Case Report
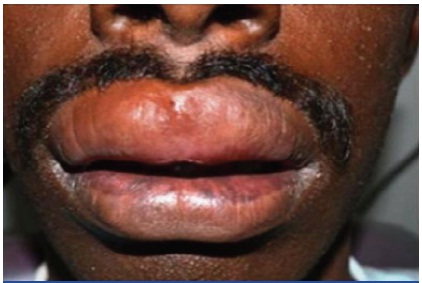
A 21-year-old male patient reported with a complaint of persistent swelling of the upper lip and gums since seven months [Table/Fig-1]. There were no associated symptoms but a sense of disfigurement persisted. The detailed medical, family and history for allergy were non contributory. The systems review particularly the Respiratory and GIT was also non contributory.
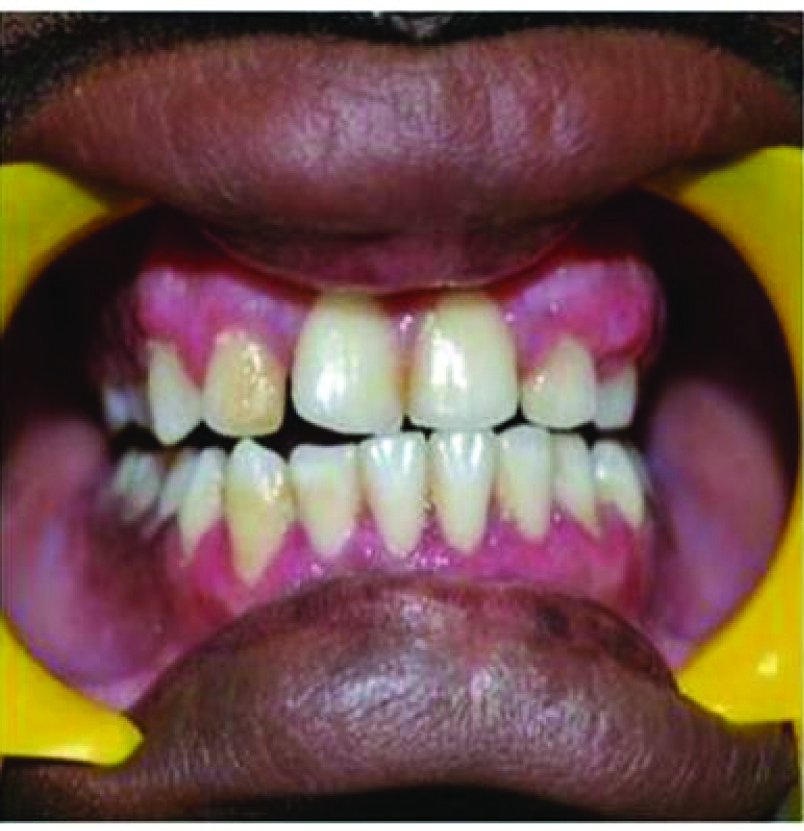
The upper lip was swollen and everted the mucosa appeared stretch and dry with no change in colour. On palpation it was soft, oedematous and non tender. Intra oral examination revealed generalized gingival enlargement [Table/Fig-2]. It was markedly evident on the facial aspect covering one fourth of the clinical crown and extending to involve the attached gingiva up to the mucogingival line. The gingiva appeared pale pink, felt fibrous and firm in consistency with no bleeding on probing.
Differential diagnosis of Angioneurotic oedema, Cheilitis granulomatosa, Cheilitis glandularis, Lymphangioma, Sarcoidosis, Tuberculosis, Orofacial granulomatosis and Crohn’s disease were considered. An empherical course of Cetirizine 10mg Bd for seven days was non beneficial.
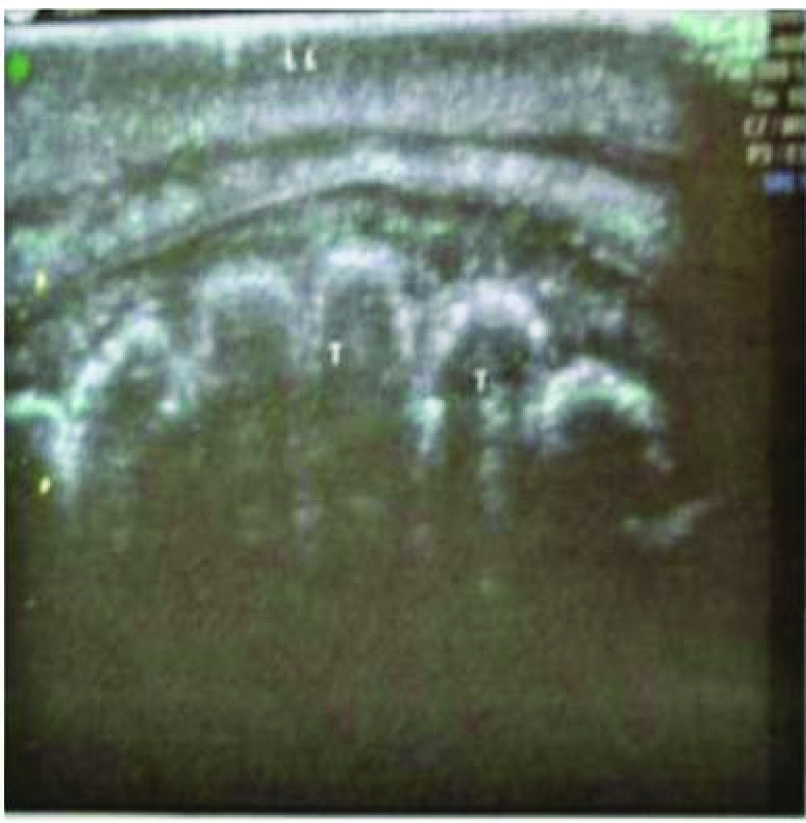
Routine blood investigations were carried out and an ultrasound of upper lip was performed to rule out cystic changes and vascular malformations [Table/Fig-3]. C1 esterase inhibitor assay obtained was 0.22g/l within normal limits (0.21-0.39) ruling out Angioneurotic oedema. A chest X-ray [Table/Fig-4], negative Mantoux test and sputum analysis for Acid Fast Bacilli (AFB) ruled out Tuberculosis. Sarcoidosis was ruled out by using angiotensin converting enzyme assay. The results obtained from the assay revealed a value of 44U/L (Normal range: 8-52U/L). Thus Sarcoidosis was ruled out. It is not recommended to subject a patient with negative Gastrointestinal (GI) symptoms to routine endoscopy, thus the possibility of Crohn’s disease was eliminated.
An incisional biopsy of the upper lip was then performed [Table/Fig-5]. Histopathology picture showed non caseating granulomas with scattered perivascular inflammatory cells [Table/Fig-6,7,8]. The clinical findings and the histopathology report identifying non-caseating granulomas suggested a diagnosis of Orofacial granulomatosis.
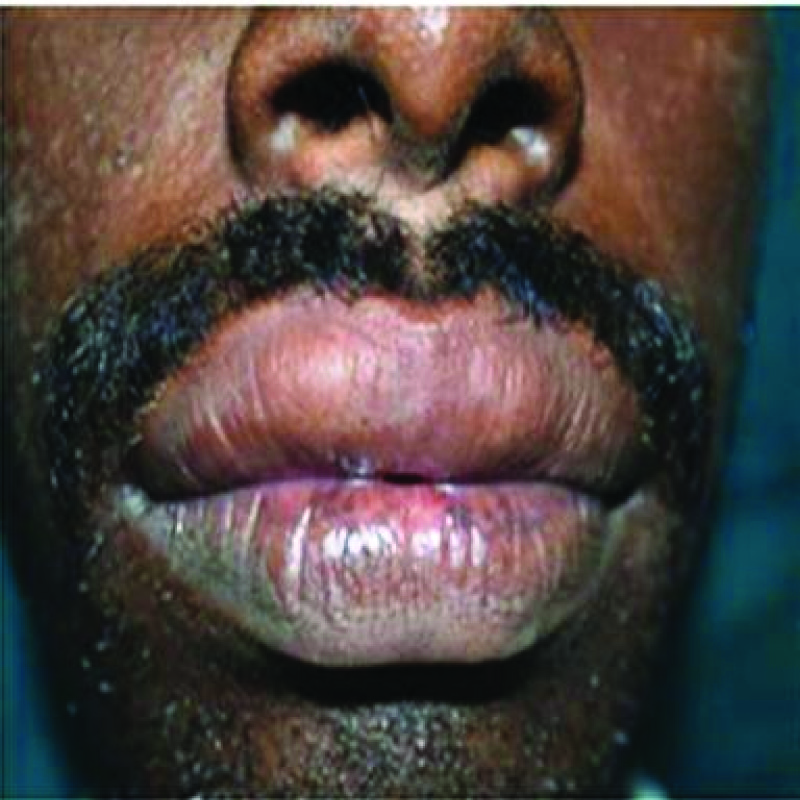
Before beginning with the management an informed consent of the patient was taken. The management protocol began with intralesional injections 0.1ml of Triamcinolone acetonide (40mg/ml) given at three equidistant points on the upper lip on the vermillion border. Care was taken to inject Triamcinolone acetonide deep into the musculature to avoid lip skin ischemia. The dose was given at an interval of three days for three weeks resulting in significant resolution of the condition [Table/Fig-9,10]. The gingival enlargement was managed by gingivectomy and gingival contouring [Table/Fig-11]. No recurrence of the lip swelling was found after eight month follow up. No fresh Gastrointestinal or Respiratory symptoms were observed.
Discussion
Orofacial granulomatosis (OFG) is a nonspecific granulomatous inflammation presenting as facial or lip swelling, cheilitis, ulcerations, gingival enlargement, mucosal tags and sometimes lymphadenopathy. Commonly it presents as a persistent or recurrent lip swelling, thus the term Cheilitis Granulomatosa (CG) [1]. CG is a monosymptomatic form of Melkersson-Rosenthal syndrome which includes CG, facial nerve palsy and fissured tongue [2]. All three components appear rarely, the most common being CG. Two major diseases may present with CG: Crohn’s disease and sarcoidosis [3]. The term Idiopathic Orofacial Granulomatosis (IOFG) is used in cases with unknown aetiology.
The term OFG introduced by Wiesenfield in 1985 is used to encompass a variety of possible conditions including Sarcoidosis and Melkersson–Rosenthal syndrome, but essentially OFG occurs mainly in isolation or as a manifestation of Crohn’s disease (CD) [4]. When the precise aetiology is unknown it is referred to as Idiopathic Orofacial Granulomatosis [5]. IOFG presents significant challenge in establishing the aetiology, management and follow up to evaluate development of Crohn’s disease at a later stage. Other aetiological factors include infections, allergy to food, food preservatives and dental materials. There is seldom any genetic relationship. However, it has been debated whether hypersensitivity to food, food additives and dental materials per se are the aetiological agents or if they are just the predisposing factors which aggravate the already existing disease.
The involvement of microbial agents in the aetiology of OFG has been suggested on the basis of implication of micro-organisms, especially bacteria, in similar chronic granulomatous conditions, such as Crohn’s disease, Sarcoidosis and tuberculosis. The available studies mainly focus on Mycobacterium tuberculosis, M. paratuberculosis, Saccharomyces cerevisiae, spirochetes and virus like measles. However, a concrete causative microbial relationship has not been associated with OFG unlike that seen in Crohn’s disease.
The inflammatory/ immunological responses as aetiological factors show a significant increase of IFN-c expression in oral lesions of OFG together with increased levels of IL-12 in most cases suggesting a predominant Th1 response. Increased levels of chemokines (RANTES⁄MIP-1a) and chemokines receptors (CCR5, CXCR3) that are linked with Th1-mediated immune response provide further evidence to the Th1 nature of the immune response in OFG [5,6]. In contrary to the hypothesis that the main allergen acts at the level of oral mucosa, instead a random influx of T cells at the site of inflammation was suggested. The profound dysregulation of the peripheral T-cell compartment suggests that OFG should be regarded as a systemic disorder with localized manifestations [7].
OFG is normally seen in the second decade of life with female predilection of approximately 56% wherein about 10% - 37% of patients with OFG have been found to have Crohn’s disease [8]. It is of paramount importance to understand the fact that oral lesions may precede the intestinal involvement in such cases. The underlying granulomatous inflammation of Crohn’s disease can involve any segment of gastrointestinal tract. An Endoscopy and biopsy from the intestinal region is essential to rule out its involvement. The intestinal manifestations might appear as late as nine years after oral lesions. Therefore, a long term follow up of these patients would be beneficial to monitor for any early changes and in case abdominal symptoms appear investigations should be carried out. Endoscopy and colorectal biopsy are justified only when signs and symptoms of gastrointestinal disturbance is evident [9-11].
Histopathological examination shows chronic inflammatory cell infiltrate, peri and paravascular aggregation of lymphocytes, plasma cells, non caseating granuloma formation with epitheloid cells and Langhans type of giant cells [10,11]. The present case fulfils most of the clinical and histopathological manifestations to consider a diagnosis of IOFG.
The treatment of OFG is challenging, with frequent recurrences despite different modalities applied. Medical management includes administration of nonsteroidal anti-inflammatory drugs, broad-spectrum antibiotics, antituberculous drugs, antilepromatous agents (clofazimine), sulfa drugs (sulfasalazine), antimalarials (hydroxycholoroquine), TNF-alpha, infliximab and steroids, be it systemic or intralesional. Surgically, cheiloplasty has shown some results, but is suggested only for resistant cases, particularly when long-lasting chronic inflammation has caused fibrosis and when it is too late to use medications. Thus, early diagnosis and treatment is mandatory for better outcome. Thalidomide has recently been shown to be effective in recalcitrant cases [12].
Among those mentioned above, corticosteroids are first-line treatments, as they are effective in reduction of the swelling. As the nature of OFG is relapsing, the use of systemic steroids has limitations because of side effects. Thus, intralesional corticosteroid injections have been suggested, wherein intralesional injection of Triamcinolone Acetonide (40mg/ml) has been proven to be effective and beneficial [12-14].
The potential side effects of corticosteroid such as temporary ischemia, hypopigmentation and soft tissue atrophy may cause cosmetic problems. Thus, the path of needle insertion should be directed orally. The expected clinical response is appropriate but not permanent, most probably requiring repeated injections in the future.
In the present case intralesional injections of 0.1 ml triamcinolone acetonide (40 mg/ml) were given into each of the three equidistant points on the border between upper lip vermillion and mucosa. The needle was inserted vertically and in order to avoid lip skin ischemia, the needle was directed slightly inwards and total volume was significantly reduced thus allowing for the usage of small thin needle which makes the procedure relatively painless [15]
The procedure was repeated every three days. Swelling was significantly resolved in three weeks. An eight month follow up did not show recurrence or development of GIT symptoms. Considering the significant role rendered by intra lesional steroids, as part of the review, the indications, contraindications, advantages, disadvantages, precautions and complications of intra lesional steroids such as triamcinolone acetonide is discussed under as follows:
Indications
• Recalcitrant and extensive lesions of Oral Lichen Planus
• Persistent lesions of Pemphigus.
• Resistant lesions of Bullous pemphigoid [16].
• Granulomatous disorders such as Orofacial granulomatosis [7]
Dermatological indications
Indications for intralesional corticosteroid therapy in dermatological lesions by virtue of their anti-inflammatory properties and their atrophogenic side effect can be used advantageously when treating hypertrophic types of lesions, including keloids, lichen simplex chronicus, hypertrophic lupus, and psoriasis [18].
Contraindications
Intralesional steroids should not be injected at the site of active skin infection e.g., impetigo (school sores) or herpes simplex (cold sores).
1. They must not be used if there is a previous history of triamcinolone hypersensitivity (allergy).
2. When large doses of triamcinolone acetonide injections are used as an alternative to oral steroids such as prednisone, they are considered to be systemic steroids. These should be avoided in patients with the following disorders-
• Active tuberculosis or systemic fungal infections
• Extensive plaque psoriasis, pustular psoriasis or erythrodermic psoriasis – systemic steroids may destabilise condition
• Active peptic ulcer disease
• Uncontrolled diabetes, heart failure or severe hypertension
• Severe depression or psychosis.
Advantage
• bypass the barrier of a thickened stratum corneum
• reduce the chance of epidermal atrophy (surface skin thinning)
• deliver higher concentrations to the site of the pathology
Complications
Complications of intralesional triamcinolone may be separated into early and delayed effects.
Early effects tend to be self-limited. They include:
• Pain, bleeding, bruising
• Infection
• Contact allergic dermatitis due to the preservative, benzyl alcohol
• Impaired wound healing
• Sterile abscess, sometimes requiring surgical drainage Delayed adverse effects include:
• Cutaneous and subcutaneous lipoatrophy (most common) appearing as skin indentations or dimples around the injection sites a few weeks after treatment, these may be permanent.
• White marks (Leukoedema) or brown marks (post inflammatory pigmentation) at the site of injection or spreading from the site of injection – these may resolve or persist long term.
• Telangiectasia, or small dilated blood vessels at the site of injection.
• Increased hair growth at the site of injection (localised hypertrichosis)
• Localised or distant steroid acne: steroids increase growth hormone, leading to increased sebum (oil) production by the sebaceous glands [19,20].
Disadvantages
• Patient discomfort, soft tissue atrophy, hypo pigmentation (cosmetic problems)
• Favorable but temporary clinical response requiring multiple repeated injections for months or even years causing relevant pain and distress in patients.
• Due to the high variability and complexity of OFG clinical behavior occasionally worst outcomes with recurrences have been reported.
Precautions
1. Numbing the lips with mental and infra orbital nerve block with 2% lignocaine to make injections painless and to inject high volume without distress suggested by Sakuntabhai, Macleod and Lawrence 1992 wherein high concentration of delayed release intra lesional triamcinolone acetonide was used which was generally well tolerated by the patient without significant pain and very low discomfort or distress.
2. Next accurate selection of precise point of needle insertion at the virtual line dividing the prolabium and labial mucosa. The needle was directed deeply towards the oral mucosa with the objective of avoiding atrophy and hypo pigmentation of labial skin.
Intralesional steroid such as triamcinolone acetonide has been chosen as the treatment option over other options and represent the corner stone of OFG therapy because they immensely contribute in reducing the swelling within 2-3 wks and preventing chronic recurrence and ultimately securing a long disease free period. This is achieved by the synergistic effect of delayed release and high concentration of the drug [21].
Clinical image shows upper lip swelling
Clinical image shows gingival enlargement

Ultrasound of upper lip reveals absence cystic spaces and vascular malformations
X-Ray reveals absence of hilar lymphadenopathy

Clinical image shows incisional biopsy of labial mucosa

Histopathological picture shows focal inflammatory areas with extravasated RBCs
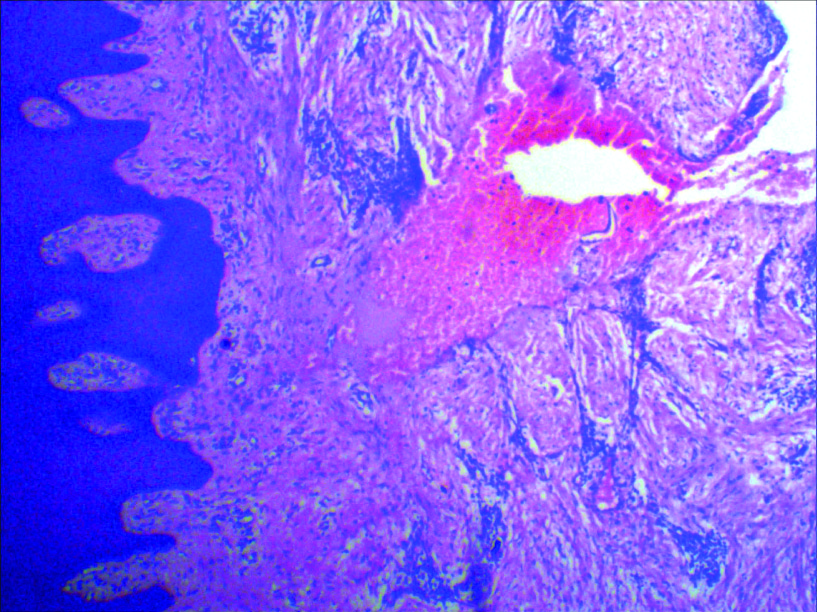
Histopathological picture shows Granulomatous areas with fibrous connective tissue

Histopathological picture shows epithelial hyperplasia with focal areas of chronic inflammatory cells

Clinical picture shows post operative facial view

Clinical picture shows resolution of lesion after treatment
Clinical picture shows post Gingivectomy
Conclusion
The diagnosis of IOFG is by exclusion supported by the histopathological evidence of chronic granulomatous inflammation. Barium meal and intestinal biopsy are not recommended to rule out Crohn’s disease without evidence of gastrointestinal manifestations. Intralesional corticosteroids are beneficial and a regular follow up and review is essential. To conclude in terms of diagnosis and management IOFG represents a challenging condition.
[1]. D Wiesenfeld, MM Ferguson, DN Mitchell, Orofacial granulomatosis – a clinical and pathological analysisQ J Med 1985 54:101-13. [Google Scholar]
[2]. G Miescher, Über essentielle granulomatöse Makrocheilie (Cheilitis Granulomatosa)Dermatologica 1945 91:57-85. [Google Scholar]
[3]. Goel Saurab, Khorate Manisha, P Nahar, J Ahmed, Cheilitis Granulomatosa - An Uncommon Clinicopathological Entity: A Case ReportJ Cancer Sci Ther 2010 2(4):086-88. [Google Scholar]
[4]. Elliott Tim, Campbell Helen, Escudier Michael, Poate Tim, Nunes Carlo, Lomer Miranda, Experience with anti-TNF-a therapy for orofacial granulomatosisJ Oral Pathol Med. 2011 40:14-19. [Google Scholar]
[5]. WM Tilakaratne, J Freysdottir, F Fortune, Orofacial granulomatosis: review on etiology and pathogenesisJ Oral Pathol Med 2008 37(4):191-95. [Google Scholar]
[6]. J Freysdottir, S Zhang, WM Tilakaratne, F Fortune, Oral biopsies from patients with orofacial granulomatosis with histology resembling Crohn’s disease have a prominent Th1 environmentInflamm Bowel Dis 2007 13(1):439-45. [Google Scholar]
[7]. A Giovannetti, F Mazzetta, A Cavani, D Pennino, E Caprini, E Ortona, Skewed T-cell receptor variable β repertoire and massive T-cell activation in idiopathic orofacial granulomatosisInt J Immunopathol Pharmacol 2012 25(2):503-11. [Google Scholar]
[8]. WM Zimmer, RS Rogers, CM Reeve, PJ Sheridan, Orofacial manifestations of – Rosenthal syndrome. A study of 42 patients and review of 220 cases from the literature.Oral Surg Oral Med Oral Pathol 1992 74:610-19. [Google Scholar]
[9]. Gingisetty Harikishan Oral Crohn’s disease without intestinal manifestationsJ Pharm Bioallied Sci 2012 4(2):S431-34. [Google Scholar]
[10]. Kim Sue Kyung, Orofacial Granulomatosis Associated with Crohn’s DiseaseAnn Dermatol 2010 22(2):203-05. [Google Scholar]
[11]. Ajith Soumya, Orofacial Granulomatosis. A Case Report.Indian J Stomatol 2012 3(2):143-45. [Google Scholar]
[12]. VG Mahima, Patil Karthikeya, Malleshi Suchetha N, A Clinico histopathologic Diagnosis of Inimitable Presentation of Orofacial GranulomatosisInternational J of Clinical Cases and Investigations 2010 1(1):13-9. [Google Scholar]
[13]. Thomas Titus K, Neelakandan RS, Bhargava Darpan, Deshpande Ashwini, Orofacial Granulomatosis: A Clinicopathologic CorrelationHead Neck Pathol 2011 5(2):133-36. [Google Scholar]
[14]. Ivan Orofacial Granulomatosis Treated with Intralesional TriamcinoloneActa Dermato venerol Croat. 2011 19(3):165-69. [Google Scholar]
[15]. Motemayel F.Ahmadi, Abdolsamadi HR, Irani S., Bardal R., Orofacial Granulomatosis of the Upper Lip: A Case ReportDJH 2009 1(1):37-40. [Google Scholar]
[16]. MD Mignona, S Fedele, L Lo Russo, L Lo Muzio, Orofacial granulomatosis with gingival onsetJ Clin Periodontol 2001 28:692-96. [Google Scholar]
[17]. Alagbeg Ivan, Rogulj Ana Andabak , Hutinec Zdenka, Orofacial granulomatosis treated with intralesional triamcenolone acetonideActa Dermatovenerol Croat 2011 19(3):165-69. [Google Scholar]
[18]. Kallali Basvaraj, Singh Kamlesh, Thaker Vidhi, Corticosteroids in dentistryJIAOMR 2011 23(2):128-31. [Google Scholar]
[19]. JJ Sciubba, N Said- Al Naief, Orofacial granulomatosis: presentation, pathology and management of 13 new casesJ Oral Pathol Med 2003 32:576-85. [Google Scholar]
[20]. RN Richards, Update on intralesional steroid: focus on dermatosesJ Cutan Med Surg 2010 :14-19. [Google Scholar]
[21]. Bolognia JL, Jorizzo JL, DermatologyElsevier Limited 2008 2nd Edition [Google Scholar]