Introduction
Gingival diseases affecting children are numerous and may progress to jeopardize the periodontium of the adult. The effects of periodontal diseases observed in adults mostly have their inception earlier in life. Dental practitioners have an important role to play in the early recognition and diagnosis of gingival and periodontal diseases to optimize treatment outcomes [1].
Anatomical Considerations
There are significant differences in the periodontal structures between childhood and adult life [2].
The width of the attached gingiva is greater in the incisor area, decreases over the cuspids, and increases again over primary molars and permanent molars. The attached gingiva increases in width with age. In addition, the contact points between deciduous teeth are not as tight as those between the permanent dentition providing favorable location for bacterial growth, thus leading to increased susceptibility of the interdental region.
Clinical and histological correlations in childhood gingiva
| Clinical Appearance | Histologic Appearance |
|---|
| Reddish in colour | Thinner epithelium, a lesser degree of cornification, and greater vascularity |
| Lack of stippling | Shorter and flatter papillae from the lamina propria. |
| Rounded and rolled gingival margins | Hyperemia and edema that accompanies eruption. Pronounced cervical ridge of the crown in deciduous teeth |
| Greater sulcular depth. The mean gingival sulcus depth for the primary dentition is 2.1 mm ± 0.2 mm. | At an early age the junctional epithelium presumably originates from the reduced enamel epithelium as a consequence of the character of its former stratum intermedium, a readiness to split up, a probe can easily be inserted deep into the marginal crevice area intruding into the tissue proper and simulating an eruption pocket. |
Tooth supporting structures and its features in childhood
| Gingiva | The connective tissue has comparatively less well-developed net of collagen fibres than in adults. The surface of the col was said to be covered by an odontogenically-derived epithelium that is atrophic, (four cell-layers thick) and has a diminished proliferative activity. The replacement of the odontogenically-derived epithelium by ingrowing oral epithelium was considered essential for a healthy periodontium. |
| Periodontal Ligament | It is wider, has fewer and less dense fibres per unit area and has increased hydration with a greater blood and lymph supply than in adults. During eruption the principal fibres are parallel to the long axis of the teeth. The bundle arrangement occurs after the teeth encounter their functional antagonists. |
| Cementum | It is often thinner and less dense than of adults. It shows a tendency to hyperplasia of cementoid apical to the epithelial attachment. Before the tooth reaches the occlusal plane, a cellular cementum is formed. |
| Alveolar Bone | The lamina dura is thinner; there are fewer trabecular and larger marrow spaces. There is a smaller amount of calcification greater blood and lymph supply and the alveolar crest appears flatter. |
The significance of these anatomical differences to the pathogenesis of periodontal disease during childhood remains to be determined. A further area of controversy the pathogenesis of periodontal disease in children is the role of interdental col described by Cohen (1959).
Physiologic Gingival Changes Associated with Tooth Eruption
During the transition period in the development of the dentition, changes associated with eruption of the permanent teeth occur in the gingiva [4].
Pre-eruption bulge: Before crown appears, gingiva presents firm bulge, slightly blanched and confirms to contour of underlying crown.
Formation of gingival margin: Marginal gingiva and sulcus develop as crown penetrates oral mucosa. In course of eruption, gingival margin is edematous, rounded, and slightly reddened.
Normal prominence of gingival margin: During the period of mixed dentition it is normal for marginal gingiva around permanent teeth to be prominent, particularly maxillary anterior region. At this stage of tooth eruption gingiva is still attached to crown, and it appears prominent when superimposed on the bulk of underlying enamel [Table/Fig-3].
Physiologic gingival changes associated with tooth eruption

Epidemiology
The prevalence of gingivitis in developed countries was about 73% among the children between 6 and 11 years of old. This rate raises with increasing in age from 6 to 11 [5].
Several studies have shown that the prevalence of gingivitis increases markedly during puberty.
During adolescence, there appears to be an increase in the prevalence of gingivitis figures varying from 50-99%.
The prevalence of gingivitis is less in girls than boys, which is probably related the levels of oral hygiene.
Classification of Gingival Diseases [
6]
A. Gingival Diseases Associated With Plaque
I. Without Local Contributing Factor
Plaque - Induced Gingivitis
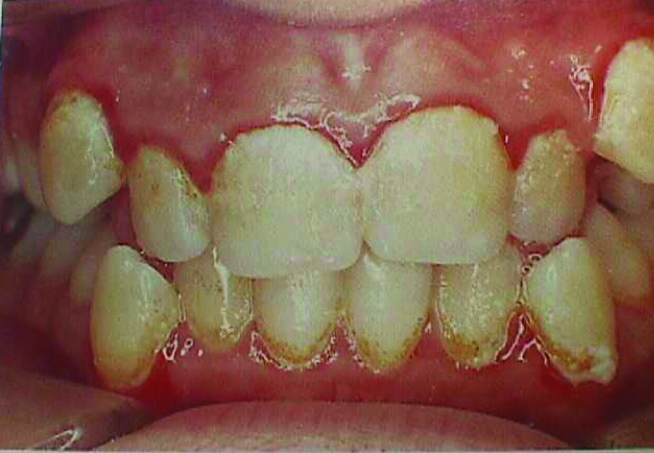
The primary cause of gingivitis is plaque. Dental plaque appears to form more rapidly in children aged 8 to 12 years than in adults [Table/Fig-4].
Plaque - induced gingivitis
Clinical Features
The plaque-induced inflammatory lesion is usually confined to the marginal aspects of the gingiva and with time, progresses to other tissues of the periodontium.
A fiery red surface discoloration is often superimposed on underlying chronic changes.
Gingival color change and swelling appear to be more common expressions of gingivitis in children than are bleeding and increased pocket depth [7].
Long term exposure can cause plaque induced gingival enlargement also [8].
The Oragranulocyte Migration rate (OMR) is low when compared with the rate in adults. The tendency to gingival bleeding, the production of crevicular fluid and leukocytes are less than in the adults [9]. The highest degree of gingival inflammation is in the 14-16-year-olds.
With Local Contributing Factor
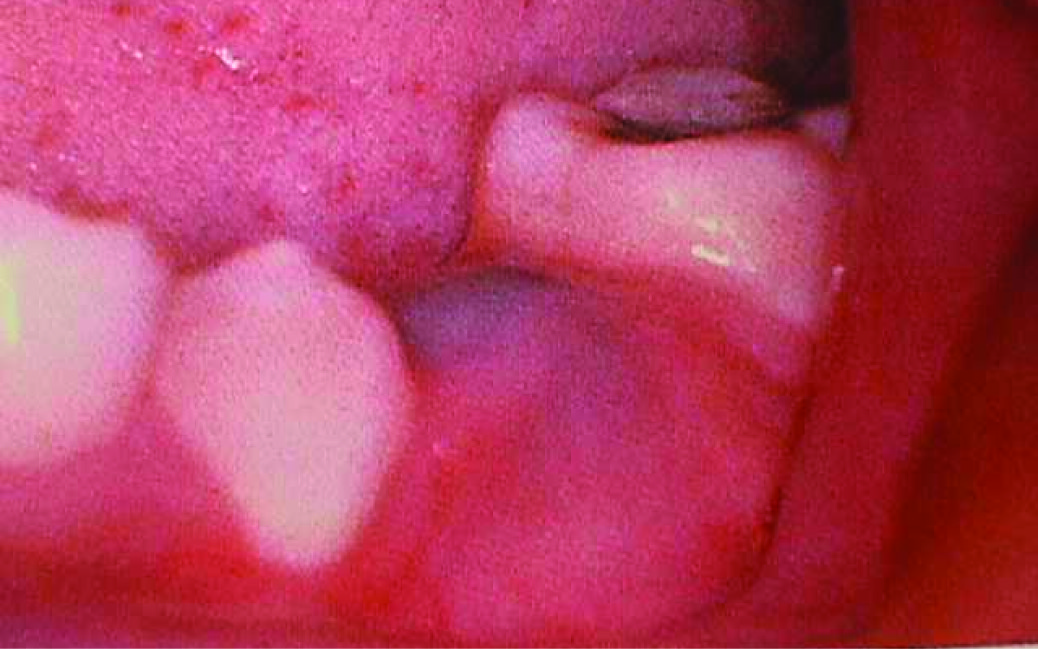
Eruption Cyst & Hematoma
It is common for erupting teeth to be associated with a form of dentigerous cyst called an eruption cyst. It is usually translucent, fluctuant and circumscribed swelling [10] [Table/Fig-5,6]. When cystic cavity contains blood, swelling appears as purple/deep-blue fluctuant, circumscribed swelling termed as eruption hematoma.

Eruption Gingivitis
Gingivitis associated with tooth eruption is frequent. However tooth eruption does not cause gingivitis. It may be caused by a greater risk of plaque accumulation in areas of shedding primary teeth and erupting permanent teeth, since oral hygiene may be difficult or even unpleasant to perform [11]. The inflammatory changes accentuate the normal prominence of the gingival margin and create the impression of a marked gingival enlargement.
Gingivitis Associated With Orthodontic Appliance
Access of interproximal tooth brushing is reduced considerably during fixed appliance therapy. The problem is compounded when teeth are banded rather than bonded. Supragingival plaque deposits are shifted into a subgingival location by tipping movement. Conversly, bodily movements are less likely to induce a relocation of supragingival plaque. Thus, gingival changes can occur within 1-2 months of appliance placement and are generally transient [12].
Other Factors
Excessive overjet and overbite, nasal obstruction, mouth breathing habit, Partially exfoliated, loose deciduous, malposed, eroded margin of partially resorbed and carious teeth can frequently cause gingivitis.
B. Gingival Diseases Modified By Systemic Factors
I. Associated With Endocrine System
Puberty Gingivitis
Enhanced levels of gingival inflammation without increased levels of plaque accumulation occur in children at puberty. The cytoplasm of gingival cells contains specific high affinity, low capacity receptors for both estrogens and testosterone. Estrogen receptors are found in the basal and spinous layers of the epithelium and in fibroblasts and endothelial cells of small vessels in the connective tissue. Thus, gingiva appears to be a target organ for some of the steroid hormones. The relationship between elevated levels of circulating sex hormones and prevalence of gingivitis in puberty is strengthened by the observation that, during adolescent, gingivitis peaks earlier in girls (11-13 years) than in boys (13-14 years) [13]. Proportions of P. intermedius correlated with levels of plasma estrogen and progesterone, and in vivo evidence is obtained indicating that these hormones are nutrients for P. intermedius [11]. Thus, it is characterized by pronounced inflammation bluish red discoloration, edema and enlargement, which result from local irritants that would ordinarily elicit a comparatively mild gingival response [14].
II. Associated With Blood Dyscrasias
Leukemia
It is a malignant disease caused by the proliferation of the WBC- forming tissues, especially those in the bone marrow. It may be acute or chronic and can affect any of the WBC – granulocytes (myeloid), lymphocytes, or monocytes. Acute types of leukemia were frequent in people under 20 years of age. Acute lymphoblastic leukemia mainly occurs in children under 10 years. Factors that have been implicated to be of etiologic significance are radiation injury, chemical injury, genetic factors – Down’s syndrome, immune deficiency and viral infections [Table/Fig-7].
Leukemia - associated Gingivitis

Clinical features
Gingiva appears as swollen, glazed, and spongy tissue which is red-deep purple in appearance with gingival bleeding.
Enlargement may appear as a diffuse enlargement of the gingival mucosa, an oversized extension of the marginal gingiva, or a discrete tumor like interproximal mass. It is moderately firm in consistency, but there is a tendency toward friability and hemorrhage, occurring either spontaneously or on slight irritation [15].
Lethargy, malaise, sore throat, fever, skin infections that fail to heal, purpura, cervical lymphadenopathy, spleenomegaly, hepatomegaly and petechiae.
III. Associated With Nutritional Deficiency
Scorbutic Gingivitis
Vitamin C deficiency causes hemorrhage, collagen degeneration and edema of the gingival connective tissue. The involvement is usually limited to the marginal tissues and papillae [16]. Gingiva is bluish, soft, and friable and has a smooth shiny surface. Hemorrhage occurring either spontaneously or slight provocation. Surface necrosis with pseudomembrane formation and necrosis occur as a result of infarcts created in the capillaries supplying the gingiva [9].
C. Modified By Medication
Drug Influenced Gingival Enlargement
Overgrowth of gingiva is a well-recognized unwanted effect of a number of drugs. The most frequently implicated are phenoytin, cyclosporine and nefidipine. Interdental papillae become nodular before enlarging more diffusely to encroach upon the labial tissues. The anterior part of the mouth most severely and frequently involved. Enlarged gingiva is pink, firm, stippled in subjects with good standard of oral hygiene. When it is refractory to long-term treatment, the patient’s physician may be requested to modify or change the anticonvulsant therapy [17] [Table/Fig-8].
Drug influenced gingival enlargement

Non Plaque Induced Gingival Diseases
A. Viral
Acute Herpetic Gingivostomatitis [Table/Fig-9]
Various characteristics of ANUG
| CausativeOrganism | Herpes simplex virus (HSV) type 1 |
| Occurance | Infants and children younger than 6 years of age, but it is also seen in adolescents and adults |
| Clinical features | Diffuse erythematous, shiny involvement of the gingiva and the adjacent oral mucosa. Varying degrees of edema, gingival bleeding, Discrete spherical gray vesicles which rupture and form painful small ulcers with a red, elevated, halo like margin and a depressed yellowish or grayish white central portion are also seen. It occurs occasionally without overt vesiculation18 |
| Recurrence | On provocation (exposure to sunlight, fever, colds, mechanical stretching of the lip) |
B. Fungal
Linear Gingival Erythema
It is characterized by 2-3mm marginal band of intense erythema in free gingiva extending to attached gingiva as focal or diffuse erythema and/or extending beyond mucogingival line into alveolar mucosa. It may be localized to one or two teeth but it is more commonly a generalized gingival condition [18] [Table/Fig-10].

Candidiasis
It occurs from an overgrowth of candida albicans, usually after a course of antibiotics or as a result of congenital or acquired immunodeficiencies [10].
C. Bacterial
Acute Necrotizing Ulcerative Gingivitis
In developing countries, the prevalence of ANUG is higher than in the industrialized countries, and the disease frequently occurs in children. In India, 54-68% of the cases occurred in children below 10 years of age [19].
Clinical Characteristics
Punched out appearance due to ulcerated and necrotic papillae and gingival margins.
Ulcers are covered by a yellowish-white or grayish slough termed psuedomembrane.
Removal of the slough results in bleeding and underlying tissue becomes exposed.
A foetor ex ore is often associated, but can vary in intensity.
Seldom associated with deep pocket formation as extensive gingival necrosis often coincides with loss of crestal alveolar bone.
The involved papillae are separated into facial and lingual portion with an interposed necrotic depression.
Swelling of lymph nodes and increased bleeding tendency are often present.
Fever and malaise is not a consistent.
The oral hygiene in these patients is usually poor [Table/Fig-11].
Acute necrotising ulcerative gingivitis

The variable flora consisted of a heterogeneous array of bacterial types although the characteristic bacterial flora of spirochetes and fusobacteria has been isolated from the necrotic lesions in several studies. Young age is one of the predisposing factors of ANUG [20].
D. Congenital Anomalies
Congenital Epulis
Congenital Epulis of newborn is a rare gingival tumour that occurs along the alveolar ridge. It is usually without associated abnormalities of the teeth or additional congenital malformations. Clinically it presents as a smooth well defined erythmatous masses arising from gum pad. Size may be large enough to lift the upper lip. The unerupted teeth are not affected usually and can be seen in MRI [21].
Congenital Gum Synechiae
It is characterized by congenital adhesions between different parts of oral cavity. It is rare type of disease. It causes difficulty in breathing and respiration soon after birth [22].
E. Trauma [Table/Fig-12]
Gingival changes due to trauma
| External trauma to the tissue, bites, tooth brush abrasion, idiopathic trauma, habits like nail biting and abrasive foods | Traumatic lesions |
|---|
| Fixed anterior margin of the acrylic plate of a removable appliance | Transient Gingival Hyperplasia |
| Chronic irritation during orthodontic treatment | Localized, acute inflammatory reaction |
| Improper brushing technique | Mucogingival defects like recession4 |
F. Gingival Diseases Associated With Heredity
Benign, non-inflammatory, familial fibrotic enlargements such as hereditary gingival fibromatosis, appears non-hemorrhagic, firm, progressing slowly upon eruption of permanent dentition [23]. But there can be an overlay of gingival inflammation which can augment the enlargement [Table/Fig-13].
Hereditary gingival fibromatosis

Hereditary gingival fibromatosis can be inherited as a simple mendelian trait, in some chromosomal disorders and as a malformation syndrome. Although the specific genes for this disease have not been identified, genetic analysis supports the presence of 2 different gene loci on chromosome 2P [24].
G. Foreign Body Reaction
Though it is not very common, it can happen during amalgam tattooing etc.
H. Gingival Manifestations Of Systemic Conditions
Gingival Lesions Associated With Chicken Pox
Varicella herpes virus primarily affects individuals under the age of 15 years. In the oral cavity small ulcers may develop in any area of the mouth, however, lesions are found most often on the palate, gingiva and buccal mucosa [18,25] [Table/Fig-14].
Ulcers associated with chicken pox

Gingival Lesions Associated With Mononucleosis
Mononucleosis is produced by the Epstein - Barr virus and is primarily a disease of children and young adults [26]. The clinical symptoms are most prominent in young adults and common signs & symptoms include fatigue, malaise, headache, fever, sore throat, enlarged tonsils, and lymphadenopathy [27,28]. Alterations in the oral cavity include gingival bleeding, petechiae of the soft palate, ulceration of the gingiva and buccal mucosa (White, 1998). Palatal petechiae are usually present before systemic symptoms become evident [29].
Soft Tissue Lesions Associated with Herpangina
The coxsackie group A viruses are associated with herpangina. Commonly seen in young children . Clinically consists of numerous small vesicles which proceed to small ulcers contained on a gray base and inflamed periphery [29]. The ulcers appear on the hard & soft palate, posterior pharyngeal wall, buccal mucosa or tongue. The ulcers are generally not painful and usually heal within a few days to a week.
Soft Tissue Lesions Associated with Hand, Foot and Mouth Disease: The majority of cases of hand, foot and mouth disease occur in children between 6 months & 5 years of age. Both coxsackie group A & B may play a role in this disease. Clinically resembles herpangina but results in difficulty in eating due to sore mouth [28]. This disease is generally self limiting and will regress in 1-2 weeks.
Wegeners Granulomatosis: It is a systemic disease that initially present with striking alterations that are confined to the gingival diseases. Classically, the gingival tissues exhibit erythema and enlargement band are typically described as Strawberry gums [29].
Kindlers Syndrome
Cutaneous neonatal bullae, poikiloderma, photosensitivity and acral atrophy are present in this condition. It may also present with oral lesions that are clinically consistent with desquamative gingivitis [29].
Conclusion
Irrelevant of age, gingival diseases have been found to occur right from children to older individuals. The common myth existing among us is that gingival diseases are pertained only to adulthood, but this review article puts forth a fact that the inception of gingival diseases could be from childhood as well. Either incomplete knowledge about gingival diseases in childhood or ignoring them would jeopardise the periodontium in adults.This article further higlights the need for patient education, parent counselling and regular pedodontic gingival examination for maintaining a healthy and hygienic oral cavity in childhood.
[1]. Clerehugh Professor Valerie, Kindelan Dr Susan, Guidelines for periodontal screening and management of children and adolescents under 18 years of ageBritish society of Periodontology and British society of Paediatric dentistry 2012 (www.bsperio.org.uk) [Google Scholar]
[2]. Bimstein Enrique, Needleman Howard L, Periodontal and gingival health and diseases 2001 United KingdomMartin Dunitz:17-30.Chapter 2, The normal gingival and periodontium [Google Scholar]
[3]. McDonald Ralph E, Avery David R., Dean Jeffrey A., Dentistry for Child and Adolescent 2004 8th edMissouriMosbyChapter 20, Gingivitis and Periodontal Diseases: p.413-452 [Google Scholar]
[4]. Newman Michael G, Takei Henri H., Carranza Fermin A., Carranza’s Clinical Periodontology 2011 11th edIndiaSaundersChapter 11, Gingival diseases in childhood: p.104-110 [Google Scholar]
[5]. Ketabi M., Tazhibi M., Mohebrasool S., The Prevalance and Risk Factors of Gingivitis Among the Children Referred to Isfahan Islamic Azad University (Khorasgan Branch) Dental School, In IranDental Research Journal Spring - Summer 2006 Vol. 3(No.1) [Google Scholar]
[6]. Ranney RR, Classification of periodontal diseasesPeriodontology 2000 1993 2(1):3-25. [Google Scholar]
[7]. Marsh PD, Dental Plaque. Biological significance of a biofilm and community life styleJ Clin Periodontol 2005 32:7-15. [Google Scholar]
[8]. Dental plaque-induced gingival diseases, Annals of periodontology, 1999 [Google Scholar]
[9]. Oh JJ, Eber R, Wang HL, Periodontal diseases in child and adolescentsJ Clin Periodontol 2002 29:400-10. [Google Scholar]
[10]. Shafer Hine Levy Shafer’s textbook of oral pathology 2009 6th edIndiaElsevier:254-310.Chapter 4, Cysts and tumours of odontogenic origin [Google Scholar]
[11]. Enrique Bimstein, Matsson CD Lars, Growth and development considerations in the diagnosis of gingivitis and periodontitis in childrenAmerican Academy of Pediatric Dentistry 1999 21(3):186-191. [Google Scholar]
[12]. Sigrun Zachrisson, Bjorn U. Zachrisson, Gingival condition associated with orthodontic treatmentAngle Orthodont 1972 42(1):26-34. [Google Scholar]
[13]. Nakagawa S, Fujii H, Machida Y, Okuda K, A longitudinal study from prepuberty to puberty of gingivitisJclin Periodontol 1994 21:658-65. [Google Scholar]
[14]. Slots J, Moenbo D, Microbiota of gingivitis in manScand J Dent 1978 86:174-81. [Google Scholar]
[15]. Serhat Demirer, Gingival hyperplasia as an early diagnostic oral manifestation in acute monocytic leukemia: A case reportEur J Dent 2007 1(2):111-14. [Google Scholar]
[16]. Armitage G, Development of a classification system for periodontal diseases and conditionsAnn Perodontol 1999 4:1-6. [Google Scholar]
[17]. Seymour RR, Ellis JS, Thomason JM, Risk Factors for drug induced gingival overgrowthJ Clin Periodontol 2000 27:217-23. [Google Scholar]
[18]. Genco RJ, Zambon JJ, Christersson LA, The origin of periodontal infectionsAdv Dent Res 1988 2:245-59. [Google Scholar]
[19]. Marshall-Day CD, Shourie KL, A roentgenographic survey of periodontal disease in IndiaJ Am Dent Assoc 1949 39:572-88. [Google Scholar]
[20]. Johnson B, Engel D, ANUG. A review of diagnosis,etiology and treatmentJ periodontal 1986 57:141-50. [Google Scholar]
[21]. Koch Bernadette L, Charles Myer III, John C. Egelhoff, Congenital EpulisAJNR 1997 18:739-41. [Google Scholar]
[22]. Havdar SG, Tercan A, Uckan S, Gurakan B.L, Congenital gum synechiae as an isolated anomaly: a case reportClinPediatric Dent 2003 28(1):81-83. [Google Scholar]
[23]. Tae-Ju Oh, Robert Eber, Hom-Lay Wang, Periodontal diseases in the child and adolescentJournal of Clinical Periodontology 2002 29(5):400-10. [Google Scholar]
[24]. DeAngelo S, Murphy J, Claman L, Kalmar J, Leblebicioglu B, Hereditary gingival fibromatosis — a reviewCompend Contin Educ Dent 2007 28(3):138-43. [Google Scholar]
[25]. Ongole Praveen B N, Textbook of Oral Medicine, Oral Diagnosis and Oral Radiology 2010 IndiaElsevier:523Chapter 19, Periodontal Diseases [Google Scholar]
[26]. Califano JV, American academy of periodontology- Research, Science and Therapy committee. Periodontal diseases of children and adolescentsJ. Periodontol 2003 74:1696-704. [Google Scholar]
[27]. Bimstein E, Peridontal health and disease in children and adolescentsPediatric Clin North America 1991 38:1183-1207. [Google Scholar]
[28]. Stina Syrjänen, Viral infections in oral mucosaEuropean Journal of Oral Sciences February 1992 Volume 100(Issue 1):17-31. [Google Scholar]
[29]. Leggott PP, Robertson PP, Greenspan D, Wara DW, Greenspan JS, Oral manifestations of primary and acquired immunodeficiency disease in childrenPediaric Dent 1987 9:98-104. [Google Scholar]