Unusual Cause for Abdominal Pain in Cirrhosis : Thrombosed Intrahepatic Portal Vein Aneurysms
Senthil Kumar Aiyappan1, Upasana Ranga2, Saveetha Veeraiyan3
1Associate Professor, Department of Radiodiagnosis and Imaging, Saveetha Medical College and Hospital, Thandalam, Kancheepuram, Tamilnadu, India.
2Associate Professor, Department of Radiodiagnosis and Imaging, Saveetha Medical College and Hospital, Thandalam, Kancheepuram, Tamilnadu, India.
3Professor, Department of Radiodiagnosis and Imaging, Saveetha Medical College and Hospital, Thandalam, Kancheepuram, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Senthil Kumar Aiyappan, Associate Professor, Department of Radiodiagnosis and Imaging, Saveetha Medical College and Hospital, Thandalam, Kancheepuram, Tamilnadu- 602105, India.
Phone: 9941501382,
E-mail: senthilkumarpgi@yahoo.co.in
Portal venous system aneurysm is a rare condition with very few reported cases in English literature. With the increasing availability of advanced imaging modalities like Doppler ultrasound, computed tomography and magnetic resonance imaging, portal venous system aneurysms are being increasingly reported. Here, we report a rare case of multiple intrahepatic portal venous system aneurysms complicated by thrombosis in a young patient with chronic liver disease and portal hypertension.
Cirrhosis, CT, MRI, Portal vein aneurysms, Thrombosed
Case Report
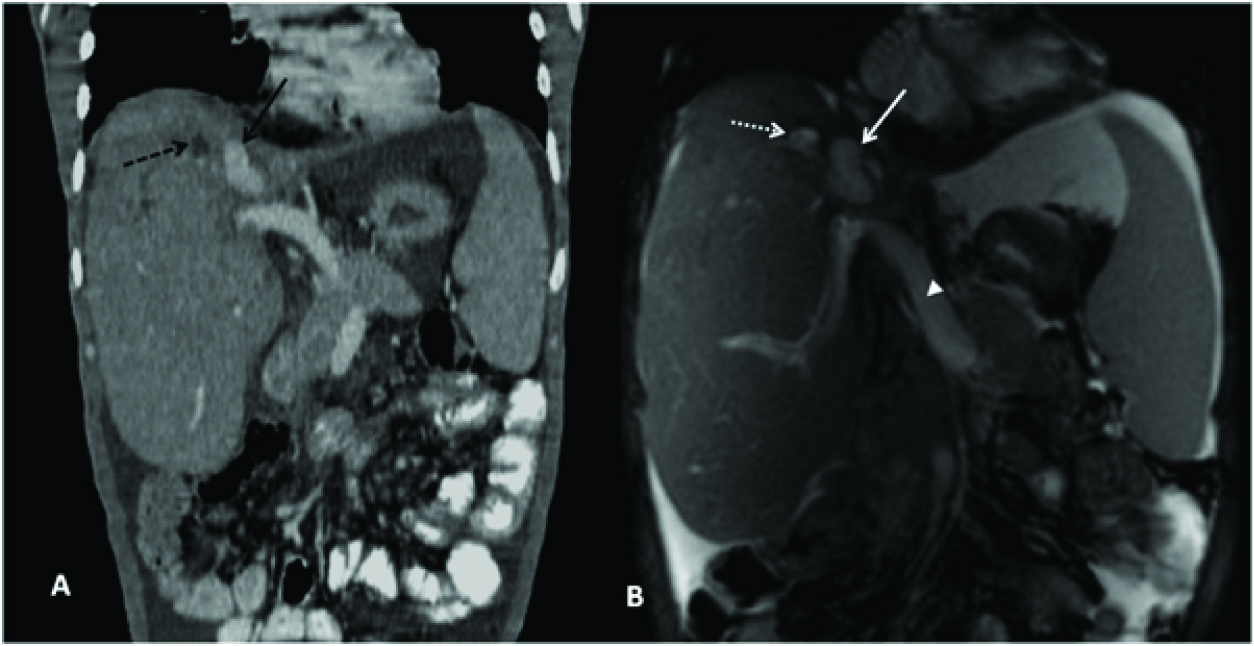
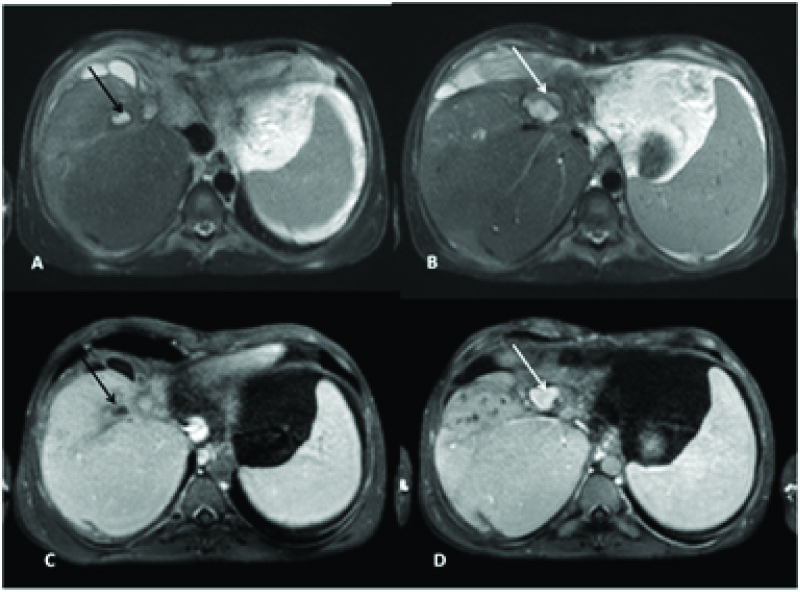
30-year-old male patient presented with complaints of upper abdominal pain, nausea, pruritus and fever for the past three days. He was diagnosed as having chronic alcoholic liver disease with portal hypertension one year back and was on regular treatment. Physical examination revealed splenomegaly and stigmata of chronic liver disease. Complete blood count showed mild neutrophilic leukocytosis with mildly reduced platelet count of 85000/mm3. Liver function tests showed elevated direct bilirubin of 7mg/dl with mildly elevated liver enzymes. Serum hepatitis markers were negative. Ultrasound abdomen with doppler imaging showed presence of 26mm sized aneurysm involving right branch of portal vein showing partial color flow and mild echogenic content likely thrombus. Contrast enhanced computed tomography (CT) of the abdomen confirmed the findings of saccular intrahepatic portal vein aneurysm involving anterior segment of right portal vein measuring 26mm with partial thrombus and another small hypodense lesion measuring 11mm along the anterior segment of right branch of portal vein close to the aneurysm not filling with contrast likely suggesting completely thrombosed aneurysm [Table/Fig-1A]. Magnetic resonance imaging (MRI) of the upper abdomen with contrast confirmed the CT findings of two saccular intrahepatic portal vein aneurysms [Table/Fig-1B] involving anterior segment of right portal vein with one completely thrombosed [Table/Fig-2A,C] and another partially thrombosed [Table/Fig-2B,D] and MRI also demonstrated completely thrombosed anterior segmental branches of right portal vein distal to thrombosed aneurysm. Since the onset of abdominal pain was recent and previous ultrasound done one month back did not show presence of thrombus, possibility of acute to subacute thrombus was considered. Hence anticoagulation therapy was started and continued for 6 months. Patient had symptomatic improvement and there was no progression of thrombus, although only partial recanalisation was obtained in follow-up doppler scan done at five month later.
Discussion
Portal venous system aneurysms are defined as a focal saccular or fusiform dilatation of the portal venous system which includes portal vein, superior mesenteric vein and splenic vein in the region of spleno-portal junction [1-3]. They represent 3% of all venous aneurysms and are the most common of the visceral venous aneurysms [1]. Portal venous system aneurysms are relatively rare with just less than 200 cases reported in the English literature [3]. SectionThe diagnosis of portal venous system aneurysm is made when the maximum portal vein diameter exceeds 2cm for extrahepatic portal venous system aneurysms [1]. For intrahepatic portal venous system aneurysms, diameter more than 9mm and any vein significantly larger than the remaining segments of the same vein is considered aneurysm [1]. Portal venous system aneurysms are mainly extrahepatic and commonly involve main portal and splenic vein [3]. Our case is a rare multiple intrahepatic portal venous system aneurysms. Age and sex of the patient does not play a role in the development of portal venous system aneurysms [1]. The aetiology of portal venous system aneurysms can be congenital or acquired [1,3]. Acquired causes include chronic liver disease, portal hypertension as in our case, and pancreatitis, trauma, effects of surgery being other acquired causes [1].
The clinical effects of portal venous system aneurysm depend on the size and its complications. The most common manifestation is abdominal pain followed by incidental detection on imaging studies [3]. Portal vein thrombosis, portal hypertension, compression of adjacent structures and aneurysmal rupture are the reported complications [4]. Gallego et al reported a 30% prevalence of portal vein thrombosis in portal venous system aneurysm [1,5]. Patient can present with acute abdominal pain, nausea, vomiting and fever in case of portal vein thrombosis as in our case [1]. However, most of the portal venous system aneurysms are stable and have low risk of complications with 88% of patients showing no progression of aneurysm size or complications on follow up imaging [1,3].
The diagnosis of portal venous system aneurysms can be easily made by doppler sonography, contrast enhanced computed tomography and magnetic resonance imaging (MRI) depending on the availability [1]. Doppler sonography is the preferred imaging modality for diagnosis and follows up [1,3]. CT scan and MRI are reserved for patients with indeterminate doppler imaging findings nd complications [3]. Most of the uncomplicated portal venous system aneurysms does not require treatment and follow up is sufficient [1,3]. Anti coagulation therapy is recommended in the setting of acute portal vein thrombosis in portal vein aneurysms with 80% of patients showing partial or complete recanalization [6].
Percutaneous thrombolysis or thrombectomy is indicated in patients failing anticoagulation therapy or with extensive thrombus burden or in patients with symptoms related to aneurysm mass effect [6]. Porto-systemic bypass surgery or aneurysmorrhaphy is performed if the recanalisation procedures fail or if the aneurysm size enlarges [6]. The time limit for anticoagulation therapy in patients with liver disease is not exactly established, although various studies recommending from one month upto lifelong maintenance [7]. The recanalisation has been shown to occur only within six months from the start of anti coagulants in cases of portal vein thrombosis without underlying liver disease [7]. Although, Prophylactic anticoagulation in cirrhotic patients may have a role in decreasing the incidence of portal vein thrombosis and improved survival, further studies are required [8]. Portal venous system aneurysm is usually diagnosed incidentally during routine imaging studies and they can be symptomatic depending on its size and related complications. Advances in imaging techniques have increased the number of portal venous system aneurysms discovered during routine imaging, however the underlying pathophysiology and management still remains a challenge.
Coronal contrast CT images done in venous phase shows saccular contrast filled outpouching along anterior segmental branch of right portal vein suggestive of aneurysm (black arrow) with another hypodense lesion close to it which is not filling with contrast (dotted black arrow) suggestive of completely thrombosed aneurysm. B Coronal true FISP MR images showing two well defined hyperintense areas (white and dotted white arrows) in right lobe of liver along the line of anterior segmental branch of right portal vein suggestive of intrahepatic portal vein aneurysms. Dilated main portal vein also noted (arrow head)
A and B) Axial T2 weighted MR images, and C and D) axial Contrast enhanced MR images showing two T2 hyperintense lesions along anterior segmental branch of right portal vein with one of them in figure B showing T2 hypointensity peripherally (white arrow) suggestive of partial thrombus. The T2 hyperintense lesion in figure B is showing partial contrast filling (white arrow in figure D) suggestive of partially thrombosed aneurysm, however the other lesion (black arrow in figure A) is not showing contrast filling (black arrow in figure C) suggestive of completely hrombosed aneurysm
[1]. Z Koc, L Oguzkurt, S Ulusan, Portal venous system aneurysms: imaging, clinical findings, and a possible new etiologic factor.AJR Am J Roentgenol 2007 189(5):1023-30. [Google Scholar]
[2]. W Debernardi-Venon, D Stradella, G Ferruzzi, F Marchisio, C Elia, M Rizzetto, Extrahepatic aneurysm of the portal venous system and portal hypertension.World J Hepatol. 2013 5(3):149-51. [Google Scholar]
[3]. R Ma, A Balakrishnan, TC See, SS Liau, R Praseedom, A Jah, Extra-hepatic portal vein aneurysm: A case report, overview of the literature and suggested management algorithm.Int J Surg Case Rep. 2012 3(11):555-58. [Google Scholar]
[4]. C Lall, S Verma, R Gulati, P Bhargava, Portal vein aneurysm presenting with obstructive jaundice.J Clin Imaging Sci. 2012 2:54 [Google Scholar]
[5]. C Gallego, M Velasco, P Marcuello, D Tejedor, L De Campo, A Friera, Congenital and acquired anomalies of the portal venous system.Radiographics 2002 22(1):141-59. [Google Scholar]
[6]. RB Schwope, DJ Margolis, SS Raman, BM Kadell, Portal vein aneurysms: a case series with literature review. J Radiol Case Rep. 2010 4(6):28-38. [Google Scholar]
[7]. SE Congly, SS Lee, Portal vein thrombosis: should anticoagulation be used? Curr Gastroenterol Rep 2013 15(2):306 [Google Scholar]
[8]. KI Rodriguez-Castro, P Simioni, P Burra, M Senzolo, Anticoagulation for the treatment of thrombotic complications in patients with cirrhosis. Liver Int. 2012 32(10):1465-76. [Google Scholar]