Chair Side Application of NovaMin for the Treatment of Dentinal Hypersensitivity- A Novel Technique
Shivaprasad BM1, Padmavati P2, Nehal N Sanghani3
1 Reader, Department of Periodontology, Rajarajeswari Dental College and Hospital, Bangalore, India.
2 Postgraduate Student, Department of Periodontology, Rajarajeswari Dental College and Hospital, Bangalore, India.
3 Postgraduate Student, Department of Periodontology, Rajarajeswari Dental College and Hospital, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shivaprasad BM, Reader, Department of Periodontology, Rajarajeswari Dental College and Hospital, Bangalore, Karnataka state, India. Phone : 9538104242, E-mail : drshivaprasad2008@yahoo.co.in
Objective: To evaluate the efficacy of calcium sodium phosphosilicate bioactive glass (NovaMin) as a chair side desensitizing agent.
Materials and Methods: The study was conducted on 60 subjects divided into 3 groups of 20 each as follows. Group I (NovaMin application without scaling and root planing), Group II (NovaMin application after scaling and root planing) and Group III (control group). Sensitivity was assessed using air blast and cold water stimulus at baseline, immediately after application, after half an hour and after 8d using Visual Analog Scale (VAS).
Results: Mean VAS (air blast stimulus) for group I was 5.9 at baseline, 3.4 immediately after application, 3.05 after half an hour, and 3.0 after 8 days. In group II VAS score were 6.2, 3.35, 2.9, 2.75 and group III 6.6, 7.0, 7.0, 7.0 respectively. For cold water stimulus in group I VAS score were 5.6, 3.35, 3.15, 3.1, group II VAS score 5.7, 3.35, 3.1, 2.85 and group III 5.8, 6.1, 6.05, 6.05 respectively. VAS scores in between group I and group III and group II and group III were statistically significant (<0.001) immediately after application, after half an hour and after 8days (ANOVA).
Conclusion: Chair side application of calcium phosphosilicate bioactive glass can be a therapeutic adjunct to provide immediate relief for the patient with dentinal hypersensitivity.
Dentinal hypersensitivity, Calcium sodium phosphosilicate bioactive Glass, Desensitizing agents
Introduction
Dentine hypersensitivity is characterized by short, sharp pain arising from exposed dentine in response to stimuli typically thermal, evaporative, tactile, osmotic or chemical and which cannot be ascribed to any other form of dental defect or pathology [1,2]. Dentine may become exposed because of several reasons, viz., attrition, abrasion, erosion, or gingival recession [3]. The role of plaque in the etiology of dentine hypersensitivity is unclear but it can play an indirect role on periodontal tissues [4,5].
The reported prevalence of dentine hypersensitivity (DH) varies from 4 to 57 percent [6,7]. These variations are likely due to differences in the populations studied and the methods of investigation (for example, questionnaires or clinical examinations). The prevalence of DH is between 60 and 98 percent in patients with perioodontitis [8] and mostly occurs in patients who are aged between 20 and 40 years [9].
A number of theories have been proposed over the years to explain the pain mechanism of dentinal hypersensitivity. An early hypothesis was the dentinal receptor mechanism theory which suggests that dentine hypersensitivity is caused by the direct stimulation of sensory nerve endings in dentine [10]. Also, odontoblast transducer mechanism theory proposed by Rapp et al.,[11] suggested that odontoblasts act as receptor cells, mediating changes in the membrane potential of the odontoblasts via synaptic junctions with nerves. The currently accepted hypothesis is the hydrodynamic theory which states that dentine hypersensitivity may be caused by movement of the dentinal tubule contents [12].
Many methods have been used for the clinical treatment of hypersensitive dentine [13,14].
In-office methods provide an advantage over home use of desensitizing agents as they do not require multiple applications, patient compliance is not required and higher concentration of the desensitizing agent can be used that provides better relief from sensitivity. The present study focuses on a method of in-office chair side desensitization using Nova Min. NovaMin is the trade name for a calcium sodium phosphosilicate bioactive glass that has been developed for use in oral health care [23]. NovaMin precipitates calcium and phosphate and has been used to decrease hypersensitivity by occluding exposed dentinal tubules [24]. The mode of action of this material results from interactions with aqueous solutions, when introduced into the oral environment, the material releases sodium, calcium, and phosphate ions, which then interacts with oral fluids and result in the formation of a crystalline hydroxycarbonate apatite (HCA) layer that is structurally and chemically similar to natural tooth mineral [24].
In- Office Agents At- Home Agents
Iontophoresis with 2% sodium Desensitizing toothpastes/dentifrices
fluoride [15] [13,14] containing strontium salts,
fluorides, formaldehyde, potassium salts like
potassium nitrate [16], potassium chloride
or potassium citrate [17]
Nova Min Mouthwashes containing potassium nitrate
and sodium fluoride [18,19],
potassium citrate or sodium fluoride [20]
or a mixture of fluorides [21]
5% sodium fluoride varnish Chewing gum containing potassium
Laser chloride [22]
The only study reported till now with the use of NovaMin powder with NovaMin-containing toothpaste showed significant hypersensitivity reduction over baseline at all time points [25]. Therefore, the present study was conducted with the objective of evaluating the efficacy of chair side application of NovaMin for reduction of hypersensitivity.
Materials and Methods
The present study was a randomized, controlled, single site and double masked clinical trial. The study was conducted from August 2012 to November 2012 and the population was selected randomly from patients attending the outpatient section of the Department of Periodontics, Rajarajeswari Dental College and Hospital, Bangalore, India. Each participant received a detailed explanation regarding the study procedure, and written informed consent was obtained. Ethical clearance certificate was obtained by institutional ethical review board. Study was conducted in accordance with the Helsinki declaration (2008).
Criteria for Selection
A total of 60 subjects in good systemic health and with hypersensitive teeth either due to wasting disease (attrition, abrasion, erosion) diagnosed as per Tooth Wear Index [26] or due to denudation of the root caused by periodontitis were selected. The following factors should exclude subjects or teeth from the study; current desensitizing therapy; allergies and idiosyncratic responses to product ingredients; excessive dietary or environmental exposure to acids; teeth with restorations like glass ionomer cement, composite etc; subjects with cervical abrasion in whom alternative modes of treatment has been planned; teeth with fluorosis and enamel hypoplasia.
Methodology
Study population consisted of 60 patients divided into the 3 groups of 20 patients each.
Group I- Chair side application of NovaMin (without scaling & root planing)
Group II- Chair side application of NovaMin (after scaling & root planing)
Group III- Control group (no application of desensitizing agent, NovaMin)
Group II NovaMin was applied after scaling and root planing, to know if the removal of the smear layer would increase the penetration of calcium sodium phosphosilicate bioactive glass.
Testing
Two different stimuli were employed, air evaporative and cold water both of which are relevant to the everyday initiation of sensitivity in subjects. The cold air stimulus was approximately a 1-second blast from the air syringe of the dental unit. The cold air was directed at the exposed surface of the selected tooth that was isolated mesially and distally from adjacent teeth with the investigator’s fingers [27]. The response to sensitivity for both the groups for air pressure and for cold water stimulus was noted. The assessment methods were response based using a Visual analog scale (VAS) score [28] completed by the subject rather than a stimulus-based binary response using stimuli of increasing intensity.
Group I patients were treated with NovaMin powder without scaling and root planing. VAS was noted at baseline. NovaMin powder was mixed with distilled water and the paste prepared was applied with a small cotton pledget to the tooth surface, left for two minutes and then rinsed off. Group II patients were treated with NovaMin powder after scaling and root planing. The reason as to why these subjects were divided into group I and group II was to know if the removal of the smear layer after scaling and root planning would increase the penetration of calcium sodium phosphosilicate bioactive glass and provide better relief from sensitivity and another reason being that scaling itself can increase the sensitivity to some extent.
After application of NovaMin, severity of sensitivity was assessed immediately after application, after half an hour and 8 days using Visual Analog Scale.
Statistical analysis included mean, standard deviation, standard error which was calculated for each of the test groups. Analysis of variance (ANOVA) was used to determine the intergroup and intragroup comparisons. Significance for all the tests was pre-determined at a probability value of <0.05.
Results
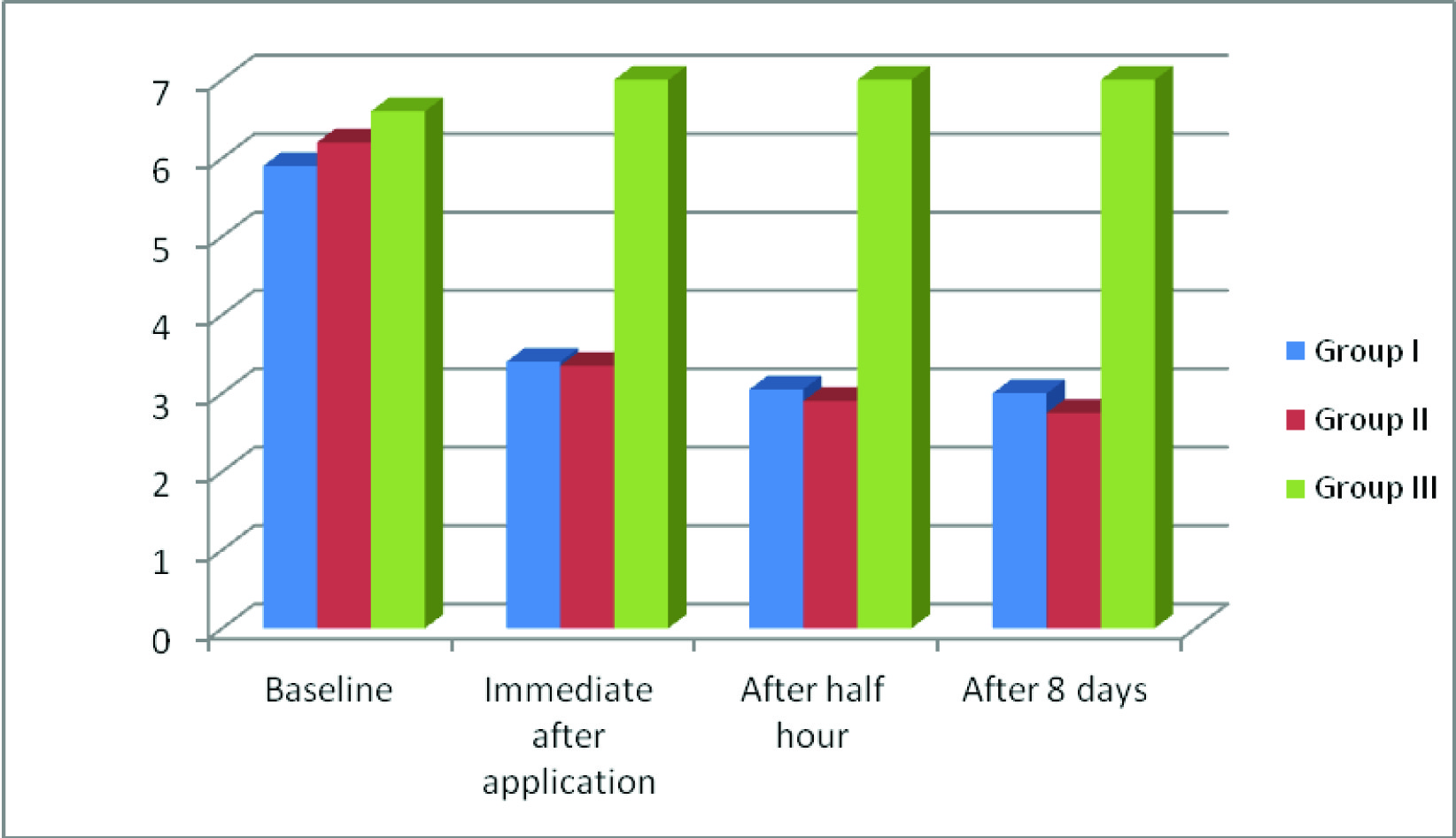
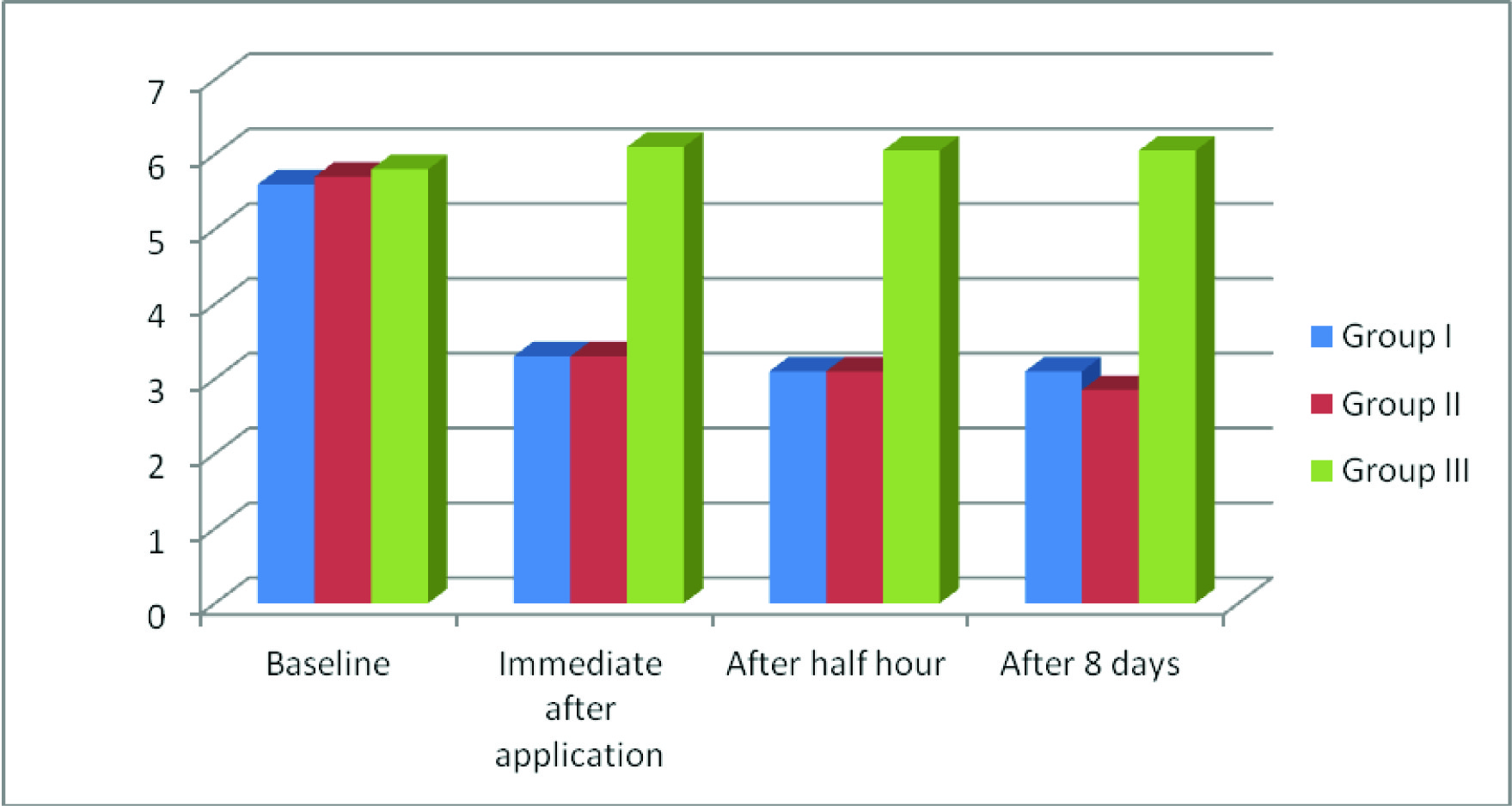
The present randomized controlled trial was conducted on a total of 60 subjects who were selected after considering the inclusion and exclusion criteria. Sixty subjects were divided into 3 groups of 20 each. The mean VAS score for air blast and cold water test are presented in [Table/Fig-1,2,3,4,5and6]. Intergroup comparisons are presented in [Table/Fig-7,8].
Mean, SD of dentinal hypersensitivity at baseline, immediate after application, after half hour and after 8 days obtained by air blast test
| Group A | N* | Mean | Standard deviation (SD) |
|---|
| Baseline | Group I | 20 | 5.90 | 1.11 |
| Group II | 20 | 6.20 | 1.00 |
| Group III | 20 | 6.60 | 1.09 |
| Immediate after application | Group I | 20 | 3.40 | 0.82 |
| Group II | 20 | 3.35 | 0.93 |
| Group III | 20 | 7.0 | 1.12 |
| After half hour | Group I | 20 | 3.05 | 0.68 |
| Group II | 20 | 2.90 | 0.85 |
| Group III | 20 | 7.0 | 1.12 |
| After 8 days | Group I | 20 | 3.0 | 0.64 |
| Group II | 20 | 2.75 | 0.85 |
| Group III | 20 | 7.0 | 1.12 |
*N= sample size
Mean, SD of dentinal hypersensitivity at baseline, immediate after application, after half hour and after 8 days obtained by cold water test
| Group A | N* | Mean | Standard deviation (SD) |
|---|
| Baseline | Group I | 20 | 5.6 | 1.18 |
| Group II | 20 | 5.7 | 1.03 |
| Group III | 20 | 5.8 | 0.98 |
| Immediate after application | Group I | 20 | 3.3 | 0.81 |
| Group II | 20 | 3.3 | 0.81 |
| Group III | 20 | 6.1 | 1.16 |
| After half hour | Group I | 20 | 3.1 | 0.81 |
| Group II | 20 | 3.1 | 0.78 |
| Group III | 20 | 6.05 | 1.09 |
| After 8 days | Group I | 20 | 3.1 | 0.78 |
| Group II | 20 | 2.85 | 0.81 |
| Group III | 20 | 6.05 | 1.09 |
* significant
Mean VAS score of dentinal hypersensitivity at baseline, immediate after application, after half hour and after 8 days obtained by air blast test
Profile plots for air blast test
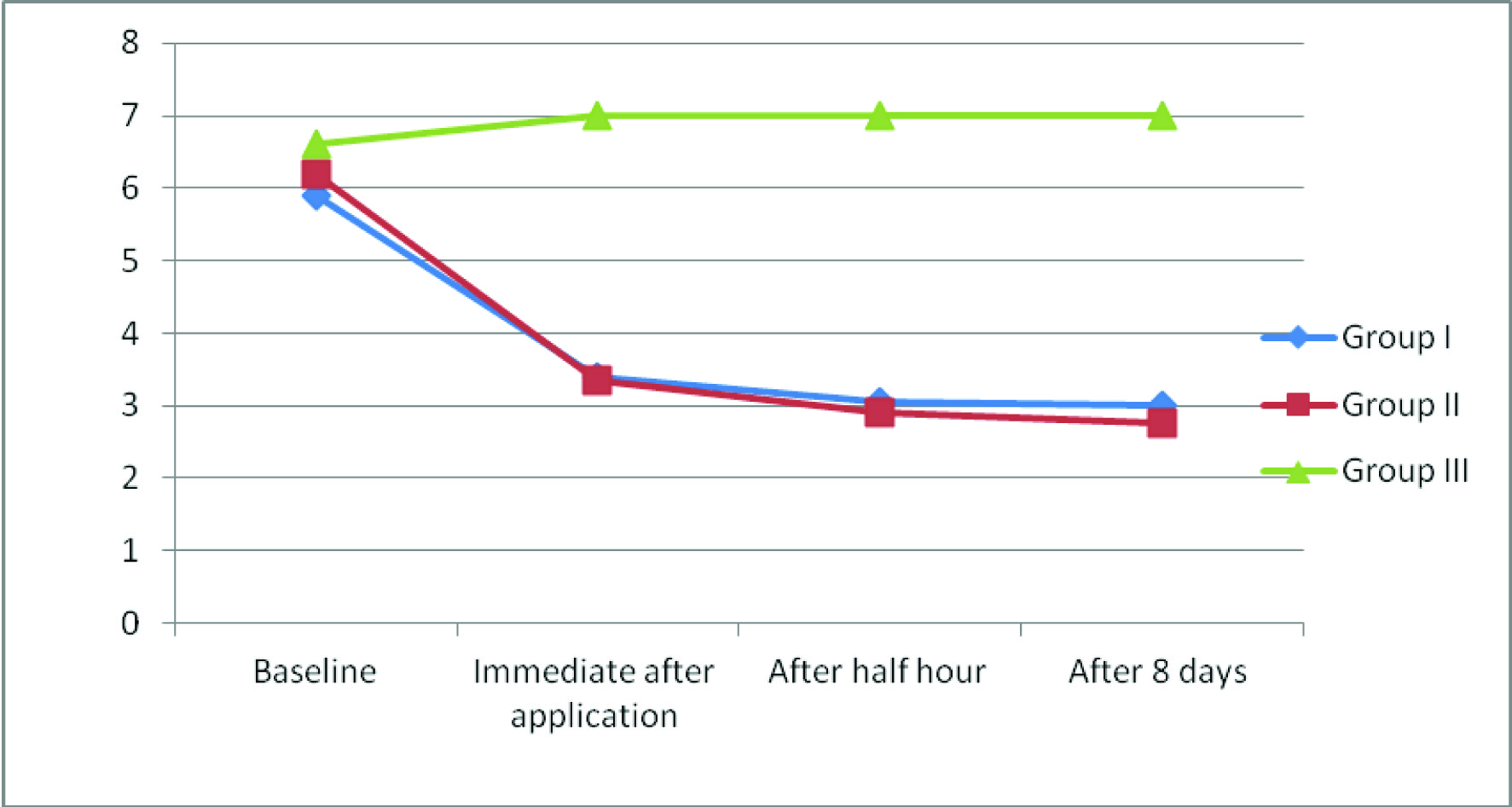
Mean VAS score for air blast stimulus before and after application of NovaMin were as follows. In group I it was 5.9 at baseline without scaling and root planing, 3.4 immediately after application, 3.05 after half an hour, and 3.0 after 8 days [Table/Fig-1,3]. In group II i.e. after scaling and root planing VAS score at baseline, immediate after application, after half an hour and after 8 days were 6.2, 3.35, 2.9, 2.75 respectively [Table/Fig-1,3]. Overall, there was an improvement in symptoms of hypersensitivity from baseline to day 8 in both group I and group II whereas in group III there was no decrease in the VAS scores from baseline over a period of 8 days.
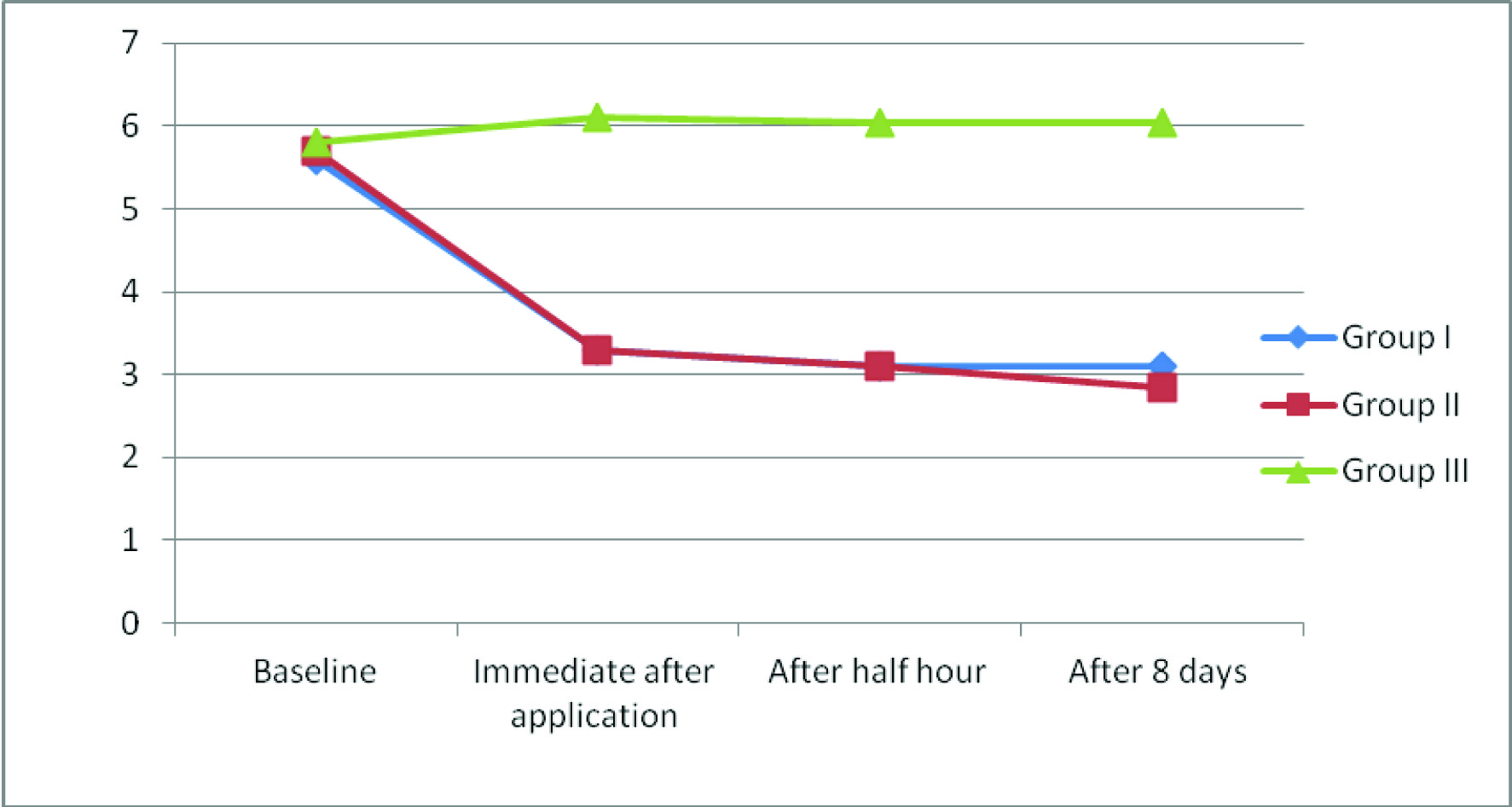
Similarly, the mean VAS score for cold water stimulus before and after application of NovaMin are provided in [Table/Fig-2, 5]. Overall, there was an improvement in symptoms from baseline to day 8 in both group I and group II. In group III there was no decrease in the VAS scores from baseline over a period of 8 days.
Mean VAS score of dentinal hypersensitivity at baseline, immediate after application, after half hour and after 8 days obtained by cold water test
VAS scores in between group I and group III and between group II and group III were statistically significant <0.001 immediately after application, after half an hour and after 8 days [Table/Fig-4,6–8].
Profile plots for cold water test
Inter group comparison of sensitivity by air blast test using ANOVA
| | Sum of squares | Df† | Mean square | F | p-value |
|---|
| Baseline | Between groups Within groups | 4.9 65.8 | 2 57 | 2.46 1.15 | 2.13 | 0.127 |
| Immediate after application | Between groups Within groups | 175.2 53.3 | 2 57 | 87.6 0.9 | 93.6 | <0.001* |
| After half hour | Between groups Within groups | 216.2 46.7 | 2 57 | 108.1 0.8 | 131.8 | <0.001* |
| After 8 days | Between groups Within groups | 227.5 45.7 | 2 57 | 113.7 0.8 | 141.7 | <0.001* |
*significant ; † degrees of freedom
Inter group comparison of sensitivity by cold water test using ANOVA
| | Sum of squares | Df† | Mean square | F | p-value |
|---|
| Baseline | Between groups Within groups | 0.63 65.5 | 2 57 | 0.317 1.15 | 0.275 | 0.76 |
| Immediate after application | Between groups Within groups | 100.8 50.9 | 2 57 | 50.41 0.89 | 56.45 | <0.001* |
| After half hour | Between groups Within groups | 114.1 47.3 | 2 57 | 57.05 0.83 | 68.74 | <0.001* |
| After 8 days | Between groups Within groups | 126.7 47.3 | 2 57 | 63.35 0.83 | 76.34 | <0.001* |
Discussion
Hypersensitivity results when dentin is exposed due to one of the two processes; either removal of the enamel from the crown of the tooth, or denudation of the root surface by loss of cementum and overlying periodontal tissues. Most of the therapeutic modalities proposed to date depend on one of the two major suppressive mechanisms: sealing (blocking) of the dentinal tubule opening or dampening neural impulses.
Interpretation of pain as elicited by visual analog scale (VAS) after single application of NovaMin showed decrease in hypersensitivity immediately after application in group I and II. Group I showed a mean decrease in sensitivity from 5.9 at baseline to 3.4 after the application of NovaMin. On the other hand group II showed a decrease from 6.2 at baseline to 3.35 after application. There was no difference to pain response in the control group III, mean VAS score at baseline noted was 6.6 which remained the same throughout the eight day period.
Reduction in sensitivity in group I and II was due to the penetration of NovaMin into the dentinal tubules which resulted in the occlusion of tubules. In aqueous environments, such as saliva, the sodium ions (Na+) in calcium sodium phosphosilicate particles immediately (within one minute) begin to exchange with hydrogen cations (H+ or H3O+). This rapid exchange of ions allows calcium (Ca2+) and phosphate (PO4) species to be released from the particle structure. A modest localized, transient increase in pH occurs that facilitates the precipitation of calcium and phosphate from the particles and from saliva to form a calcium phosphate (Ca-P) layer on tooth surfaces. As the reactions and the deposition of Ca-P complexes continue, this layer crystallizes into hydroxycarbonate apatite (HCA), which is chemically and structurally similar to biological apatite. The combination of the residual calcium sodium phosphosilicate particles and the HCA layer results in the physical occlusion of dentinal tubules, which will relieve hypersensitivity [23].
Early clinical studies demonstrated that a dentifrice containing NovaMin significantly improves oral health as measured by a reduction in gingival bleeding and reduction in supragingival plaque compared with a negative dentifrice over the six weeks study period [29].
The efficacy of a dentifrice containing calcium sodium phosphosilicate (NovaMin) versus a placebo and a commercially-available strontium chloride (SrCl2) containing dentifrice was evaluated for the treatment of dentin hypersensitivity showed the percent reduction in sensitivity at six weeks for the NovaMin test group was higher than placebo and SrCl2 group [30]. Another NovaMin Research Report compared the use of DenShield (NovaMin) with GC Tooth Mousse (Recaldent) on bovine root surfaces in a pH-cycling model. After 10days, the number of occluded dentinal tubules was greater with the DenShield product than with the Tooth Mousse. This was determined by SEM evaluation and the counting of occluded tubules [31]. A very recent in vitro study evaluated the effect of NovaMin desensitising toothpaste mixed with 15% carbamide peroxide on tooth bleaching and tubule occlusion. It was found that the addition of NovaMin to 15% Carbamide peroxide occluded the dentinal tubules and that it did not affect the bleaching procedure. They also emphasized its clinical relevance in a dual advantage of desensitizing and bleaching with a single paste system [32]. Recent studies have also demonstrated a potential for NovaMin to prevent demineralization and/or aid in remineralization of white-spot lesions [23].
Reviewing the literature many clinical trials have used NovaMin in dentifrices [23, 29–32], but very little data is available on application of NovaMin powder directly to tooth structure to relieve dentin hypersensitivity. The use of other desensitizing agents in dentifrices needs frequent applications and use of laser equipment is expensive and requires skilled personnel. It requires repeated application and maintenance of excellent quality of home care to achieve the therapeutic results. To overcome the shortcomings, this study attempted to measure the chairside application of NovaMin powder for the management of dentin hypersensitivity. NovaMin is the new product available in the market and has an added advantage of chair-side application.
Conclusion
Dentinal hypersensitivity is a relatively common and significant dental problem which can be successfully managed by a very wide variety of procedures, agents and formulations applied locally, either “in office i.e. chairside” or “at home”. This was an in-office procedure and proved to be a therapeutic adjunct to provide rapid precipitation and blocking of tubules and filling in of surface defects with NovaMin, and providing immediate relief for the patient with hypersensitive teeth. Future studies with more sample size carried in different parts of world will authenticate the use of NovaMin as chair side desensitizing agent.
*N= sample size
* significant
*significant ; † degrees of freedom
[1]. Orchardson R, Collins W, Clinical features of hypersensitive teethBr Dent J 1987 162:253-56. [Google Scholar]
[2]. Addy M, Clinical aspects of dentine hypersensitivityProc Finn Dent Soc 1992 88:407-12. [Google Scholar]
[3]. Bartold PM, Dentinal hypersensitivity: a reviewAust Dent J 2006 51(3):212-18. [Google Scholar]
[4]. Addy M, Mostafa P, Newcombe RG, Dentine hypersensitivity: The distribution of recession, sensitivity and plaqueJ Dent 1987 15:242-48. [Google Scholar]
[5]. Alexander A.G, A study of the distribution of supra and subgingivai calculus, bacterial plaque and gingival inflammation in the mouths of 400 individualsJ Periodontol 1971 59:222-28. [Google Scholar]
[6]. Rees JS, Addy M, A cross-sectional study of dentine hypersensitivityJ Clin Periodontol 2002 29:997-1003. [Google Scholar]
[7]. Irwin CR, McCusker P, Prevalence of dentine hypersensitivity in a general dental populationJ Ir Dent Assoc 1997 43(1):7-9. [Google Scholar]
[8]. Chabanski MB, Gillam DG, Bulman JS, Newman HN, Prevalence of cervical dentine sensitivity in a population of patients referred to a specialist periodontology departmentJ Clin Periodontol 1996 23:989-92. [Google Scholar]
[9]. Graf HE, Galasse R, Morbidity, prevalence and intra-oral distribution of hypersensitive teethJ Dent Res 1977 (Special issue A, Abstract Number 479):56 [Google Scholar]
[10]. Irvine JH, Root surface sensitivity: a review of aetiology and managementJ New Zealand Soc Periodontol 1988 66:15-58. [Google Scholar]
[11]. Rapp R, Avery JK, Strachen DS, Possible role of the aceylcholinesterase in neural conduction within the dental pulpIn: Finn SB, editor. Biology of dental pulp organ 1968 BirminghamUniversity of Alabama Press:309 [Google Scholar]
[12]. Brannstrom M, A hydrodynamic mechanism in the transmission of pain-produced stimuli through the dentine. In: Anderson DJ, editorSensory mechanisms in dentine 1963 LondonPergamon Press:73-79. [Google Scholar]
[13]. Zappa U, Self-applied treatments in the management of dentine hypresensitivityArch Oral Biol 1994 39:107S-12S. [Google Scholar]
[14]. Gangarosa L, P. Current strategies for dentist-applied treatment in the management of hypersensitive dentineArch of Oral Biol 1996 39:101-6S. [Google Scholar]
[15]. Mangalekar SB, More SP, Shetty RM, Oswal R, Prasad P, Sheikh S, Comparative assessment of efficacy of single application of dipotassium oxalate, Potassium nitrate and sodium fluoride with iontophoresis in the treatment of hypersensitive teeth: An in-vitro and in-vivo studyInt J Contemp Dent 2010 :60-67. [Google Scholar]
[16]. Tarbet WJ, Silverman G, Stolman JM, Fratarcangelo PA, Clinical evaluation of a new treatment for dentinal hypersensitivityJ Periodontol 1980 51:535-40. [Google Scholar]
[17]. Orchardson R, Gillam DG, The efficacy of potassium salts as agents for treating dentin hypersensitivityJ Orofac Pain 2000 14(1):9-19. [Google Scholar]
[18]. Gillam DG, Bulman JS, Jackson RJ, Newman HN, Efficacy of a potassium nitrate mouthwash in alleviating cervical dentine sensitivity (CDS)J Clin Periodontol 1996 23:993-97. [Google Scholar]
[19]. Pereira R, Chava VK, Efficacy of a 3% potassium nitrate desensitizing mouthwash in the treatment of dentinal hypersensitivityJ Periodontol 2001 72:1720-25. [Google Scholar]
[20]. Yates R, West N, Addy M, Marlow I, The effects of a potassium citrate, cetylpyridinium chloride, sodium fluoride mouthrinse on dentine hypersensitivity, plaque and gingivitis: a placebo controlled studyJ Clin Periodontol 1998 25:813-20. [Google Scholar]
[21]. Yates RJ, Newcombe RG, Addy M, Dentine hypersensitivity: a randomized, double-blind placebo-controlled study of the efficacy of a fluoride-sensitive teeth mouthrinseJ Clin Periodontol 2004 31:885-89. [Google Scholar]
[22]. Krahwinkel T, Theiss P, Willershausen B, Clinical effectiveness of a potassium chloride containing chewing gum in the treatment of hypersensitive teethEur J Med Res 2001 6:483-87. [Google Scholar]
[23]. Burwell AK, Litkowski LJ, Greenspan DC, Calcium Sodium Phosphosilicate (NovaMin): Remineralization PotentialAdv Dent Res 2009 21:35-9. [Google Scholar]
[24]. Wefel J.S, NovaMin: Likely Clinical SuccessAdv Dent Res 2009 21:40-43. [Google Scholar]
[25]. Narongdej T, Sakoolnamarka R, Boonroung T, The Effectiveness of a Calcium Sodium Phosphosilicate Desensitizer in Reducing Cervical Dentin HypersensitivityJ Am Dent Assoc 2010 141:8995-99. [Google Scholar]
[26]. Smith BGN, Knight JK, An Index for measuring the wear of teethBr Dent J 1984 156:435-38. [Google Scholar]
[27]. Tarbet WJ, Silverman G, Stolman JH, An evaluation of two methods for the quantification of dentinal hypersensitivityJ Am Dent Assoc 1979 98:914-18. [Google Scholar]
[28]. Clark GE, Troullos ES, Designing hypersensitivity clinical trialsDent Clin North Am 1990 34:531-44. [Google Scholar]
[29]. Tai BJ, Anti-gingivitis effect of a dentifrice containing bioactive glass (NovaMin) particulateJ Clin Periodontol 2006 33:86-91. [Google Scholar]
[30]. Du Min Q, Clinical evaluation of a dentifrice containing calcium sodium phosphosilicate (NovaMin) for the treatment of dentin hypersensitivityAn J Dent Res 2008 21:210-14. [Google Scholar]
[31]. Burwell A, Tubule occlusion of a NovaMin-containing dentifrice compared to Recaldent-containing dentifrice—a remin/demin study in vitroNovaMin Research Reports 2006 http://www.NovaMin.com [Google Scholar]
[32]. Kakodkar G, Lavania A, Ataide Ide N, An In vitro SEM study on the effect of bleaching gel enriched with NovaMin on whitening of teeth and dentinal tubule occlusionJ Clin Diagn Res 2013 7(12):3032-35. [Google Scholar]