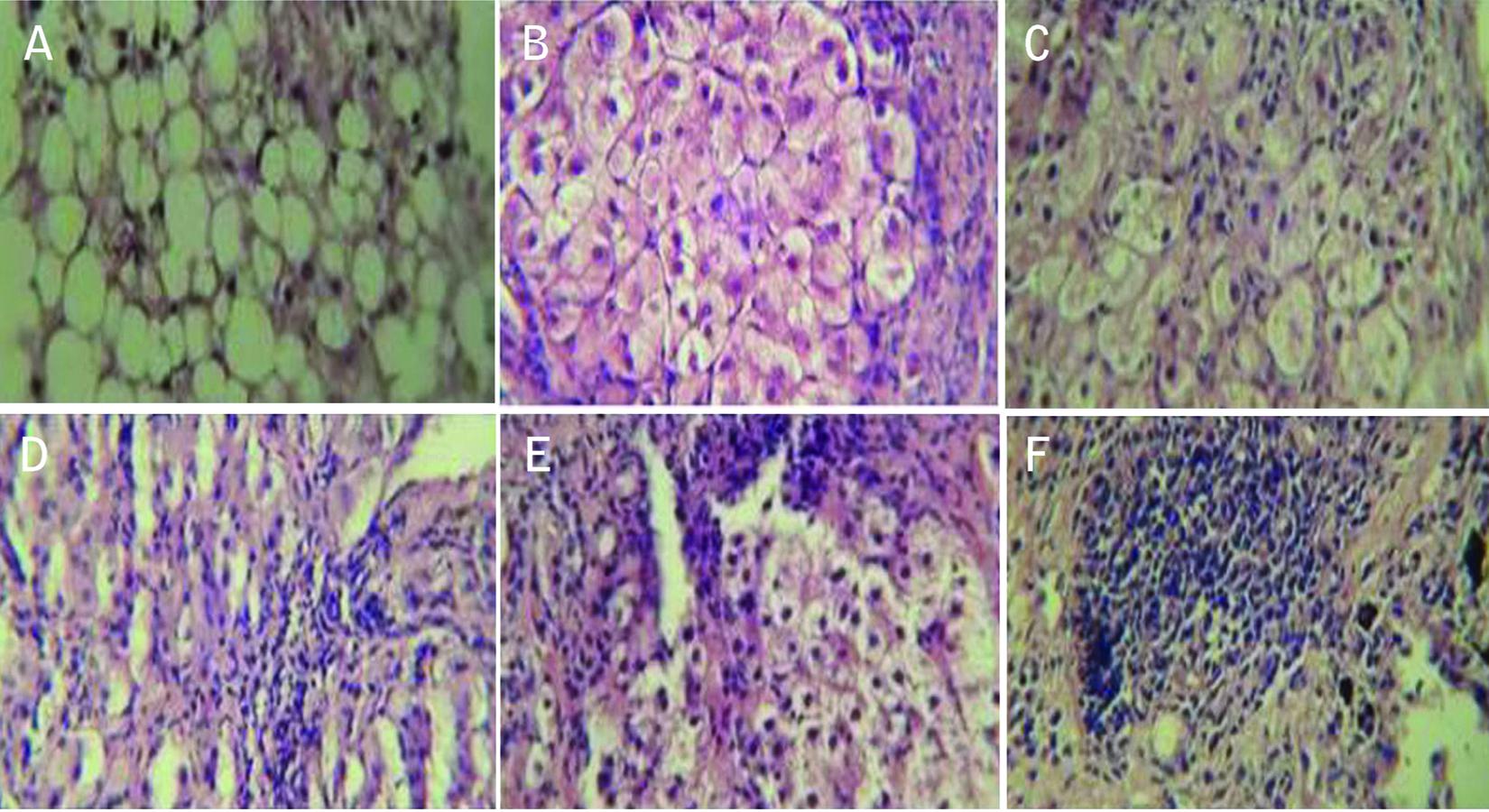
(A) Liver biopsy specimen showing moderate macrovesicular fatty changes (Hematoxylin and eosin, X 400), (B) High power view of liver tissue with alcoholic steatohepatitis showing a large cluster of hepatocytes with striking ballooning degeneration and inflammatory infiltrate in adjacent area. (H and E, X 400); (C) High power view showing ballooning degeneration of hepatocytes on left side with inflammatory infiltrate in the right side. (H and E, X 400); (D, E) Hepatic parenchyma with dense inflammatory infiltrate suggesting severe degree of chronic hepatitis with dense chronic inflammatory infiltrate (H and E, X 400); (F) High power view showing cirrhotic nodules separated by dense band of fibrosis (H and E, X 400)
Pattern of alcohol intake, clinical feature and liver function tests of alcoholic liver disease patients
| Parameters | Fatty liver (n=36) | Alcoholic hepatitis (n=60) | Cirrhosis (n=104) |
|---|
| Alcohol consumption |
| Quantity (in grams) of alcohol intake (Mean ±SD) | 60.25 ± 1.11 | 75.62 ± 11.5 | 144.0 ± 50.37 |
| Duration (years) of alcohol intake (Mean ±SD) | 12.8 ± 3.17 | 13.8 ± 4.4 | 17.6 ± 4.5 |
| Clinical features |
| Anorexia (%) | 4 (11%) | 52 (87%) | 104 (100%) |
| Abdominal pain (%) | 4 (11%) | 36 (60%) | 40 (38%) |
| Fever (%) | 0 (0%) | 32 (53%) | 24 (23%) |
| Upper gastrointestinal hemorrhage (%) | 0 (0%) | 0 (0%) | 60 (61%) |
| Pedal edema (%) | 0 (0%) | 0 (0%) | 64 (61%) |
| Ascites (%) | 0 (0%) | 0 (0%) | 88 (85%) |
| Jaundice (%) | 20 (55%) | 36 (60%) | 84 (81%) |
| Hepatomegaly (%) | 36 (100%) | 60 (100%) | 12 (12%) |
| Splenomegaly (%) | 0 (0%) | 8 (13%) | 96 (92%) |
| Signs of liver failure (%) | 0 (0%) | 0 (0%) | 32 (30%) |
| Liver function tests |
| Bilirubin >2 mg/dl (%) | 0 (0%) | 40 (67%) | 96 (92%) |
| AST >50 IU/L (%) | 9 (25%) | 60 (100%) | 24 (23%) |
| ALT > 50 IU/L (%) | 0 (0%) | 32 (53%) | 4 (3%) |
| ALP >350 IU/L (%) | 0 (0%) | 20 (33%) | 10 (10%) |
| Albumin <3 gram/dl (%) | 0 (0%) | 40 (67%) | 96 (92%) |
| Globulin > 3.5 gram/ dl (%) | 0 (0%) | 30 (50%) | 62 (60%) |
| Increased PT >3 seconds (%) | 0 (0%) | 22 (37%) | 83 (80%) |
Relationship of clinical and biochemical parameters of alcoholic liver disease with respect to duration and quantity of alcohol intake
| Duration of alcohol intake | Quantity of alcohol intake |
|---|
| <10 Years (n=68 | 10-15 years (n=80) | >15 Years (n=52) | p- value | <60 gram/ day (n=24) | 60-90 gram/ day (n=140) | >90 gram/ day (n=36) | p-value |
|---|
| Clinical parameters |
| Anorexia (%) | 40 (59%) | 72 (90%) | 48 (92%) | 0.02 | 8 (33%) | 116 (83%) | 36 (100%) | <0.01 |
| Abdominal pain (%) | 20 (29%) | 36 (45%) | 24 (46%) | 0.54 | 0 (0.0 %) | 60 (43%) | 20 (55%) | 0.08 |
| Fever (%) | 0 (0%) | 32 (40%) | 24 (46%) | <0.01 | 0 (0%) | 36 (26%) | 20 (55%) | 0.06 |
| Hematemesis Malaena (%) | 0 (0%) | 32 (40%) | 28 (54%) | <0.01 | 0 (0%) | 36 (26%) | 24 (67%) | 0.01 |
| Pedal oedema (%) | 0 (0%) | 36 (45%) | 28 (54%) | <0.01 | 0 (0%) | 40 (29%) | 24 (67%) | 0.01 |
| Ascites (%) | 4 (6%) | 48 (60%) | 36 (70%) | 0.001 | 0 (0%) | 64 (46%) | 24 (67%) | 0.03 |
| Jaundice(%) | 36 (53%) | 56 (70%) | 48 (92%) | <0.01 | 12 (50%) | 96 (69%) | 32 (89%) | <0.01 |
| Hepatomegaly (%) | 64 (94%) | 32 (40%) | 12 (23%) | <0.001 | 24 (100%) | 80 (57%) | 4 (11%) | <0.01 |
| Splenomegaly (%) | 4 6%) | 56 (70%) | 44 (85%) | <0.001 | 0 (0%) | 72 (51%) | 32 (89%) | <0.01 |
| Signs of Liver failure (%) | 0 (0%) | 20 (25%) | 12 (23%) | 0.08 | 0 (0%) | 20 (14%) | 12 (33%) | 1.19 |
| Parameters of liver function test (mean ± SD) |
| Bilirubin | 1.16 ± 0.31 | 2.17 ± 0.35 | 4.48 ± 2.34 | <0.001 | 0.80 ± 0.13 | 1.98 ± 0.55 | 5.23 ± 2.48 | <0.001 |
| AST | 55.12 ± 17.11 | 100.95 ± 10.76 | 193.92 ± 94.92 | <0.001 | 36.50 ± 7.94 | 91.74 ± 21.44 | 227.44 ± 96.69 | <0.001 |
| ALT | 31.71 ± 7.42 | 49.80 ± 5.26 | 96.38 ± 38.02 | <0.001 | 23.83 ± 4.92 | 47.06 ± 10.01 | 110.84 ± 37.25 | <0.001 |
| ALP | 318.59 ±142.65 | 327.10 ± 72.08 | 330.31 ±133.21 | 0.95 | 294.33 ± 141.52 | 333 ± 106.47 | 314.56 ±133.98 | 0.72 |
| Albumin | 3.05 ± 0.50 | 2.89 ± 0.46 | 2.42 ± 0.56 | <0.001 | 3.18 ± 0.41 | 2.91 ± 0.51 | 2.21 ± 0.30 | <0.001 |
| Globulin | 3.59 ± 0.20 | 3.61 ± 0.24 | 4.77 ± 1.03 | <0.001 | 3.48 ± 0.41 | 3.59 ± 0.23 | 5.41 ± 0.27 | <0.001 |
| PT | 13.46 ±1.98 | 14.91 ± 1.59 | 18.08 ± 1.93 | <0.001 | 11.67 ± 0.52 | 14.86 ± 1.62 | 19.11 ± 1.05 | <0.001 |
Relationship of alcohol intake and clinical features of alcoholic liver diseases with respect to liver histology
| Ishak’s modified HAI staging |
|---|
| Parameter | 0 (n=28) | 1 (n=8) | 2 (n=16) | 3 (n=20) | 4 (n=24) | 5 (n=48) | 6 (n=56) | P-value |
|---|
| Duration of alcohol intake |
| <10 years (%) | 24 (86%) | 8 (100%) | 12 (75%) | 8 (40%) | 6 (25%) | 6( 12%) | 4 (7%) | <0.001 |
| 10-15 years (%) | 4 (14%) | 0 (0%) | 4 (25%) | 4 (20%) | 16 (67%) | 24 (50%) | 28 (50%) | <0.001 |
| >15years (%) | 0 (14%) | 0 (0%) | 0 (0%) | 8 (40%) | 2 (8%) | 18 (37%) | 24 (43%) | <0.001 |
| Quantity of alcohol intake |
| <60 gram (%) | 16 (57%) | 0 (0%) | 8 (50%) | 0 (0%) | 0(0%) | 0 (0%) | 0 (0%) | <0.001 |
| 60-90 grams (%) | 12 (43%) | 8 (100%) | 8 (50%) | 20 (100%) | 24 (100%) | 28 (58%) | 28 (50%) | <0.001 |
| >90 grams (%) | 0 (0%) | 0 (0%) | 0 | 0 (0%) | 0 (0%) | 20 (42%) | 28 (50%) | <0.001 |
| Clinical features |
| Anorexia (%) | 0 (0%) | 4 (50%) | 8 (50%) | 20 (100%) | 24 (100%) | 48 (100%) | 56 (100%) | <0.001 |
| Abdominal pain (%) | 0 (0%) | 4 (50%) | 4 (25%) | 16 (80%) | 16 (67%) | 20 (42%) | 20 (36%) | 0.001 |
| Fever (%) | 0 (14.3) | 0 (50%) | 8 (50%) | 12 (60%) | 12 (50%) | 8 (17%) | 16 (29%) | 0.25 |
| Upper gastrointestinal haemorrhage (%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 24 (50%) | 36 (64%) | <0.001 |
| Pedal oedema (%) | 0 (0%) | 0(0%) | 0 (0%) | 0 (0%) | 0 (0%) | 24 (50%) | 40 (71%) | <0.001 |
| Ascites (%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 44 (73%) | 44(79%) | <0.001 |
| Jaundice (%) | 16 (14.3%) | 4 (50%) | 4 (25%) | 16 (80%) | 16 (67%) | 48 (92%) | 36(64%) | <0.01 |
| Hepatomegaly (%) | 28 (100%) | 8 (100%) | 16 (100%) | 20 (100%) | 24 (100%) | 12 (25%) | 0(0%) | <0.001 |
| Splenomegaly (%) | 0 (0%) | 0 (0%) | 4 (25%) | 0 (0%) | 4 (17%) | 48 (100%) | 48 (86%) | <0.001 |
| Signs of Liver failure (%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 32 (57%) | <0.001 |
| Parameters of liver function test |
| Bilirubin >2 mg/ dl (%) | 0 (0%) | 0 (0%) | 10 (62%) | 12 (60%) | 18 (75%) | 40 (83%) | 56 (100%) | <0.001 |
| AST >50 IU/L (%) | 3 (11%) | 6 (75%) | 16 (100%) | 20 (100%) | 24 (100%) | 12 (25%) | 12 (21%) | <0.001 |
| ALT >50 IU/L (%) | 0 (0%) | 0 (0%) | 0 (0%) | 12 (100%) | 20 (83%) | 2 (4%) | 2 (3%) | <0.001 |
| ALP 350>IU/ L (%) | 0 (0%) | 0 (0%) | 5 (31%) | 6 (30%) | 9 (37%) | 8 (17%) | 2 (3%) | 0.25 |
| Albumin <3 gram/ dl (%) | 0 (0%) | 0 (0%) | 8 (50%) | 10 (50%) | 22 (92%) | 44 (92%) | 52 (93%) | <0.001 |
| Globulin >3.5 gram/ dl (%) | 0 (0%) | 0 (0%) | 8 (50%) | 10 (50%) | 12 (50%) | 30 (62%) | 32 (57%) | <0.001 |
| PT >3 seconds than control (%) | 0 (0%) | 0 (0%) | 6 (37%) | 8 (40%) | 8 (33%) | 38 (79%) | 45 (80%) | <0.001 |
Discussion
Alcoholic liver disease (ALD) is one of the leading causes of morbidity and mortality associated with alcohol ingestion in developed as well as developing countries. In the present study, majority of the patients with ALD were in the age group of 40-49 years of age which corroborates with the study of Amarapurkar et al., [7] and Beckett et al., [8]. In the present study all the cases were male. This is contrary to the study by Amarapurkar et al., [7], in which female comprises of 6% of patients using alcohol. Morgan et al., [9] in their study of sex related differences among 100 patients with ALD showed that females comprised 23% of the patients using alcohol. In India, especially in West Bengal, alcohol intake is considered as a social stigma among women and that probably is reflected in our study subjects.
Average amount and duration of alcohol consumption were noted to be 81-90 gram per day for 9-12 years in our study. Morgan et al., [9] in their study revealed that mean duration of alcohol intake was 20.4 years in men and 16.8 years in women. Sorensen et al., [10] conducted a prospective study on 258 alcohol abusing men which showed that mean duration of alcohol consumption was 10-13 years. Leiber et al., [11] in their study among 100 patients using alcohol, the average amount of alcohol intake was found to be 90-180 gram/ day. In Bangalore study, it has been found that nearly three fourths of the consumers had been using alcohol for more than 5 years, were frequent users and were using spirits with high alcohol content [5]. In a recent study from eastern India, out of the 28 patients investigated, 57% revealed stigmata of chronic liver disease and they gave a history of 150 to 200 ml alcohol intake for more than ten years [12].
The wide prevalence of ALD including cirrhosis among Indian males was noted with significantly lower quantity and duration of alcohol ingestion. This is probably because of difference in pharmacodynamics of alcohol metabolism seen among Indians. Sarin et al., [13] showed that intake of poor quality country liquor was quite common (60%) among patients of alcoholic liver disease, but its use was not found to be associated with more severe liver injury as compared with the use of foreign liquor. In a similar study from Mumbai, Narawane et al., [14] found that liver disease was more common in those who consumed illicitly-brewed as compared to licit liquor. Daily drinking, volume of consumption > 200 ml/day, and duration of drinking > 14 years were each significantly more common in patients with cirrhosis.
Anorexia was noted as the most common symptom in our study. This study corroborates with the clinical findings of Medenhall et al., [15] except that hepatic encephalopathy was noted in 27% of the patients in that study whereas we did not have a single patient of hepatic encephalopathy. Haemetemesis or melena is reported in 30% of total ALD patients in our study and all of them had cirrhosis in liver histology. Medenhall et al., [15] found hematemesis and melena in 57% of ALD patient in their study and all of them had cirrhosis. Hislop et al., [16] observed that gastro-oesophageal varices accounted for 40% of instances of upper gastrointestinal bleeding and the mortality resulted from upper gastrointestinal bleeding was 17%.
Jaundice and hepatomegaly were found to be the most commonly observed clinical findings. In the study of Leiber et al., [11] jaundice was seen in 35% of patients with fatty liver, 60% patients with alcoholic hepatitis and 81% with cirrhosis which is similar to the finding in this study. Hepatomegaly was present in 75%, 95% and 67% in fatty liver, hepatitis and cirrhosis respectively. In our study ascites was found in 44% of cases and all of them were cirrhotic patients. In Leiber’s study [11] ascites was present in 87% patients with cirrhosis but none of the patients with fatty liver and hepatitis. In the present study, splenomegaly was present in 8% patients of alcoholic hepatitis and 92% patients of cirrhosis which nearly approaches the figures found in the study by Medenhall et al., [15] Hyperbilirubinaemia was present in 68% of ALD patients in our study. Medenhall’s [15] study found elevated levels of bilirubin in 65% of hepatitis and 90% of cirrhosis patients. In Leiber’s [11] study elevated level of ALT were noted in 50%, 95% and 50% cases of fatty liver, hepatitis and cirrhosis respectively which differs from the findings in our study. Matloff et al., [17] in their study showed ratio of AST / ALT greater than 2 is highly suggestive of alcoholic hepatitis. ALP was raised in 15% patients in our study. In the study of Medenhall et al., [15] ALP was raised in 67% of alcoholic hepatitis patient. In this study hypoalbuminaemia and hyperglobulinaemia were observed in 68% and 46% cases of ALD respectively. In the study of Leiber et al., [11] hypoalbuminaemia and hyperglobulinaemia were present in 50% and 62% of ALD patients. PT was raised (3 seconds more than control) in half of the cases in our study and most of them were cirrhotic patients. In the study by Medenhall et al., [15] PT was raised in 65% of patients with hepatitis and 90% patients with cirrhosis. In the study from Kolkata, 46% patients revealed a high degree of biochemical abnormalities [12].
In our study clinical features and biochemical changes are found to be significantly correlated with HAI stages of ALD. However, Bode et al., [18] concluded that symptoms and clinical and biochemical findings did not help in differentiating between hepatitis without cirrhotic change and cirrhosis. Majority of the patients of ALD were found to be either cirrhotic in our study. That can be explained by the fact that only patients admitted to our hospital was selected for the study and large number of patients with other spectrum of ALD were being treated from out-patient department. In one study by Amarapurkar et al., [7], the histopathological study of liver among patients using alcohol showed that 15% had normal liver, 40% had fatty change 15% had alcoholic hepatitis and 10% had cirrhosis and the rest 20% had other causes like viral hepatitis, drug induced hepatitis. One study suggested that features of tender hepatomegaly when taken along with biochemical features of hepatitis tend to demonstrate a better correlation with features of steatohepatitis [12].
Our study showed that severity of liver disease is significantly correlated with the amount and duration of alcohol intake. Amarapurkar et al., [7] noted that fatty liver developed in majority of the individuals who consume alcohol more than 60 gram per day. Medenhall et al., [15] in their study showed that alcoholic hepatitis was seen in those individuals who consumed 160 grams of alcohol per day for an average of 9 years. According to Lelbach et al., [19] cirrhosis developed in individuals who consumed alcohol 190 gram per day for 10 years. In the study from Kolkata, regression analysis showed that only abdominal parameters and not biochemical measures were able to predict the severity of histological abnormality in any given case of alcoholic liver disease [12]. Another study from North India also concluded similar correlations [20]. In the study conducted in Mumbai [14] among 327 patients that were followed up, 41% had cirrhosis while the remaining 31% had non-cirrhotic liver disease. However, this study also did not utilize liver biopsy for confirming the diagnosis in the patients. In 1995, Teli et al., [21] published data demonstrating that patients with alcoholic fatty liver and alcoholic cirrhosis had 10% and 70% risk of progressing to cirrhosis in those who continued to drink alcohol. However, in 10% of patients, the changes associated with alcoholic hepatitis can be reversed and the liver function normalized with complete cessation of alcohol intake.
Conclusion
To conclude, there are controversial data regarding whether clinical features of alcoholic liver disease correlates with stages of liver histology. Our study is unique in a way that we studied 200 male patients using alcohol and calculated HAI scores of their liver histology which showed significant correlations with clinical features. On the other hand the severity of liver damage – clinically and histologically was directly related to the quantity and duration of alcohol consumption. However, our study was limited by paucity of sample size, without any female cases and, not being a prospective one.