Transient Patellar Dislocation Resulting in Simultaneous Osteochondral Fractures of Patella and Lateral Femoral Condyle – A Case Report
Divesh Jalan1, Vivek Machhindra Morey2, Ravi Mittal3, Chaitanya Dev Pannu4
1 Assistant Professor, Department of Orthopaedics, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
2 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India.
3 Additional Professor, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India.
4 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Divesh Jalan, House No.1038, Sector-4, Gurgaon -122001, Haryana, India. Phone : +918003996897, E-mail : dvsh_jalan@yahoo.com
Transient Patellar dislocations are commonly associated with bony contusions or osteochondral fractures involving the medial facet of patella or lateral femoral condyle. Simultaneous osteochondral fractures are rare and have not been reported in the adult. The authors report a case of combined osteochondral fracture of patella and lateral femoral condyle following acute patellar dislocation in an adult, which was misdiagnosed as meniscal injury. Both the osteochondral fracture fragments were rigidly fixed with headless compression screws and repair of the medial retinaculum was done. At latest follow up after two years, patient had regained full range of motion with no further episodes of patellar dislocation. The rarity of this combination of injury along with difficulty in interpreting radiographs makes this case interesting.
Lateral femoral condyle, Medial facet patella, Osteochondral fracture, Patellar dislocation
Case Report
A 30-year-old female presented to us with pain and swelling of the left knee following a fall on the knee two weeks back. Pain and swelling had decreased subsequently. Pain was aggravated on weight bearing and relieved with rest and medication. There was no history of locking or any instability of the knee.
On examination, there was mild effusion of the knee and tenderness was present over the lateral femoral condyle, medial surface of patella as well as over the medial joint line. Pain was also produced by posteriorly directed pressure on patella as well as on passive motion of the patella. There was loss of full extension. Anterior drawer, Lachmann and Mc murray tests were negative and there was no neurovascular deficit.
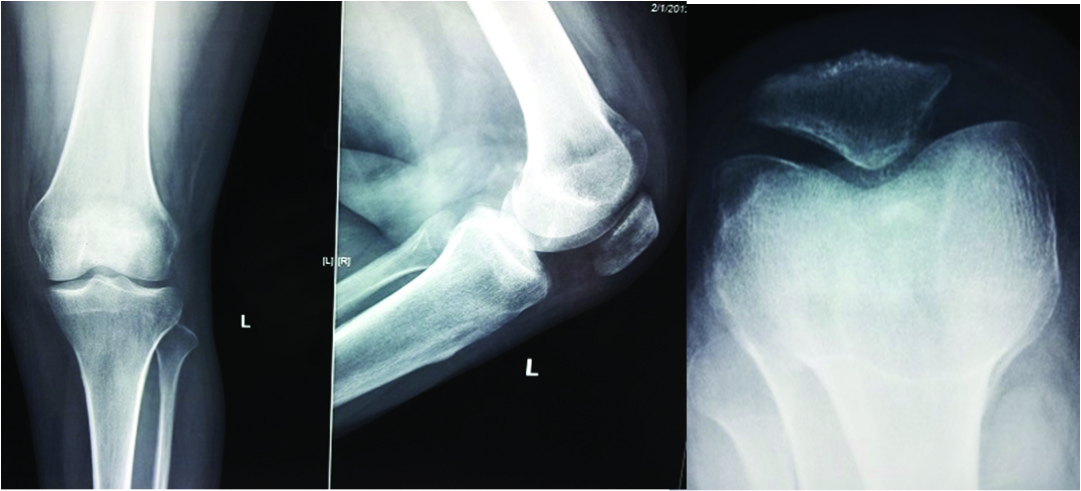
As the fragment was not clearly visible on the initial roentgenogram [Table/Fig-1], the diagnosis of medial meniscus tear with loose meniscal fragment in the knee joint was made based on clinical and MRI findings in another hospital. Patient came to us for a second opinion. On re-evaluation, we found a defect in the medial facet of patella along with the loose fragment which was further confirmed with computed tomography of the knee to be an osteochondral fragment [Table/Fig-2]. So, a final diagnosis of patellar dislocation with osteochondral fracture of patella was made.
Preoperative radiographs (anteroposterior, lateral and skyline view) of the left knee. A small radiopaque shadow can be seen posteriorly in the lateral view.
CT and MRI images (Axial and Sagittal) showing defect in the medial facet of patella along with patellar subluxation and tilt (suggestive of previous dislocation) and the loose osteochondral fragment lying in the intercondylar notch.

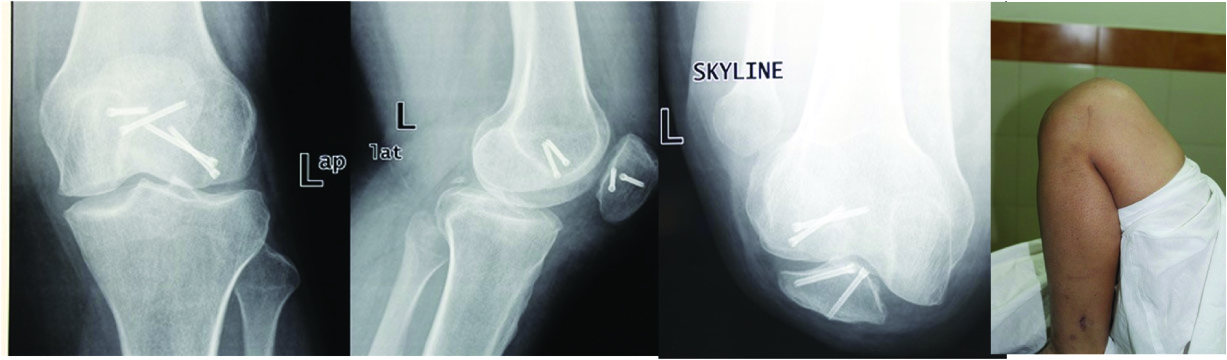
There were two treatment options, diagnostic arthroscopy to confirm the diagnosis and then proceed with internal fixation by arthrotomy or directly perform arthrotomy. We chose the second option as the diagnosis was confirmed. The medial parapatellar arthrotomy was done and an osteochondral fragment was identified in the notch. The patella was averted to expose the defect. A further search in the joint revealed another osteochodral fragment which found out to be arising from the lateral aspect of lateral femoral condyle [Table/Fig-3].Both the fracture beds were then debrided of all the fibro cartilage. The osteochondral fragments were then reduced and rigidly fixed with two headless compression screws in each fragment buried within the cartilage [Table/Fig-4]. Both the menisci and the ligaments were normal. After fixation, knee was brought through full range of motion with normal patellar tracking. The wound was closed after repair of the medial retinaculum to prevent further dislocation.
Osteochondral fragments from the patella and the lateral femoral condyle.

Osteochondral fragments fixed with 2 headless compression screws buried within the cartilage.

The patient made an uneventful recovery and regained full range of motion with no further episodes of patellar dislocation at two years [Table/Fig-5].
At 2 years, radiographs and the clinical picture shows healing of the osteochondral fractures with full range of knee motion.
Discussion
The combined osteochondral fracture of lateral femoral condyle and patella following acute patellar dislocation is rarely documented in orthopaedic literature. In majority of the studies, patellar osteochondral fracture is associated with a bony contusion involving the lateral femoral condyle in the classical impaction pattern of injury [1]. There are only two studies in which simultaneous osteochondral fractures of patella and lateral femoral condyle following patellar dislocation is reported in children and adolescents [2,3]. However, no case has been reported in the adult.
The exact reconstruction of the forces that caused the injury is often elusive because of the insensitivity of subchondral bone. Secondly, dislocation of patella is typically transient with spontaneous reduction so most of the patients like in our case are unaware that they have had lateral patellar dislocation.
Radiographic diagnoses of these fractures are often difficult and multiple projections are required along with strong clinical suspicion. Only 11 out of 48 radiographs could diagnose an osteochondral defect in a study by Stanitski et al., [4]. Computed tomography is occasionally useful however purely cartilaginous lesions may not be recognized. MRI can identify the ostechondral and chondral lesions in majority of the patients and recognize features which point towards previous dislocation like loss of medial retinacular integrity resulting in patellar tilt or subluxation which was also seen in our case. Diagnostic arthroscopy is also helpful in identifying these fractures and resultant defects. Fixation of the fragments, however, usually requires open approach.
Early diagnosis of these osteochondral fractures decides treatment as most of the studies reported open reduction and fixation of these fractures within two weeks and excision of the loose fragment was done thereafter [5–7]. Toupin et al., had emphasized that after a period of 10 d post-trauma, the osteochondral fragment volume increases and the fibrous tissue develops at the fracture site which may prevent proper reduction [8].
Because of the rarity of this combination of injury and the associated difficulty in identifying such injuries on radiographs, these are often missed and misdiagnosed, like in our case where it was being treated for meniscal injury. If the fracture remains untreated, it will predispose to early degenerative arthritis in these young individuals. Hence, the most important factor in preventing both the development of degenerative arthritis and loose bodies in these young individuals is early diagnosis and management.
Conclusion
Diagnosis of osteochondral fractures of the knee is often difficult because of the nonspecific history and clinical findings along with poor sensitivity of plain radiographs and computed tomography scans. So, a high index of suspicion is required along with MRI or arthroscopy to identify these fractures and the entire knee joint particularly lateral femoral condyle should be inspected to find out other associated injuries.
[1]. Sanders TG, Paruchuri NB, Zlatkin MB, MRI of Osteochondral Defects of the Lateral Femoral Condyle: Incidence and Pattern of Injury After Transient Lateral Dislocation of the PatellaAJR 2006 187:1332-37. [Google Scholar]
[2]. Rorabeck CH, Bobechko WP, Acute dislocation of the patella with osteochondral fracture: a review of eighteen casesJ Bone Joint Surg Br 1976 58:237-40. [Google Scholar]
[3]. Seeley MA, Knesek M, Vanderhave KL, Osteochondral injury after acute patellar dislocation in children and adolescentsJ Pediatr Orthop 2013 33(5):511-18. [Google Scholar]
[4]. Stanitski CL, Paletta GA, Articular cartilage injury with acute patellar dislocation in adolescents. Arthroscopic and radiographic correlationAm J Sports Med 1998 26:52-55. [Google Scholar]
[5]. Rae PS, Khasawneh ZM, Herbert screw fixation of osteochondral fractures of the patellaInjury 1988 19:116-19. [Google Scholar]
[6]. Pritsch M, Velkes S, Levy O, Greental A, Suture fixation of osteochondral fractures of the patellaJ Bone Joint Surg Br 1995 77:154-55. [Google Scholar]
[7]. Matsusue Y, Nakamura T, Suzuki S, Iwasaki R, Biodegradable pin fixation of osteochondral fragments of the kneeClin Orthop Relat Res 1996 322:166-73. [Google Scholar]
[8]. Toupin JM, Lechevallier J, Osteochondral fractures of the external femoral condyle after traumatic patellar dislocation during physical exercise in childrenRev Chir Orthop Reparatrice Appar Mot 1997 83:540-50. [Google Scholar]