Corticotomy-assisted orthodontic treatment is an established and efficient technique that has gradually gained popularity as an adjunct treatment option for the orthodontic treatment of adults. Over the last two decades, the refinements of an attempt to engineer an “optimal response” of alveolar bone to an applied “optimal force” has propelled both the periodontal and the orthodontic specialties directly into the field of surgical dento-facial orthopedics [1].
Corticotomy has roots in orthopedics going back to the early 1900s. In 1892, it was first defined as a linear cutting technique in the cortical plates surrounding the teeth to produce mobilization of the teeth for immediate movement [2]. Heinrich Köle’s publication in 1959 however, laid the foundation for the subsequent evolution in decortication-facilitated orthodontics [3].
Corticotomy is defined as the osteotomy of the cortical bone. A Corticotomy is a procedure whereby only the cortical bone is cut, perforated, or mechanically altered in a controlled surgical manner and at the same time penetrating into the bone marrow minimally. This is in contrast to an osteotomy, which is defined as a surgical cut through both the cortical and medullary bone [4]. This term is frequently used when describing the creation of bone segments.
After any trauma to bone tissues, remodeling, which is commonly found in the bone tissue structures is greatly increased to accelerate the repair process and consequently functional recovery. This takes place by a phenomena called as Regional Accleratory Phenomena RAP [5] (Harold Frost). RAP is believed to occur after a fracture, arthrodesis, osteotomy or any bone grafting procedure [6].
The rapid tooth movement in corticotomy is because of increased bone turnover in response to surgical trauma. This change in the bone physiology results in a localized decrease in trabecular bone density, which in turn would offer less resistance to tooth movement [7].
The AOO (Acclerated Osteogenic Orthodontics) technique does not owe its success to revolutionary materials that have defined orthodontic progress in the past, although the efficiency of one’s orthodontic tooth movement system can be greatly enhanced. The AOO treatment instead focuses on enhancing the manner in which the periodontium responds to applied forces and on providing for a more intact periodontium and increased alveolar volume to support the teeth and overlying soft tissues in retention. The surgical component of the AOO technique is an in-office procedure. The postoperative recovery should be no more uncomfortable than that of other orthodontic-related surgeries such as third molar removal, bicuspid extractions, and gingival grafting, and it is certainly less of an issue than the recovery following orthognathic surgery [3].
The AOO treatment creates a four to five month “window of opportunity” that provides more than enough time to accomplish the major tooth movements when the correct protocols are used. The AOO treatment also provides for an increased differential between anchorage and activated teeth. The activated teeth move so readily that the non-activated teeth provide better relative anchorage [3].
Materials and Methods
Source of Data
Subjects reporting to the Department of Orthodontics and Dentofacial Orthopedics at Institute Of Dental Sciences, Bareilly, India requiring orthodontic treatment were included in the study after obtaining an informed and written consent from the patients and their guardians. The study was approved by the ethical committee of Institute of Dental Sciences, Bareilly, India.
Patient Inclusion Criteria
On the basis of the diagnosis of the malocclusion, individuals requiring retraction of upper anterior teeth in the extraction space of First premolar were selected.
The patients should be a minimum of 15 y of age at the beginning of treatment to minimize confounding results due to growth.
Patients with good periodontal health and maintaining good oral hygiene were taken for the study.
Exclusion Criteria
Patients showing any signs of active periodontal disease.
Patients with severe crowding (≥ 3.5 mm) in maxillary arch.
Patients on long term corticosteroid therapy.
Individuals with inadequately treated endodontic problems.
Persons taking medications that slow down bone metabolism, such as bisphosphonates and NSAIDS.
Patients were randomized into control and corticotomy groups. Each group consisted of 10 subjects.
Control group: Subjects who underwent orthodontic treatment without corticotomy.
Corticotomy group: Subjects who underwent orthodontic treatment after corticotomy.
Age range for the patients in control group was 15-25 y and for the corticotomy group was 16-25 y, with a mean ± S.D of 19.8 ± 3.22 for control group and 18.8 ± 3.48 for corticotomy group respectively.
Each group was having nine females and one male member thus female patients form 90% of the study population i.e. subjects of both group were age and gender matched and were thus comparable.
After case selection, patients were bonded with MBT brackets (0.022 slot T.P Orthodontics), initial alignment and leveling of the upper anterior teeth was done by using 0.014” NiTi arch wire and further, till a 0.016 x 0.22″ stainless steel wire fits passively in the bracket slots [Table/Fig-1]. The patients of the control group were referred to the Department of Oral Surgery for extraction of the upper first premolars. The patients in the corticotomy group were referred to Department of Periodontics for surgery.
Upper arch with 0.16 x 0.22 stainless steel wire in place

Surgical Procedure
Corticotomy surgery was performed in the maxillary alveolar region from mesial surface of maxillary 1st premolar of one side to the other side. Surgery was performed under local anaesthesia. A full thickness periosteal flap was raised and using 2 mm round bur under proper saline irrigation, vertical grooves were placed in the interradicular space, midway between the root prominences in the alveolar bone. The grooves were made to extend from a point 2 to 3 mm above the crest of the bone to a point 2 mm beyond the apices of the roots [4]. Horizontal corticotomy cuts were made, joining these vertical cuts, from labial and lingual sides of the maxillary alveolar region [Table/Fig-2a,b]. 1st premolars were extracted, at the same time the surgical site was then covered by Demineralised Freeze Dried Bone Allograft (DFDBA) after the completion of surgery [Table/Fig-3a,b]; sutures were given after placing the raised flap back [4] [Table/Fig-4]. Patients were recalled after two weeks for suture removal and for placement of arch wire to start the retraction of maxillary anterior segment [6,8].
Mucoperiosteal flap reflected and vertical and horizontal corticotomy cuts placed along with alveolar perforations on buccal side

Mucoperiosteal flap reflected and vertical and horizontal corticotomy cuts placed along with alveolar perforations on buccal side

Bone graft placed over the corticotomized area (buccal surface)

Bone graft placed over the corticotomized area (palatal surface)

Sutures placed after the completion of corticotomy procedure

En masse retraction of the anterior segment was carried out in a similar manner in both the control as well as corticotomy group, using a NiTi closed coil spring, which delivered a constant force of 250 gm. The closed coil spring were placed from the canine and was posteriorly engaged to the molar hook [Table/Fig-5] . The coil springs were removed only after the completion of retraction i.e. when the canine touches the mesial surface of upper second premolar tooth [Table/Fig-6]. A Transpalatal arch was used for anchorage reinforcement in both the groups.
Retraction started using niti closed coil spring

Space closure after 4 months of active orthodontic treatment

Treatment Records
After patient selection, routine records of all the patients such as a detailed case history, pre-treatment study models, extra oral and intra oral photographs, Lateral Cephalograms [9], Orthopantomograms. Computed Tomographic scans were acquired, for the corticotomy group.
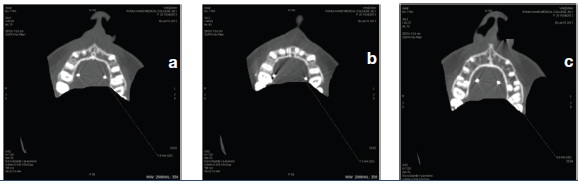
Computed Tomography was used for evaluating the changes in the alveolar bone thickness before and after the retraction of anterior teeth in corticotomy group subjects only. In addition, contiguous 0.625 mm slice thickness CT scans were obtained for the maxillary incisors at 120 kV, 175 mA, with the window width set at 2000, 1500 HU (GE Bright Speed 16 Slice China) [Table/Fig-7].
GE bright speed 16 ct scan machine

CT scanning was done perpendicular to the long axis of the incisors on the desired jaw, and this angle was determined by setting the gantry angle according to the lateral scanogram of the head position. For each tooth, the thickness of the labiolingual alveolar plates measurements were taken to the nearest 0.2 mm.
The thickness of the alveolar plates were measured for each tooth in three slices separated by 3 mm i.e. at crestal level (S1), mid root level (S2), and apical level (S3) [Pre-Treatment(T1)]. The same measurements were repeated after incisor retraction was completed (depending upon the case) {Post Treatment (T2)}. [Table/Fig-8a–c] All measurements on CT scans were made by the same investigator.
Evaluation of alveolar bone thickness in maxillary slice at crestal level (S1), mid root level (S2), and apical level (S3)
Statistical Analysis
The statistical analysis was done using SPSS (Statistical Package for Social Sciences) statistical Analysis Software. Parametric statistical tests: paired t-test was used to determine the significance of changes in the groups after the corresponding treatment. An inter examiner reliability test was performed for control and corticotomy group by using intra class correlation coefficient (r) and was found to be very high i.e. r = 0.95 and r = 0.94 respectively. A confidence level larger than 5% was considered statistically not significant.
Results
A total of 20 patients were selected for the study and were randomly distributed in the control and corticotomy groups.
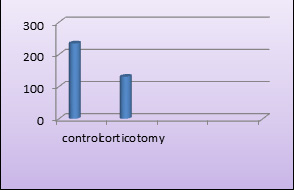
From [Table/Fig-9], it can be seen that, a significant difference in retraction time (days) was observed between control and corticotomy groups (p<0.001). Implying that, the retraction time (days) was significantly higher in control group as compared to corticotomy group [Table/Fig-10].
Comparison of retraction time in control and corticotomy groups (days) by t-test
| Variable | Group | Mean | S.D. | t-value | p-value |
|---|
| Retraction time | Control group | 234.10 | 8.91 | 28.3319 | <0.001* |
| Corticotomy group | 130.50 | 7.37 |
Comparison of retraction time in control and corticotomy groups (days) by t-test
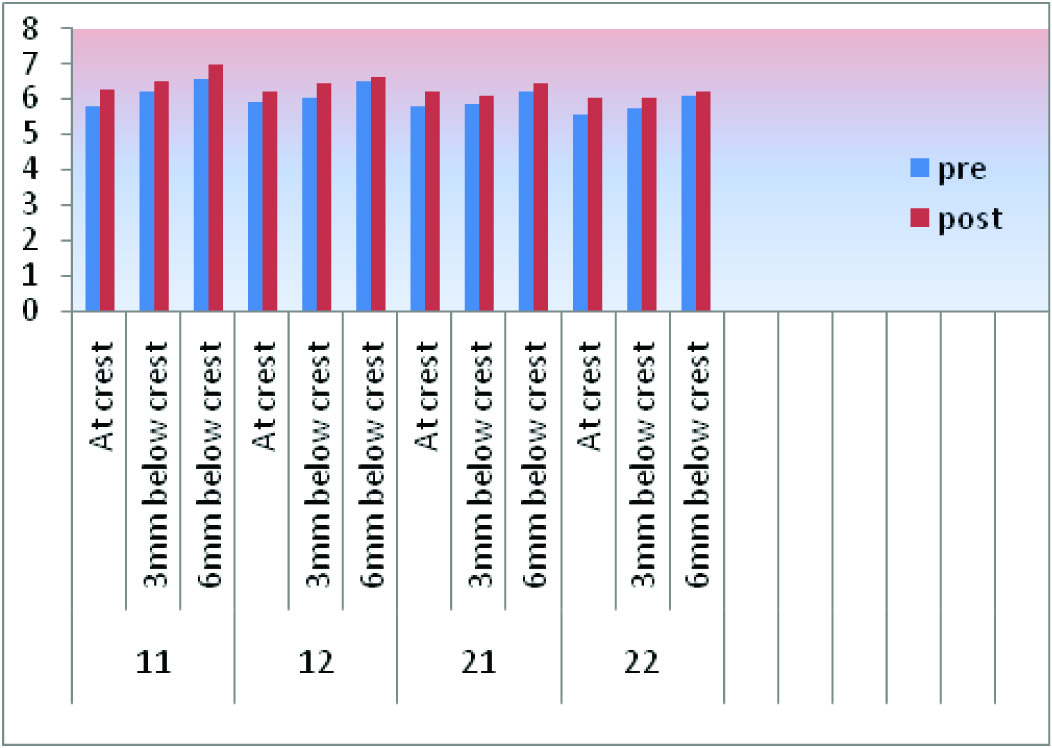
The results for changes in alveolar bone thickness as measured on CT scans from pre treatment to post treatment are listed in [Table/Fig-11]. At the crestal level(S1) alveolar bone width showed highly significant increase for all the incisors(p<0.001).Alveolar bone width at the mid root level (S2) showed significant increase for all the incisors except left central incisor at 5% level of significance(p<0.005), Regarding the bone width at S3 level only the central incisors showed significant difference (p<0.005).
Comparison of pre-treatment and post-treatment alveolar bone thickness at s1,s2,s3 levels by paired t-test
| Tooth No. | Variable | Pre | S.D. | Post | S.D. | T/t Change | S.D. Diff. | % OF Change | Paired t | p-value |
|---|
| 11 | S1 | 5.83 | 0.81 | 6.26 | 0.74 | 0.43 | 0.18 | 7.38 | 7.6955 | < 0.001* |
| S2 | 6.24 | 0.66 | 6.52 | 0.61 | 0.28 | 0.25 | 4.49 | 3.5624 | 0.0061* |
| S3 | 6.60 | 0.96 | 6.97 | 0.77 | 0.37 | 0.30 | 5.61 | 3.9220 | 0.0035* |
| 12 | S1 | 5.93 | 0.82 | 6.24 | 0.85 | 0.31 | 0.18 | 5.23 | 5.4706 | < 0.001* |
| S2 | 6.07 | 1.00 | 6.45 | 1.05 | 0.38 | 0.15 | 6.26 | 7.7567 | < 0.001* |
| S3 | 6.49 | 1.10 | 6.65 | 1.04 | 0.16 | 0.27 | 2.47 | 1.8628 | 0.0954 |
| 21 | S1 | 5.81 | 0.92 | 6.25 | 1.09 | 0.44 | 0.27 | 7.57 | 5.2015 | < 0.001* |
| S2 | 5.88 | 1.08 | 6.12 | 1.01 | 0.24 | 0.52 | 4.08 | 1.4685 | 0.1760 |
| S3 | 6.25 | 1.12 | 6.44 | 1.07 | 0.19 | 0.20 | 3.04 | 2.9673 | 0.0158* |
| 22 | S1 | 5.59 | 0.86 | 6.05 | 0.87 | 0.46 | 0.15 | 8.23 | 9.6619 | < 0.001* |
| S2 | 5.75 | 0.86 | 6.06 | 0.85 | 0.31 | 0.26 | 5.39 | 3.7686 | 0.0044* |
| S3 | 6.11 | 1.25 | 6.22 | 0.99 | 0.11 | 0.59 | 1.08 | 0.5899 | 0.5697 |
The comparison of pre and post treatment alveolar bone thickness at S1,S2,S3 levels by paired t-test are also shown in [Table/Fig-12].
Comparison of pretreatment and post-treatment alveolar bone thickness at s1,s2,s3 levels by paired t-test
Discussion
Orthodontic tooth movement is a process in which a mechanical force is applied to induce alveolar bone resorption on the pressure side, and alveolar bone deposition on tension side [10]. Conventional orthodontic treatments with either fixed or functional appliances rely on biological tooth movements. Using conventional techniques, biological tooth movement can be achieved at a limited rate. Individual factors such as optimum force, turn over in periodontal ligament, and bone metabolism plays a role in determination of rate of tooth movement [11].
Time is an essential factor in the course of orthodontic treatment. Traditional orthodontic therapy in patients often results in protracted treatment time due to which many patients forgo orthodontic treatment [12]. Since the last few decades many attempts have been made to shorten the time needed for tooth movement. Various methods to fasten the orthodontic tooth movement are: local administration of chemicals [13], physical or mechanical stimulation of the alveolar bone, such as the use of direct electrical current or magnets [14], and surgery, including dental distraction [15] and alveolar corticotomies [1,3,4].
Alveolar corticotomies are defined as surgical intervention limited to the cortical portion of the alveolar bone. Whereas in osteotomies both cortical and trabecular bone material is removed in considerable quantities. In corticotomy the incision must pierce the cortical layer, and at the same time, penetrate into the trabecular bone only minimally [4].
Optimal tooth movement requires the combination of well planned orthodontic forces [16] and an alveolar bone that offers less resistance to movement, i.e., less dense bone and increased bone metabolism. When alveolar bone metabolism is increased, orthodontic movement is accelerated [17]. Effective tooth movement enhancement has been demonstrated in laboratory studies with animals after the administration of certain drugs [18]; or by changing the optimal levels of hormones involved in regulating bone metabolism [19]. Change in bone physiology would result in a localized decrease in trabecular bone density, which in turn, would offer less resistance to tooth movement [6].
The corticotomy technique reduces treatment time when compared to conventional techniques by 30-50 %. The rapid orthodontic tooth movement in corticotomy is due to a phenomenon called as RAP (Regional Accleratory Phenomena). Yaffe et al., suggested that RAP in humans begins within a few days of surgery, typically peaks at 1 to 2 mnth, and may take 6 to more than 24 mnth to subside. They stated that the initial phase of RAP is characterized by an increase in cortical bone porosity because of increased osteoclastic activity. Frost stated that the duration and intensity of the RAP is proportional to the extent of injury and soft tissue involvement in the injury [5]. RAP is believed to occur after a fracture, arthrodesis, osteotomy or any bone grafting procedure [6].
There are many case reports that have been published in the literature regarding the corticotomy procedure and its advantages, but till date long term studies published in the orthodontic literature are rare.
So the present study was undertaken to evaluate the claimed accelerated orthodontic tooth movement after corticotomy as well as alveolar bone thickness is judged in the corticotomy group. Upper first premolars were extracted in all the patients in both groups. The two primary reasons for removal of permanent teeth are to correct a discrepancy between tooth size and arch length, and to reduce maxillary protrusion. In addition, the desire to control the vertical dimension can also be a reason to extract permanent teeth [20].
En masse retraction of the anterior teeth was carried out using a closed coil spring delivering a force of 250 g. Corticotomy surgical procedure was used in the corticotomy group to evaluate the claimed accelerated orthodontic tooth movement.
In the present study the treatment time required for the en mass retraction of anterior teeth was reduced by performing corticotomy procedure in the maxillary anterior alveolar region on buccal and palatal aspect of alveolar bone. By making horizontal and vertical corticotomy cuts in the alveolar bone, the resistance of the alveolar bone is reduced. Performing corticotomy procedure activates a phenomena called as RAP (Regional Accleratory Phenomena). Activation of RAP causes increase in osteoblastic and osteoclastic activity in the alveolar bone, which gives a “window period” of 4-6 mnth to carry out the required tooth movement at an accelerated rate [4].
The mean time for the en masse retraction in the corticotomy group was found to be 131±7.5 d, in comparison to 234±9 d for the conventional technique. There was a statistically significant reduction in the treatment time with corticotomy procedure (p<0.001) which is in accordance with the results obtained by Wilcko et al.,[1], Murphy et al.,[4], Saad et al., [21].
Computed tomographic scanning was performed in order to assess the dento-alveolar morphology in saggital dimension which cephalometric findings fail to reveal due to surrounding bone superimpositions. For this reason 3-D evaluation is required which could provide 3 dimensional displacement for dento-alveolar changes [22]. It was found that width of the alveolar bone irt maxillary anteriors had improved to a considerable level in the corticotomy group, which may be attributed to the osteoinductive graft material added during the surgical procedure. BA Twaddle et al., [23] conducted a similar study and concluded that Orthodontic therapy facilitated with corticotomy surgery and grafting improved alveolar bony support and resulted in permanent alveolar process width increase.
The changes in the present study were significant at the coronal level (S1) irrespective of the teeth. Alveolar bone width at the midroot level (S2) and at the apical level (S3) had also considerably increased but were inconsistent. Yodthong et al., [10], demonstrated a significant increase in the labial bone thickness at the crestal level during upper incisor retraction. Bimstein et al., [24] also reported an increase in the amount of buccal alveolar bone as a result of orthodontic treatment, and attributed it to lingual positioning of the procumbent mandibular permanent central incisor.
Further studies are needed to compare the difference in the treatment effects between male and female patients as related to bone differences and hormonal differences in bone re-organization. Simultaneously an increased sample size could have enhanced the accuracy than the present levels of the results in the study. The results of the study could have been analysed better had it been a split mouth design study. Finally long term changes in bone thickness after orthodontic treatment should be evaluated.
Conclusion
The results of the study led to the following conclusions-
On comparing the retraction time of the two groups, it was found that there was a significant decrease in the treatment time in corticotomy group, when compared to the control group.
Alveolar corticotomies with alveolar bone grafting provides the advantage of increased alveolar width to support the teeth and overlying structures.
This new method of retraction definitely reduces the treatment time, is viable and can be incorporated as a routine orthodontic protocol in clinical practice.