Three Cases of Subungual Glomus Tumours of the Fingers – A Case Series
Surya Rao R V M1, D Alagar Raja2
1 Assistant Professor, Department of Plastic Surgery, Saveetha Medical College Hospital, Thandalam, Kanchipuram, India.
2 Assistant Professor, Department of Plastic Surgery, Saveetha Medical College Hospital, Thandalam, Kanchipuram, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surya Rao R V M, Assistant Professor, Department of Plastic Surgery, Saveetha Medical College Hospital, Thandalam, Kanchipuram Dist - 602105, India. Phone : 9444152963, E-mail : surya_3@hotmail.com
Subungual glomus tumours are rare tumours (2% of all hand tumours) presenting with excruciating pin point pain under the nail which is often misdiagnosed. Diagnosis is often always clinical. Here, we report the case of three patients who had subungual glomus tumour not diagnosed earlier for many years.
Clinical diagnosis, Painful fingertip, Rare, Surgical excision
Case Report
Case 1
A 37-year-old patient presented to us with a painful left index finger tip for the past 12 years. The pain was excruciating with waxing and waning episodes, pain increases in cold weather and not relieved by any analgesics. The patient had consulted many doctors for the above complaints. On examination, there was severe point tenderness at eponychial region of the left index finger. Love’s Pin test and Hildreth’s test were positive. There was no nail discolouration and no nail deformity.
A clinical diagnosis of a subungual glomus tumour of left index finger was made and proceeded for exploration.
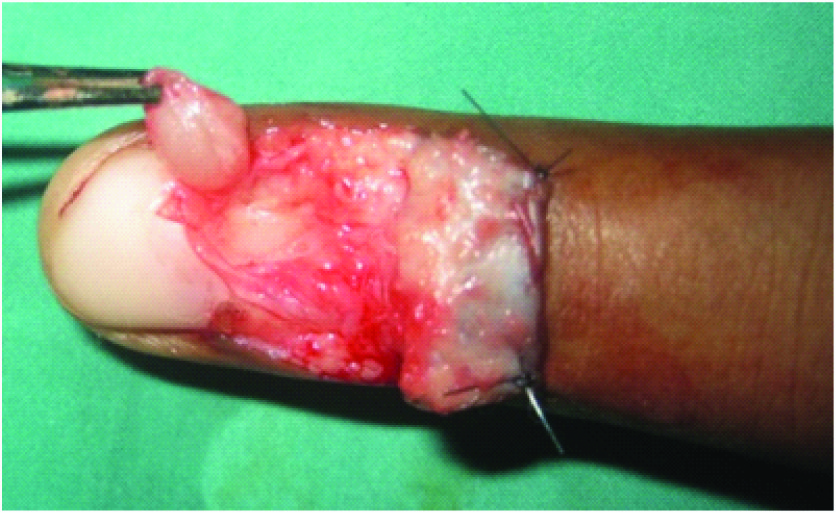
Under local anaesthesia (2% Plain Xylocaine), a latero-ungual approach was used. An eponychial flap was raised, nail bed incised and the tumour was shelled out [Table/Fig-1]. Haemostasis was secured and the eponychial flap was sutured back with 5-0 ethilon.
Glomus tumour being excised
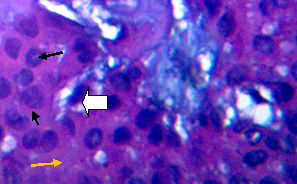
Histopathology examination showed a circumscribed neoplasm composed of sheets of round glomus cells collared around the blood vessels which were lined by normal endothelium [Table/Fig-2]. The intervening stroma showed myxoid change.
Histopathology examination showed a circumscribed neoplasm composed of sheets of round glomus (black arrows) cells collared around the blood vessels (bold white arrow) which were lined by normal endothelium. The intervening stroma (yellow arrow) showed myxoid change (Haematoxylin- Eosin stain, high power magnification)
Case 2
A 47-year-old male presented to us with pain and deformity of right little finger for the past 4 years. He was wrongly diagnosed as a subungual haematoma elsewhere where an incision and drainage was done, but swelling recurred and pain was persistent.
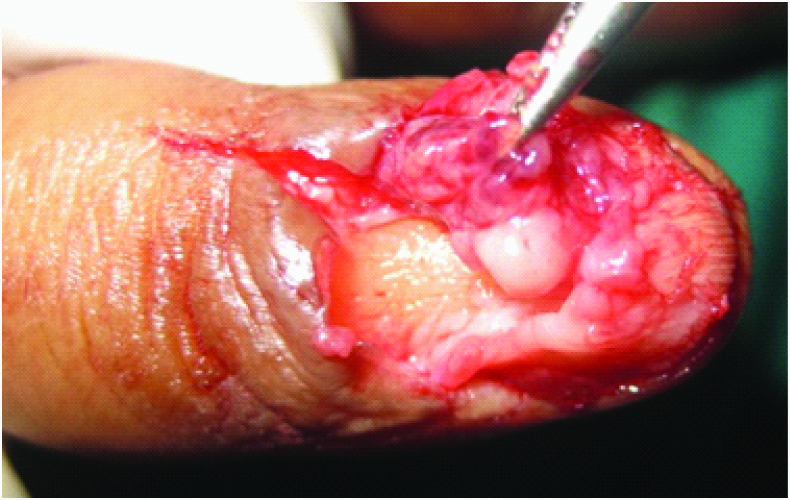
On examination, there was deformity and bluish discolouration under the nail with the Love’s Pin test and the Hildreth’s test being positive. A clinical diagnosis of a subungual glomus tumour of the right little finger was made and preceded for exploration [Table/Fig-3a]. Through a transungular approach [Table/Fig-3b], the deformed nail plate was excised and the nail bed was incised. A small pin sized swelling with surrounding fibroareolar tissue was excised and sent for histopathology. The nail bed was repaired with 5-0 monocryl and a Vaseline gauze and finger bandage was applied. Histopathology examination confirmed glomus tumour.
Subungual glomus tumour of right liitle finger

Tumour removed by transungular approach
Case 3
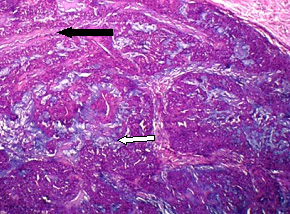
A 22-year-old girl presented to us with painful right ring finger tip for 2 years [Table/Fig-4a]. Love’s pin test was positive with typical history of increased pain during winter months. Excision was done and histopathology revealed a subungual glomus tumour [Table/Fig-4b].
Glomus tumour right ring finger tip

Low power magnification of glomus tumour (Haematoxilin - Eosin stain) showing sheets of glomus cells. Blood vessels (white arrow), stroma (black arrow)
Discussion
Glomus tumours that were described first by Masson in 1942, can occur anywhere in the skin or soft tissue, and the most common site is the finger. The tumour usually presents as a painful, firm, purplish solitary nodule of the extremities, most commonly in the nail bed [1]. It is a rare tumour, 2% of all hand tumours.
Normal glomus bodies are found in the dermal retinacular layer of the skin and thought to aid in the thermoregulation of skin circulation and to be highly concentrated in the finger tips, particularly beneath the nail bed [2]. Glomus body (MASSON) is a neuromyoarterial glomus, which is an arteriovenous anastomosis functioning without an intermediary capillary bed & surrounded by a capsule of connective tissue (structures called Sucquet – Hoyer canals).
They are solitary tumours commonly found in the distal phalanx in a paraungual or subungual location. They present with a classic triad of paroxysmal pain, pinpoint tenderness, and cold hypersensitivity. Changes in temperature, palpation, and touching may cause pain and hypersensitivity [3].
Specific Tests
Diagnostic clinical tests included Love’ sign, Hildreth’ sign and transillumination. Love’ sign i.e. pressure applied over the lesion with the tip of a pencil eliciting excruciating pain [4]. Hildreth’ sign i.e. the point pain diminished after slowly insufflating a brachial cuff [5].
Investigations
Transillumination [6], Magnetic resonance imaging (MRI) [7] and US are useful tools to confirm the tumour location. MRI shows a low signal on T1 and a high signal on T2. As long as there is no bony erosion, plain X-rays cannot be helpful except in long standing cases where bony erosions are evident [8].
Treatment
In central (subungual) lesions, a direct transungular approach was performed by removing the nail plate and incising the nail bed longitudinally to explore the underneath tumour. In peripheral lesions, a lateroungual approach was preferred, where a lateral incision was done close to and parallel to the nail margin accompanied with partial nail removal if necessary.
[1]. Moor EV, Goldberg I, Westreich M, Multiple glomus tumor. A case report and review of the literatureAnn Plast Surg 1999 43:436-38. [Google Scholar]
[2]. Cotran RS, Kumar V, Collins T, Stanley L, Robbins Pathologic Basic of Disease 1999 6th edPhiladelphiaWB Saunders Company:533-34. [Google Scholar]
[3]. Ogino T, Ohnishi N, Ultrasonography of a subungual glomus tumorsJ Hand Surg (Br) 1993 18:746-47. [Google Scholar]
[4]. Love JG, Glomus tumors: Diagnosis and treatmentMayo Clin Proc 1944 19:113-16. [Google Scholar]
[5]. Hildreth DH, The ischemia of glomus tumors. A new diagnostic testRev Surg 1970 27:147-48. [Google Scholar]
[6]. Ekin A, Ozkan M, Kabaklioglu T, Subungual glomus tumors: A different approach to diagnosis and treatmentJ Hand Surg (Br) 1997 22:228-29. [Google Scholar]
[7]. Drape JL, Idy-Peretti I, Goettmann S, Wolfram-Gabel R, Dion E, Grossin M, Subungual glomus tumors: Evaluation with MR imagingRadiology 1995 195:507-15. [Google Scholar]
[8]. Johnson DL, Kuschner SH, Lane CS, Intraosseous glomus tumor of the phalanx: A case reportJ Hand Surg (Am) 1993 18:1026-28. [Google Scholar]