Juvenile Ossifying Fibroma with Aneurysamal Bone Cyst: A Case Report
A Vikram Simha Reddy1, K Rajeev Kumar Reddy2, A Ravi Prakash3, Rajinikanth4, Pavani Vidhyadhari5
1Reader, Department of Oral and Maxillofacial Pathology, G.Pulla Reddy Dental College. GPR Nagar, Nandyal Road, Kurnool, Andhra Pradesh, India.
2Professor, Department of Prosthodontics, G.Pulla Reddy Dental College. GPR Nagar, Nandyal Road, Kurnool, Andhra Pradesh, India.
3Professor, Department of Oral and Maxillofacial Pathology, G.Pulla Reddy Dental College. GPR Nagar, Nandyal Road, Kurnool, Andhra Pradesh, India.
4Reader, Department of Oral and Maxillofacial Pathology, G.Pulla Reddy Dental College. GPR Nagar, Nandyal Road, Kurnool, Andhra Pradesh, India.
5Post Graduate Student, Department of Oral and Maxillofacial Pathology, G.Pulla Reddy Dental College. GPR Nagar, Nandyal Road, Kurnool, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pavani Vidhyadhari, G. Pulla Reddy Dental College, GPR Nagar, Nandyal Road, Kurnool, Andhra Pradesh, India. Phone : 9581100699,
E-mail: Pavani.vidhyadhari31@ gmail.com
The fibro osseous lesions of the jaws represent a diverse group of entities that are characterized by replacement of normal bone by a fibrous connective tissue matrix, with in which varying amounts of osteoid, immature and mature bone and in some instances, cementum like material are deposited. Fibro osseous lesions of the jaws include developmental (hamartomatous) lesions, reactive or dysplastic processes and neoplasms. Juvenile ossifying fibroma (JOF) is a unique fibro osseous neoplasm. It has 2 histopathological variants (1) Trabecular juvenile ossifying fibroma (TrJOF) and (2) Psammomatoid juvenile ossifying fibroma (PsJOF) with TrJOF affecting the jaws of children. Only 20% of the patients are over 15 years of age. JOF is more common in maxilla than mandible. Origin in extragnathic locations is extremely rare. It presents as an asymptomatic progressive, rapid expansion of jaws. Radiographically, tumour is well circumscribed, along with lack of continuity with adjacent bone, cortical expansion & perforation. Histopathologically it consists of a cell rich fibrous stroma with bundles of cellular osteoid and bone trabeculae without osteoblastic rimming, and aggregates of giant cells. It has a recurrence rate of 30-58%. Long standing lesions shows cystic changes. Aneurysmal bone cyst is the most common complication. Here we present a case report of 16 yr old female patient with clinical, radiographic & histopathological features of Trabecular JOF with Aneurysmal bone cyst.
Aneurysmal bone cyst, Juvenile ossifying fibroma, Psammomatoid juvenile ossifying fibroma, Trabecular juvenile ossifying fibroma
Case Report
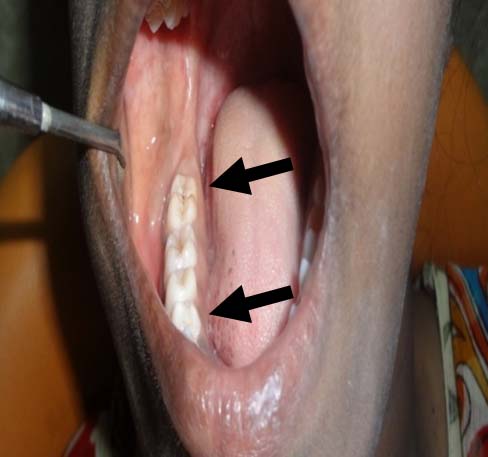
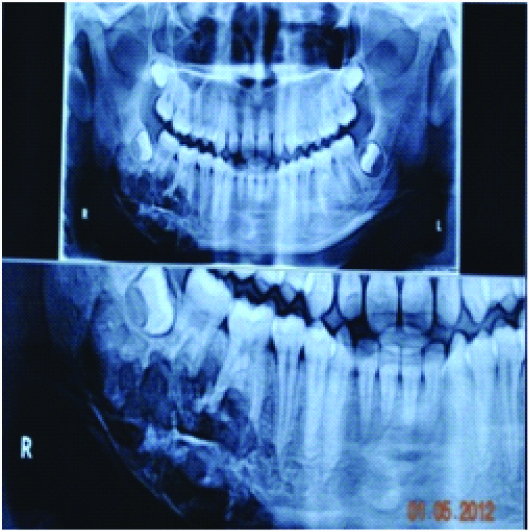
A 16-year-old female patient of presented with an asymptomatic swelling on lower right posterior region of the mandible, since 4 months [Table/Fig-1]. The swelling was extending anterioposteriorly 3cms from the corner of the mouth to beyond angle of the mandible and superiorly the swelling was not well delineated extending inferiorly beyond the base of the mandible. The Overlying skin was intact and on palpation the swelling was hard in consistency and temperature of overlying skin was not elevated. Intra oral examination showed unicortical expansion of mandible extending from mesial surface of 46 to distal surface of partially erupted 48 on lingual side, extending to the base of mandible [Table/Fig-2]. On palpation the swelling was hard and smooth. Panaromic radiograph revealed a well defined multilocular (soap bubble appearence) radiolucency in right body of mandible extending from 45 to angle of mandible measuring 3X5 cm with the thinning and expansion of lower body of mandible. Resorption of roots of first and second molars was also noted [Table/Fig-3].
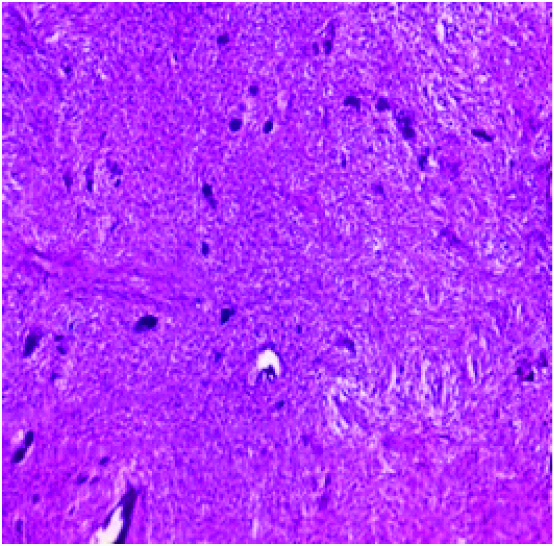
Provisional diagnosis was given as Ameloblastoma and differential diagnosis was given as Central cemento ossifying fibroma and Fibrous dysplasia. Initially an incisional biopsy was performed and the histological sections revealed fibro cellular stroma with numerous plump fibroblast with vesicular nuclei and cementum like calcifications [Table/Fig-4]. The final diagnosis was given as cement-ossifying fibroma. Later hemi-mandibulectomy was done from 45 to angle of the mandible on right side. When the grossing specimen was cut cystic spaces were evident [Table/Fig-5]. Multiple sections were made from various regions of the mandible for histological examination.
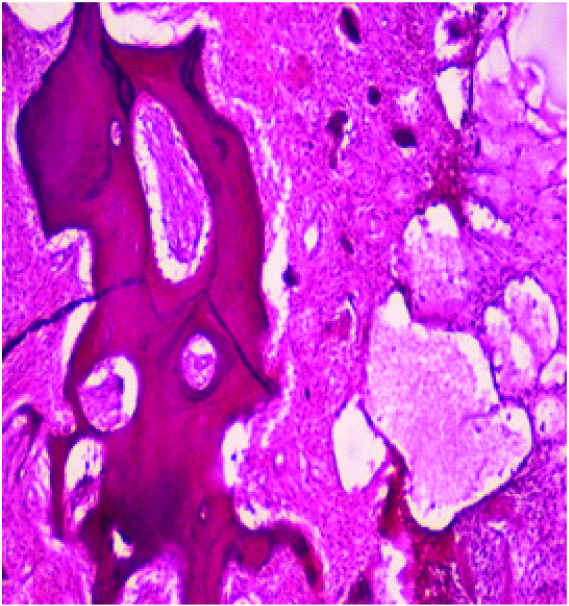
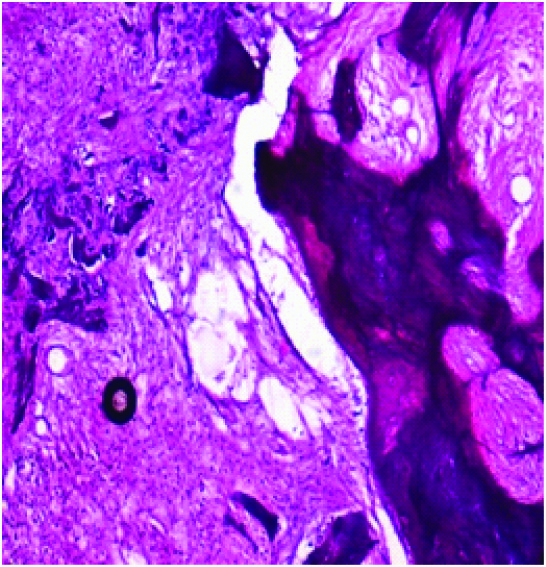
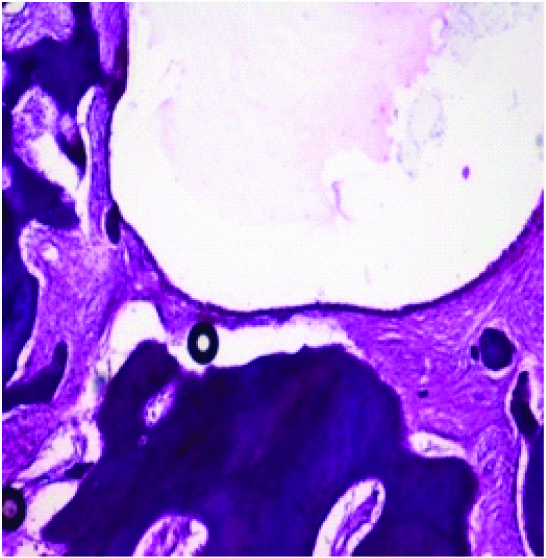
Histological examination of multiple sections from the specimen revealed highly cellular fibrous stroma with numerous plump fibroblast with vesicular nuclei & cementum like calcifications, reactive woven bone and mature bone with osteoblast rimming [Table/Fig-6,7]. Some of the sections showed multiple degenerative locules [Table/Fig-8]. The diagnosis was confirmed as Trabecular Juvenile ossifying Fibroma with Aneurysmal bone cyst. Hemimandibulectomy was the treatment done and the patient was symptomless in a follow up of 2 years.
Discussion
Benign fibro-osseous lesions of craniofacial complex are represented by a variety disease processes that are characterized by pathologic ossifications and calcifications in association with a hypercellular fibroblastic marrow element [1] . These lesions include fibrous dysplasia (FD), Ossifying fibroma (OF) and cement-osseous dysplasia (COD). OF is further divided into conventional and juvenile ossifying fibroma (JOF) [2] . JOF is distinguished from larger group of OF on the basis of age of the patients, most common site of involvement and clinical behaviour [3] . WHO in classification of odontogenic tumours (2005) defined JOF “as an actively growing lesion well demarcated from surrounding bone that is composed of cell rich fibrous tissue containing bundles of cellular osteoiod and bony trabeculae without osteoblastic rimming. Giant cells may also be present” The lesion is nonencapsulated but well demarcated from surrounding bone [1,4] . Compared to conventional ossifying fibroma, JOF is characterized by early age of onset that is under 15years of age, location of tumour, rapid growth, radiological appearance and tendency to recur [5] . Most of the features in the present case were consistant with that described in the literature like age of the patient, rapid growth that is within aduration of 4 months, radiographic features and histological features.
Two histological varients of JOF were reported, one which fulfills criteria described by WHO is designated as trabecular JOF or WHO type. Those characterized by the presence of a fibrocellular stroma containing ossicles resembling psammoma bodies have been designated as Psammomatoid JOF [2,4] . TrJOF most commonly affects jaws where as PsJOF is extragnathic. Histopathologically TrJOF is characterized by presence of trabeculae of fibrillar osteoid, woven bone and PsJOF by presence of small uniform spherical ossicles that resemble psammoma bodies [3,5] . The aneurysmal bone cyst is an expansile osteolytic lesion, often multilocular, with blood-filled spaces separated by fibrous septa containing osteoclast-type giant cells and reactive bone. It usually affects the long bones. In the jaws, it is more often found in the mandible, predominantly in the posterior regions, and is more common in the second to third decades of life. Aneurysmal bone cyst can develop as a secondary change in number of benign and malignant bone lesions [6,7] Johnson et al., commented that large aggressive maxillary lesions were commonly associated with aneurysmal bone cyst formation [7,3] .
The histogenesis of this lesion is poorly understood. Johnson et al., believe that mandibular lesions arise from the myxoid dental papilla of the developing tooth. Virtanen et al., consider JOF as a neoplasm that develops from the undifferentiated cells of the periodontal ligament [8] , or from a primitive mesenchymal cell nest or from cells remaining after incomplete migration of medial part of nasal anlage [9] .
Most of the cases reported in the literature were PsJOF of maxilla or paranasal sinuses and aneuryamal bone cyst was associated with extragnathic PsJOF. The features in the present case were correlating with that presented by Carolina Amalia Barcellos Silva et al.,[7] , Bhavani S.N et al., [10] which were showing the same features as Tr JOF of mandible with aneurysmal bone cyst in a female patients. The case reported by CEE Noffke [11] was 8 year follow-up of a 4year old boy who refused treatment initially, that showed progression of the lesion almost double the size of the initial lesion along with aneurismal bone cyst formation in a course of 7 years.
The aggressiveness of the JOF along with high rates of recurrences, (30-58%) [3,8,12] suggests that JOF should be treated like a locally aggressive neoplasm. For smaller lesions complete excision or through curettage is adequate [2,3,8] . En block resection is the treatment of choice for aggressive lesions [5,10] , which was the treatment of choice in the present case. If adequate surgical treatment is not done, Jof has very high rate of recurrence and recurrences are mostly seen in early stage which are more aggressive than primary [5] . Recurrence occurs after a period ranging from 6months to 19 years, so long term follow up is needed [2] .
Photograph showing swelling on right posterior region of the mandible.

Intra-oral view of the lesion
OPG showing multilocular radiolucency on right mandible
H&E section showing fibro cellular stroma
Grossing specimen with cystic spaces

H&E section showing cystic spaces with dense fibrous stroma and osteoid with osteoblastic rimming (10X magnification
Section showing dense fibrous stroma along with trabeculae and small degenerative locules
H&E section showing cystic spaces and osteoid (10X magnification).
Conclusion
JOF are uncommon lesions which need to be recognized in early stages and should be managed appropriately. Long term follow up should be needed as recurrences can be seen even after 10-15 years.
[1]. Eversole Roy, Su Lan, ElMofty Samir, Benign Fibro-Osseous Lesions of the Craniofacial Complex A ReviewHead and Neck Pathol. 2008 2:177-202. [Google Scholar]
[2]. Sarode Sachin C., Sarode Gargi S., Waknis Pushkar, Patil Anuprita, Jashika M., Juvenile psammomatoid ossifying fibroma:A review Oral Oncology 2011 47:1110-16. [Google Scholar]
[3]. Neville , Damm , Allen , Bouquot , Oral and maxillofacial pathology 2009 3rd EditionNoida, India,Elsevier Publications. [Google Scholar]
[4]. Kubbi Jithender Reddy, K Navadeepak Kumar, Reddy Vivekanandh, G Ramlal, Juvenile Ossifying Fibroma.Journal of Dental Sciences and Research.2(2):1-5. [Google Scholar]
[5]. Keles Bahar, Duran Mutlu, Uyar Yavuz, Azimov Ahmet, Demirkan Abdullah, Esen Haci Hasan, Juvenile Ossifying Fibroma of the Mandible. A case reportJ Oral Maxillofac Res. 2010 1():e5 [Google Scholar]
[6]. Nasser Munir J, Shawarbi Mohamed, Hybrid psammomatoid ossifying fibroma & aneurysmal bone cyst of frontal sinus.Pan arab journal of neurosurgery. 2010 14(1) [Google Scholar]
[7]. Silva Carolina Amalia Barcellos, Silva Alessandra Dutra, Araújo José Antonio de Carvalho, Araújo Ney Soares de, Furuse Cristiane, Trabecular Juvenile Ossifying Fibroma With Aneurysmal Bone Cyst: A Rare Presentation;Pediatric dentistry 2002 33:5-11. [Google Scholar]
[8]. R Ravikumar, K Raghavendra, Kumar Santhosh, Aggressive Juvenile Ossifying Fibroma of the Anterior Mandible.Journal of Dental Sciences and Research. 2011 2(1) [Google Scholar]
[9]. F Samantha F., Newman Laurence, M.Walker Donald, Papadopoulos Harry, Juvenile Aggressive Psammomatoid Ossifying Fibroma. An Interesting, Challenging, and Unusual Case Report and Review of the literature.Journal of oral and maxillofacial surgery. 2009 67(1):200-06. [Google Scholar]
[10]. S.N Bhavani, Rajesh A., Reddy Narendranatha, Kamal Firoz, Mandibular Aneurysmal Bone Cyst Associated with Cemento- ossifying Fibroma.Journal of clinical and diagnostic research 2013 7(12):3092-93. [Google Scholar]
[11]. Noffke CEE, Su Lan, ElMofty Samir, Juvenile ossifying ®broma of the mandible. An 8 year radiological follow-up.Dentomaxillofacial Radiology. 1998 27:363-66. [Google Scholar]
[12]. Chrcanovic Bruno Ramos, Freire-Maia Belini, An expanded juvenile ossifying fibroma in maxillary sinus. A case report.Korean Assoc Oral Maxillofac Surg. 2011 37:127-32. [Google Scholar]