Oral cancer is one of the most common forms of malignancy, representing 2–4% of all the malignancies in developed countries and almost 40% of all cancers in the Indian subcontinent. In spite of major advances in diagnostic & therapeutic sciences, the pathology is still one of the major causes of untimely death [1]. The prognosis of patients who are treated early is much better, with five year survival rates as high as 80% [2].
A significant proportion of oral squamous cell carcinomas (OSCC), the most common form of oral malignancy, develop from premalignant lesions such as leukoplakia, erythroplakia as well as conditions like oral submucous fibrosis. Although recent advancement in research methodologies as well as longitudinal follow up of the rate of incidence, confirms genetic factors as a major contributing factor in etiopathogenesis of such malignancies [3–5].
Variety of primarily non-candidal oral mucosal lesions are reported to be associated with candida including leukoplakia, lichen planus, oral submucous fibrosis, fibroma, papilloma, pemphigus vulgaris and cheilitisactinica [6]. In addition, it has recently been observed that Candida albicans is much more frequently detected in the biofilms of oral squamous cell carcinoma sites as well as some premalignant lesions, than in control areas [7]. However, the mechanism of occurrence, as well as the significance of infection in each of these diseases is not established. Absence of confirmatory data regarding such correlation was considered as the need for the current study.
This cross-sectional study was designed to evaluate the presence of candidal organisms with the degree of dysplastic changes in lesions of oral mucosa, with following aims and objectives:
The aims of the study were to investigate the presence of Candidal organisms in oral mucosal lesions, by studying PAS stained cytosmear and histopathological sections of mucosal lesions. The second aim of the study was investigate the degree of dysplasia of such oral mucosal lesions.
The objective of the study was to correlate the presence of Candidal organisms if any, with the degree of dysplasia of oral mucosal lesions.
Materials and Methods
The study involved thorough evaluation of interested volunteers for oral mucosal lesions and investigating for the presence of candidal organisms in Periodic Acid Schiff (PAS) stained cytosmear and histopathologic sections of intra oral lesions. The dysplastic changes of same lesions were investigated by evaluating Hematoxylin & Eosin (H&E) stained histopathologic sections.
Ethical clearance was obtained from the ethical committee of the institution to conduct the study.
During the study period, which spanned for nine months, 65 patients were short listed. Out of these 15 patients had to be excluded from the study either because of their unwillingness to participate in the study or due to some serious systemic problems making them unfit to undergo the surgical procedures. Participants who demonstrated high scores for oral hygiene were not included, as this condition is known to influence number of candidal organisms in the oral micro flora. Hence, the final sample comprised of 50 participants visiting the outpatient section of the Department of Oral medicine. The volunteers not less than 18yrs of age and with clinically definable oral mucosal lesions were included in this study. Patients suffering from any systemic or oral ill health, rendering the person unfit for the surgical procedure, and oral mucosal lesions other than red and white were excluded from this study.
After obtaining the duly signed consent, the participants were examined thoroughly for oral mucosal lesions. The lesions were diagnosed based only on clinical features as explained by Mats Jontell & Palle Holmstrup [8], R.Rajendran [9], Neville, Damm, Allen, Bouquot [10]. The details such obtained were sincerely recorded on a custom made performa, designed for the study. The lesions were further photographed for the record purpose.
Exfoliative cytology and Incisional biopsy of the lesion was carried out on the same day of diagnosis of the lesion using standard procedure. The cytosmear and the biopsy specimen were sent to Department of Oral Pathology for evaluation. The incisional biopsy specimen was evaluated using H&E stain and PAS stain to assess the degree of dysplasia and presence of Candidal hyphae respectively. The cytosmear was stained with PAS also to assess candidal hyphae. Cytosmears and histopathological sections were evaluated for hyphal form alone as only this stage of organism describes colonization within epithelium.
H&E stained slides were evaluated for various forms of epithelial dysplastic changes as described by Krammer, et al. 1978[11]. The dysplastic changes were further categorized into: mild, moderate & severe stage. These observations were noted by an oral pathologist. The findings of microscopic pictures were recorded using Microsoft excel software program. The significant fields of histopathological sections were recorded with the help of photomicrograph using Lawrence & Mayo research microscope with camera. The results thus obtained were statistically analysed using Chi square analysis. p-value<0.05 was considered statistically significant.
Results
A total of 50 patients were checked for oromucosal lesions. Out of these 50 patients, 45 patients had lesions on the buccal mucosa, 4 patients had lesions the labial mucosa & one patient had lesions on the gingiva. Out of 45,12 of these patients were smokers, 14 were gutkha chewers, 3 used to keep tobacco quid in their vestibular region, 6 patients consumed tobacco and gutkha, 5 patients chewed gutkha and were smokers, 1 patient used tobacco as quid & was smoker, 1 patient chewed pan with tobacco, 1 patient chewed mawa, 2 patients chewed mawa and were smokers. Five patients kept tobacco as quid, chewed gutkha and were smokers.
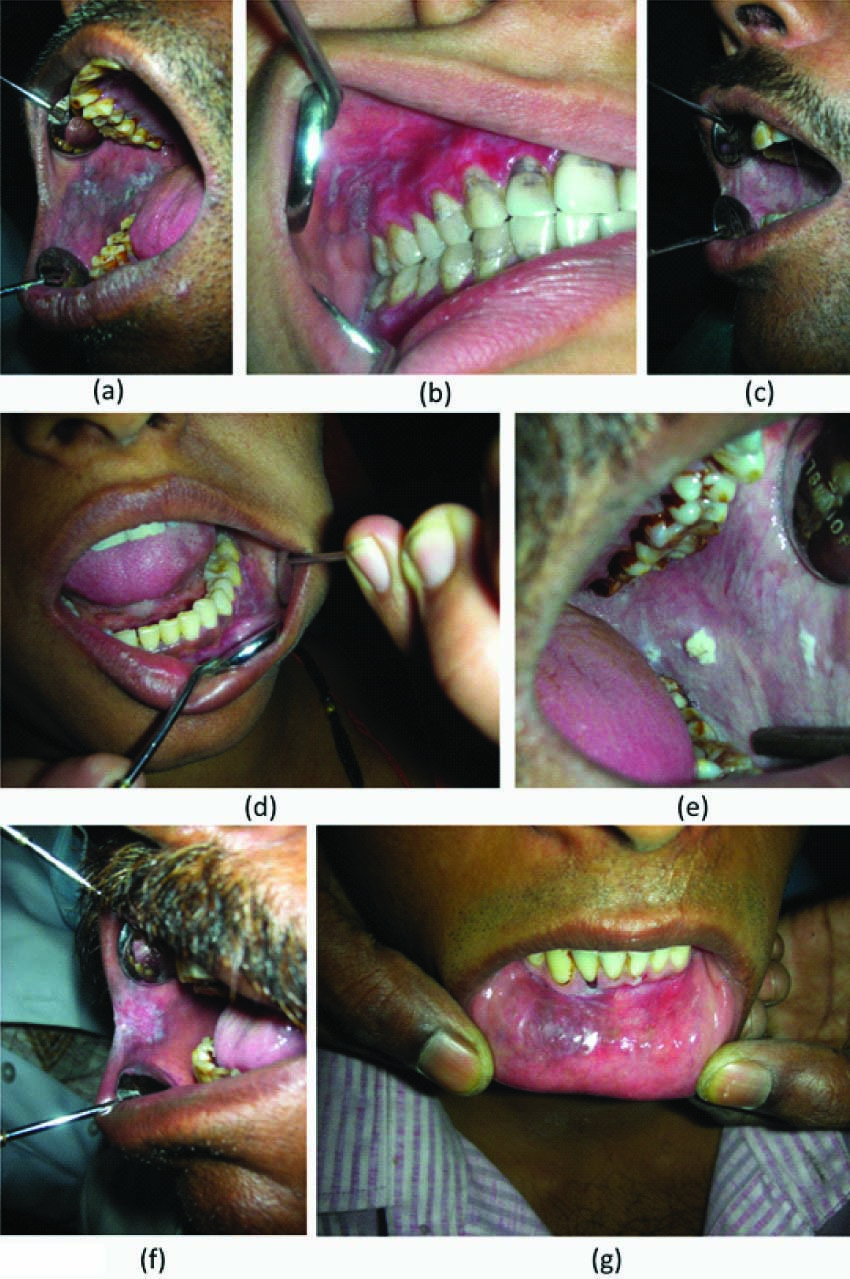
The clinical as well as histopathological findings of different oral lesions have been shown [Table/Fig-1,2]. [Table/Fig-1a–g] corresponds to clinical pictures of patients suffering from Homogenous leukoplakia, Lichen planus, Oral submucous fibrosis, Lichenoid reaction, Verrucous leukoplakia, Speckled leukoplakia, and Tobacco Pouch Keratosis respectively.
Clinical picture of various oral lesions
Histopathological appearance of various oral lesions
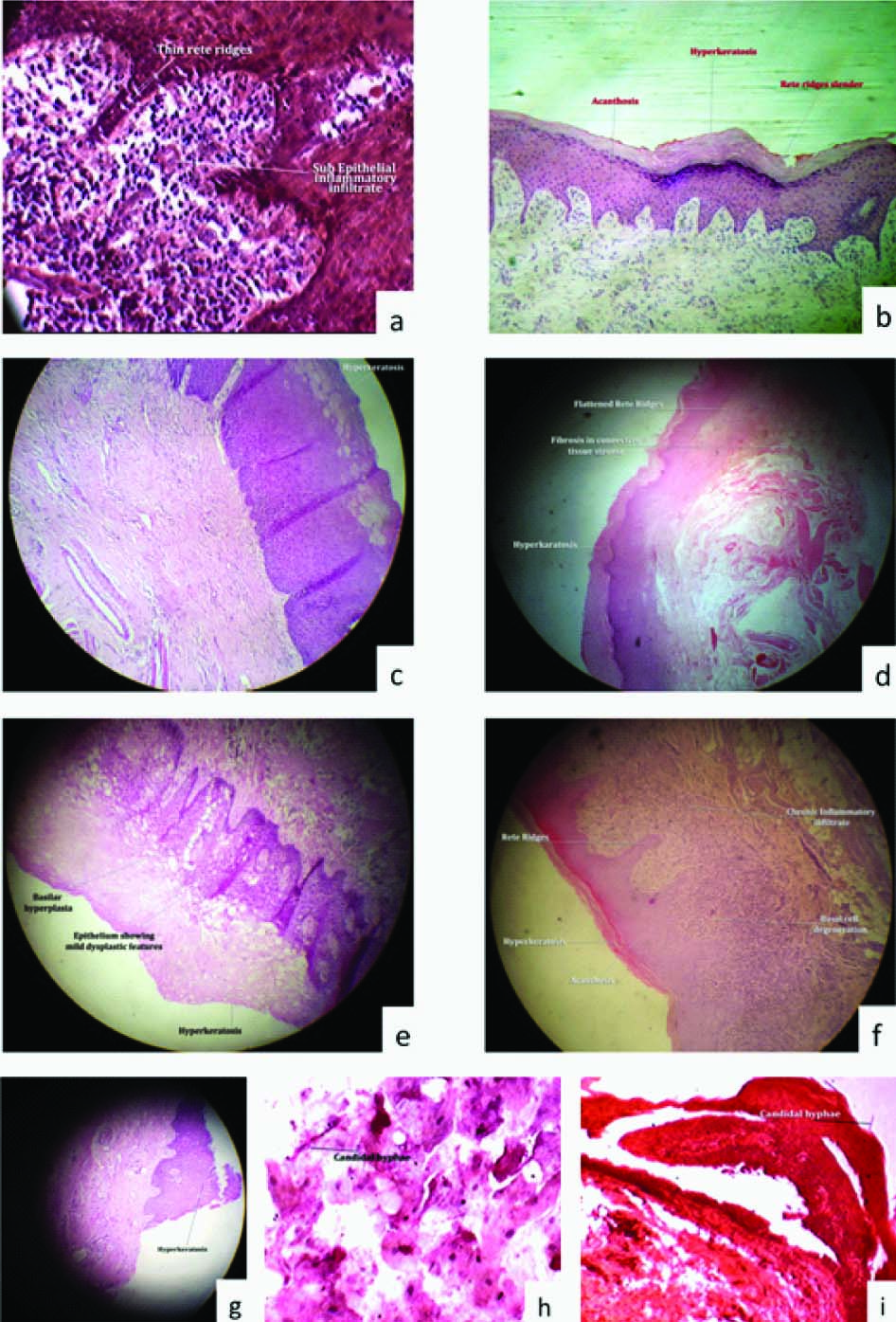
[Table/Fig-2a–i] correspond to the histopathological pictures of Lichenoid reaction, Verrucous Leukoplakia, Homogenous Leukoplakia, OSMF, Speckled Leukoplakia, Lichen planus, Tobacco pouch keratosis, Candidal presence in the histopathological specimen & Candidal presence in the cytosmear respectively.
Majority of the patients (N=15) had Oral Submucous fibrosis, followed by Homogenous leukoplakia (N=13). Amongst the patients who had OSMF, 10 patients demonstrated candida in the cytosmear. Histopathological analysis showed that candida was present only in patients who had OSMF and Lichenoid reactions [Table/Fig-3].
Lesions evaluated, presence of candida in cytosmear and histopathological specimen and presence of dysplasia
| Conditions | Number of Participants | Number of Candida Present in Cytosmear | Number & Type of Dysplasia Present | Number Of Candida Present in Histopathological Specimen |
|---|
| Oral submucous fibrosis | 15 | 10 | 4 (Mild-2, Moderate-1, Severe-1) | 1 |
| Homogenous leukoplakia | 13 | 6 | 4(Mild-3, Moderate-1) | Absent |
| Lichen planus | 6 | 5 | 1 (Moderate) | Absent |
| Lichenoid reaction | 7 | 3 | 1 (Mild) | 1 |
| Speckled leukoplakia | 4 | 1 | 4 (Mild) | Absent |
| Verrucous leukoplakia | 2 | 1 | 1 (Mild) | Absent |
| Tobacco pouch keratosis | 3 | 0 | 1 (Mild) | Absent |
| Total | 50 | 26 | 16 | 2 |
No significant differences (p-value= 0.308) were observed between presence of candida in cyto smear with presence of epithelial dysplasia [Table/Fig-4].
Cross tabulation between presence of Candida in cytosmearand epithelial dysplasia., X2 = 1.039, p=0.308
| Dysplasia | | Candida in Cytosmear | Total |
|---|
| Present | Absent |
|---|
| Present | Count | 10 | 6 | 16 |
| % of Total | 20.0% | 12.0% | 32.0% |
| Absent | Count | 16 | 18 | 34 |
| % of Total | 32.0% | 36.0% | 68.0% |
| Total | Count | 26 | 24 | 50 |
| % of Total | 52.0% | 48.0% | 100.0% |
No significant differences (p-value= 0.166) were observed between presence of candida in cytosmear and candida in histopathological specimen [Table/Fig-5].
Cross tabulation between presence of Candida in histopathological specimen and Candida in cytosmear, X2 = 1.923, p=0.166
| Candida in histopathological specimen | | Candida in Cytosmear | Total |
|---|
| Present | Absent |
|---|
| Present | Count | 2 | 0 | 2 |
| % of Total | 4.0% | 0% | 4.0% |
| Absent | Count | 24 | 24 | 48 |
| % of Total | 48.0% | 48.0% | 96.0% |
| Total | Count | 26 | 24 | 50 |
| % of Total | 52.0% | 48.0% | 100.0% |
Frequency distribution of candidal presence among various lesions showed that patients who had OSMF, demonstrated maximum percentage (20%) of candida in cytosmear followed by homogenous leukoplakia (12%). However no significant differences were observed between the presence of candida in cytosmear and different oral lesions. (p-value=0.205) [Table/Fig-6].
Frequency distribution of candidal presence among various lesions., X2 = 18.487, P= 0.205
| ese | | Total | Candida in Cytosmear |
|---|
| Present | Absent |
|---|
| Oral submucous fibrosis | Count | 15 | 10 | 5 |
| % of Total | 30.0% | 20.0% | 10.0% |
| Speckled leukoplakia | Count | 4 | 1 | 3 |
| % of Total | 8.0% | 2.0% | 6.0% |
| Verrucous leukoplakia | Count | 2 | 1 | 1 |
| % of Total | 4.0% | 2.0% | 2.0% |
| Homogenous leukoplakia | Count | 13 | 6 | 7 |
| % of Total | 26.0% | 12.0% | 14.0% |
| Lichen planus | Count | 6 | 5 | 1 |
| % of Total | 12.0% | 10.0% | 2.0% |
| Lichenoid reaction | Count | 7 | 3 | 4 |
| % of Total | 14.0% | 6.0% | 8.0% |
| Tobacco pouch keratosis | Count | 3 | 0 | 3 |
| % of Total | 6.0% | .0% | 6.0% |
| Total | Count | 50 | 26 | 24 |
| % of Total | 100.0% | 52.0% | 48.0% |
No significant differences (p-value= 0.099) were observed between the presence of epithelial dysplasia and various oral lesions [Table/Fig-7].
Cross tabulation between dysplasia and various lesions., X2 = 10.663, p=0.099
| Dysplasia | | Lesions | Total |
|---|
| Oral submucous fibrosis | Speckled leukoplakia | Verrucous leukoplakia | Homogenous leukoplakia | Lichen planus | Lichenoid reaction | Tobacco pouch keratosis |
|---|
| Present | Count | 4 | 4 | 1 | 4 | 1 | 1 | 1 | 16 |
| % of Total | 8.0% | 8.0% | 2.0% | 8.0% | 2.0% | 2.0% | 2.0% | 32.0% |
| Absent | Count | 11 | 0 | 1 | 9 | 5 | 6 | 2 | 34 |
| % of Total | 22.0% | .0% | 2.0% | 18.0% | 10.0% | 12.0% | 4.0% | 68.0% |
| Total | Count | 15 | 4 | 2 | 13 | 6 | 7 | 3 | 50 |
| % of Total | 30.0% | 8.0% | 4.0% | 26.0% | 12.0% | 14.0% | 6.0% | 100.0% |
Discussion
Oral yeast carriage denotes colonization of the mouth by yeast without overt infection. The yeast that colonizes in the mouth is the source of oral candidiasis. Candida species are innocuous oral commensals and when optimal conditions supervene, they cause diseases. A diverse array of local factors such as trauma, maceration, atrophy, hyperplasia, dysplasia and systemic factors, such as iron deficiency and malnutrition, may facilitate candidal infection [12].
Presence of Candida in the mouth together with epithelial changes may predispose to candidal infection. Candidal infection together with other co-factors may also induce epithelial atypia and dysplasia leading to malignant change [12].
The present study was designed to evaluate the correlation between presence of candidal organisms and epithelial dysplasia in various oral mucosal lesions associated with areca nut and tobacco use.
Out of 50 participants included in the study, 15 (30%) were clinically diagnosed with Oral submucous fibrosis, 13 (26%) with Homogenous leukoplakia, 7 (14%) with Lichenoid reaction, 6 (12%) with Lichen planus, 4 (8%) with Speckled leukoplakia, 3 (6%) with Tobacco pouch keratoses and 2 (4%) with Verrucous leukoplakia. Such a spectrum of multiple lesions was also considered in the previous studies done by AW Barrett et al.,[13] & Nada Vuckovic et al., [6].
In the present study, the most common study site was buccal mucosa (45/50, 90%), as the lesions defined in the study were mostly found in relation to buccal mucosa. Several studies report incidence of Candidiasis being more commonly associated with respect to this region [14,15]. Apart from buccal mucosa, lesions were also present on labial mucosa, gingiva, floor of the mouth and oropharynx.
Correlation of presence of Candida with gender was not done as it has already been proved that gender has no influence on the yeast carriage in the mouth [16].
To study the presence of Candida in the superficial layers of the epithelium cytosmears were evaluated, whereas, for evaluating the presence of the fungal organism in deeper layers of the epithelium, histopathological specimen was prepared. Staining for the organism was done with PAS stain both for cytosmears as well as for histopathological specimen. Evaluation of presence of dysplasia was done by staining the histopathological specimen by H&E stain. Similar method has been explained by Nada Vuckovic et al.,[6].
In the present study, Candida was diagnosed in 26 out of 50 cytosmears (52%). Lesion having maximum candidal presence detected by exfoliative cytology was Lichen planus accounting for 83.3% (5 out of 6 smears). 25-90% of healthy population are Candida carriers according to certain studies [17–21]. It may also be possible that the increased colonization and prevalence of oral yeast in these lesions is entirely coincidental and merely reflects a changed local environment that allows for the proliferation of these common oral commensals [22, 23]. Thus, the presence of Candida itself may not be sensitive enough to draw any definite conclusion regarding malignant potential. In a similar study, candidal presence was found in 3 out of 30 cases (10%) using exfoliative cytology with PAS staining [6].
Other studies using non invasive techniques to estimate the presence of candidal hyphae in the oral cavity, other than exfoliative cytology included: Swab and culture method which yielded 90.1% [24] & 64% [25] yeasts & Rinse and culture method, which yielded 74.7% [7] & 75%[16] yeasts.
The method used to obtain the sample and to detect the fungi significantly affects the findings [17]. There is abundant evidence that values of fungal infection as assessed by PAS staining are lower than those obtained by culture. The disharmony in the study results may be explained by the fact that, majority of previous studies were done by using the culture method to evaluate the presence of candidal organisms as compared to exfoliative cytology in the present study.
In the present study, incidence of dysplasia was maximum in Speckled leukoplakia, accounting for 100% (4 out of 4 participants, Mild dysplasia), followed by Verrucous leukoplakia 50% (1 out of 2 participants, Mild dysplasia).
Candida was present only in 2 out of 50 cases (4%) in histopathological sections. These were present in 1 case of Oral submucous fibrosis with mild dysplasia and Lichenoid reaction with no dysplasia respectively. However, previous studies done based on similar criteria reported the incidence of 20% [6] & 4.7% [13] candida presences in the histological specimens stained by PAS.
Such variations may be because of the site that is studied. It has been previously reported that the tongue, particularly the dorsal surface is the site most vulnerable to candidal infection [17]. It might be because of the physical protection afforded to the candidal organisms by the papillary epithelium. One study done on the similar criteria by AW Barrett [13] revealed that a total of 6.7% tongue biopsies showed fungal infection.
Since in the present study, no specimen for biopsy or cytological evaluation was taken from the tongue mucosa as done by AW Barrett [13], we may have got a lesser proportion of Candida positive samples, leading to discrepancy in the results between these two studies.
In the present study, when grades of dysplasia were compared with candidal presence in the histopathological sections, Candida was found in mildly dysplastic Oral submucous fibrosis but not found in one case of severely dysplastic Oral submucous fibrosis. Candida was also found in Lichenoid reaction which showed no dysplastic features. Thus in our study, we could not correlate candidal presence to degree of dysplasia. This could probably be because of reduced number of sample size.
When different oral lesions were evaluated, a discrepancy of candidal organisms and epithelial dysplasia was observed, in most of the lesions.
Summarizing the results of the present study, Candida was present in 32% of cases without dysplasia, and 20 % with dysplasia, and no correlation was observed between presence of candida & epithelial dysplasia among various oral lesions (p-value 0.308). The retrospective study done by Luis Carlos Spolidorio et al.,[26]. also showed a similar result. On the contrary, AW Barrett et al., [13] found a statistically significant association between histologically determined fungal infection and epithelial dysplasia. These variations in the present study and other studies could be because of small sample size, variation in collection of sample and processing techniques.
After obtaining the biopsy specimen & exfoliative cytology specimen, various patients were treated in accordance with their lesions. All the patients were advised to quit the habit of tobacco consumption and areca nut chewing. Patients having Grade I & II OSMF were given intra lesional injections of dexamethasone sodium phosphate (4mg/ml) and hyaluronidase (1500 IU). The intra-lesional injections were given at multiple sites once a week for six weeks. Grade III OSMF patients were referred to oral surgeon for surgical excision of fibrous bands. Patients having leukoplakia were treated using 13-cis retinoic acid, 2 mg/kg body weight for three months, with periodic follow up. Regime used for Lichen planus patients consisted of topical application of 0.1% triamcinolone acetonide (Ointment TESS) four times a day for two weeks. As per for Lichenoid reaction patients, the causative agent was evaluated and removed. In case of persistent erythema & burning sensation, ointment TESS was advised for a period of 2 weeks.
All the patients having moderate & severe dysplasia were referred to an oncologist for further opinion & treatment.
Conclusion
The overall analysis of the study revealed no positive correlation between the incidence as well as severity of epithelial dysplasia, with the presence of candidal organisms. Though the cytosmears demonstrated the organisms to a greater extent, this may not be considered as reliable evidence, significant enough to adapt such protocol during investigation of premalignant lesions. Neither it can be considered to have a prognostic value as cytosmears could always be expected to get contaminated with Candida, that are otherwise present as normal commensal. The result of cytosmear did not correlate with the histopathological sections stained for Candida, which further weakens the hypothesis of association of Candida with the degree of epithelial dysplasia. But at the same time, it is also realized that a longitudinal study involving greater number of lesions utilizing newer sophisticated techniques to access candidal presence may provide better answers.