The world Health Organization (WHO) has laid the definition of infertility as the inability of a couple to conceive within two years of exposure to the risk of pregnancy. At present, about 15% of couples are infertile because of several reasons, out of which the male factor is responsible for approximately 50% of the cases [1]. It is estimated that globally, 60–80 million couples suffer from infertility every year, of which probably 15–20 million are in India alone [2].
Different genetic factors, including chromosomal abnormalities, single gene defects and phenotypes with multifactorial inheritance, have been considered in about 30-60% of infertile males [3]. Genetic defects may cause the dysfunction of the hypotha lamao-gonadal axis or interfere with the development of the male gonads and urogenital tract. They may cause arrest of germ cell production and maturation or lead to the production of nonfunctional spermatozoa [4].
Chromosomal anomalies have been postulated to contribute as one of the principal genetic factors in male infertility. It has been estimated that the prevalence of chromosomal abnormalities in infertile males have been found within the range of 2.4-16.4% [5] compared to the frequency in general male population (0.3- 0.4%) [6]. In men with azoospermia the incidence of chromosomal abnormalities is especially high, varying from 13.1% to 23.6%; in males with oligospermia, the incidence is 2.1-6.6% and in men with severe oligospermia it is 10.6% [7,8]. The incidence of autosomal chromosome abnormalities in infertile men is 1.1-7.2% [9] and sex chromosome abnormalities are in a range of 0.4-12.3% [7]. Thus, the aim of this study was to determine the occurrence of various chromosomal aberrations of infertile men having primary infertility in the Indian males prior to assisted reproductive techniques (ART)treatment. India is an ethic country where different communities of people are living. The number of studies had been conducted on infertile men causing infertility due to chromosomal defects, so here in this study we also tried to consolidate the data published from different parts of India with the aim to estimate the overall frequency of chromosomal abnormalities in infertile men.
Materials and Methods
The present study was carried out at Preventine Life Care, Navi- Mumbai and Genetic division, Department of Anatomy, Grant Medical College & Sir J.J. Group of Hospitals, Mumbai, India. All samples for this study were received from government, private hospitals, infertility clinics and informed consent was taken up by referring doctors. The 78 infertile men with primary infertility, out of which 26 men were azoospermic, 19 men were oligospermic, 4 men were asthenospermic and 29 men were oligoasthenoteratospermic (OAT) were studied. The 30 fertile males with at least one child were taken as controls. For Indian data analysis, total 1736 infertile subjects were analyzed based on their seminal parameters.
The 3ml heparinised peripheral blood samples of the patient were cultured for 72h in RPMI-1640 medium supplemented with fetal bovine serum and phytohemagglutinin. Cytogenetic analysis was performed in patients by using the GTG banding technique. At least 20 metaphases were analysed, images was captured using Karyo Imaging Metasystem software (Zeiss), and the karyotype was designated according to ISCN (2009) nomenclature.
Results
In present study, chromosomal analysis of 78 infertile males having primary infertility with abnormal sperm parameters showed major chromosome abnormalities in 10.2% (8/78) cases, with an occurrence of 6.4% (5/78) and 3.8% (3/78) in autosomal chromosome abnormalities and sex chromosome abnormalities [Table/Fig-1]. Among these, the incidence of major chromosome abnormalities in oligospermic males were 21% (4/19) and azoospermic males were 15.4 % (4/26); no chromosomal defect were observed in the other categories [Table/Fig-2].
Chromosomal alterations in infertile men and in the control group
| S. No. | Classification of chromosome | Infertile males (n=78) | Control Group (n=30) |
|---|
| I | Normal Chromosomal Karyotype | 57 (73%) | 25 (83.4%) |
| II | Chromosomal Alterations | 21 (27%) | 5 (16.6%) |
| A | Major Chromosomal Abnormalities | 8 (10.2%) | - |
| Autosomal abnormalities | 5 (6.4%) | - |
| Sex chromosome abnormalities | 3 (3.8%) | - |
| B | Polymorphic Chromosomal variants | 13 (16.7%) | 5 (16.6%) |
Chromosomal alterations in infertile men having primary infertility with abnormal sperm parameters
| Sr. No | Classification of chromosome | Azoospermia (n=26) | Oligospermia (n=19) | Asthenospermia (n=4) | Oligoasthenoterato spermia (n=29) |
|---|
| I | Normal Chromosomal Karyotype | 21 (80.8%) | 8 (42.1%) | 3 (75%) | 25 (86.2%) |
| II | Chromosomal Alterations | 5 (19.2%) | 11 (57.9%) | 1 (25%) | 4 (13.8%) |
| A. | Major Chromosomal Abnormalities | 4 (15.4%) | 4 (21%) | – | – |
| Autosomal abnormalities | 1 (3.9%) | 4 (21%) | – | – |
| Sex chromosome abnormalities | 3 (11.5%) | – | – | – |
| B. | Chromosomal variants | 1 (11.5%) | 7 (36.8%) | 1 (25%) | 4 (13.8%) |
| III | Karyotype |
| Major Chromosomal Abnormalities | 46,XY,t(13;14)(q14;p11) | 45,XY,t(13;14)(q10;q10) | – | – |
| 47,XXY | 45,XY,t(15;22) |
| 47,XYY | 45,XY,t(13;14)(q10;q10) |
| mos 45,X[45]/46,XY[5] | 46,XY,t(8;12)(p23;q15) |
| Polymorphic Chromosomal variants | 46,X,inv(Y) | 46,XY,22pstk+ | 46 XY,15pstk+ | 46,X,inv(Y) |
| 46,XY,inv(9)x2(p11;q13) | 46,X,inv(Y) |
| 46,XY,inv(9)(p11;q13) | 46,X,inv(Y) |
| 46,XY,22ps+ | 46,XY,inv(9)(p11;q13) |
| 46,X,Yqh+ | |
| 46,X,Yqh+ |
| 46,X,Yqh- |
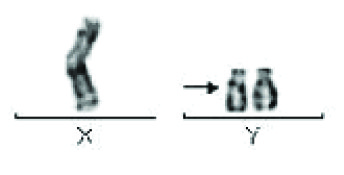
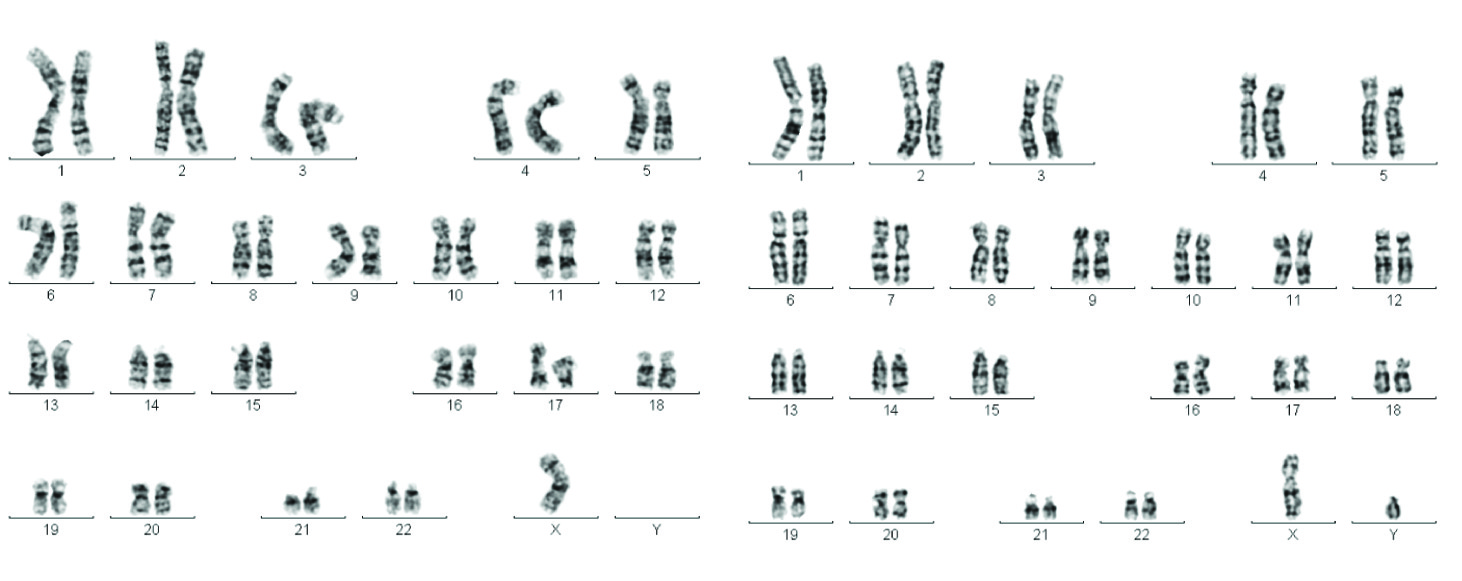
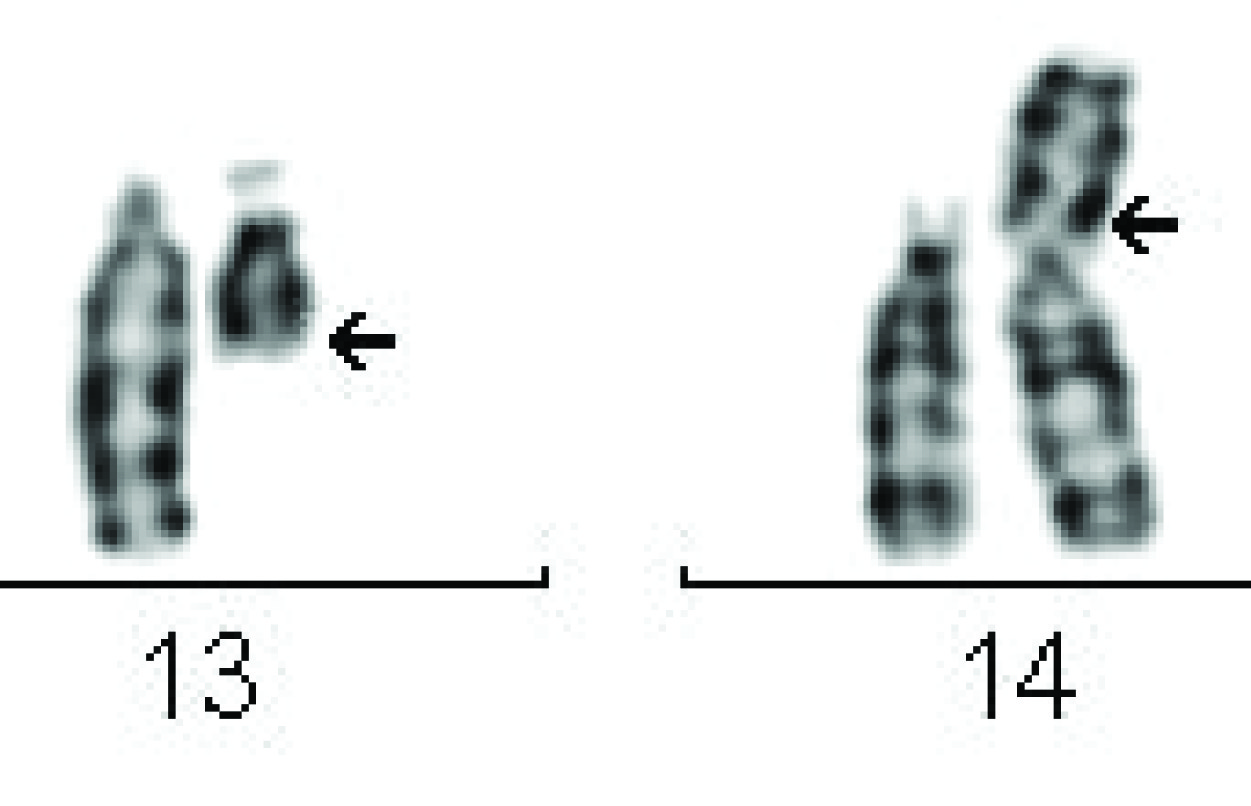
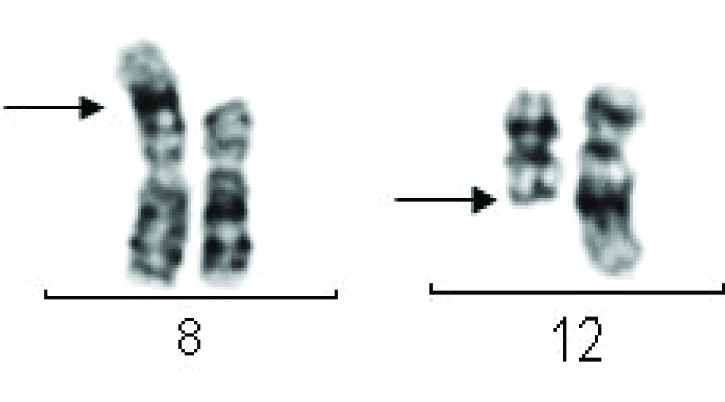
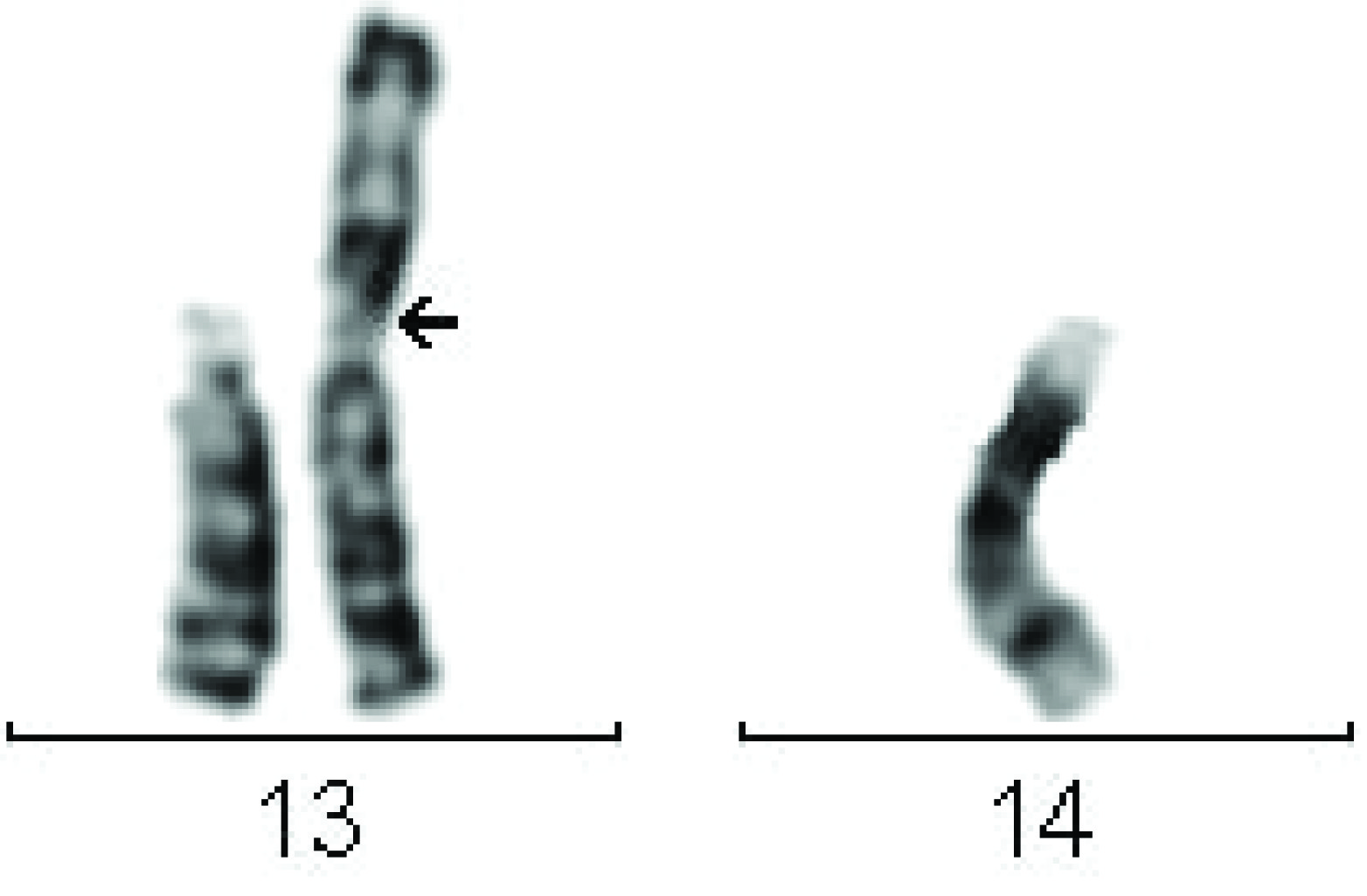
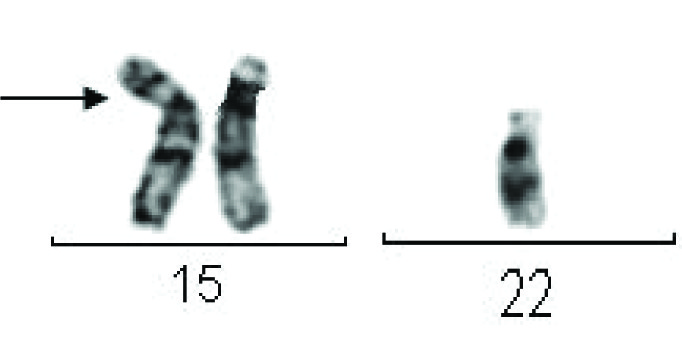
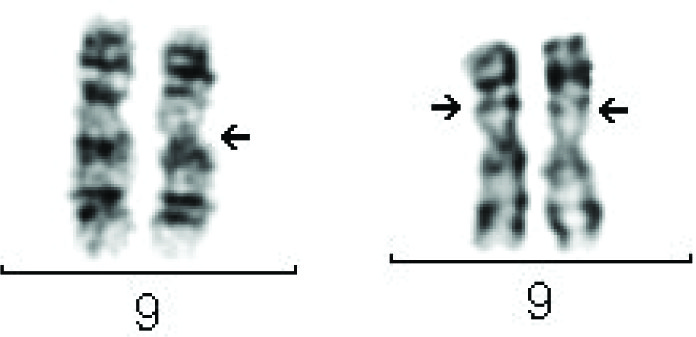
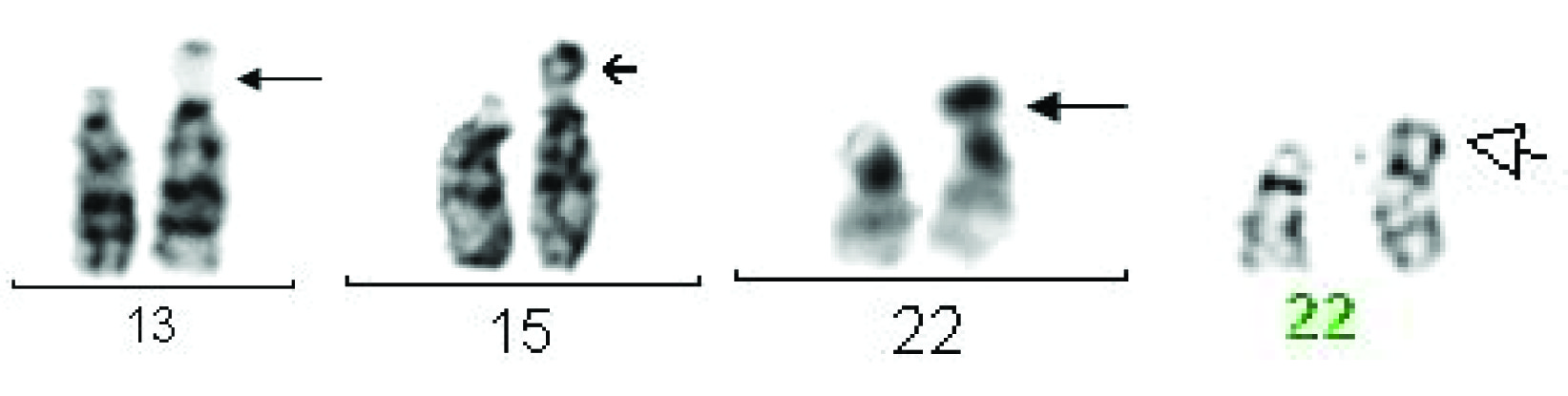
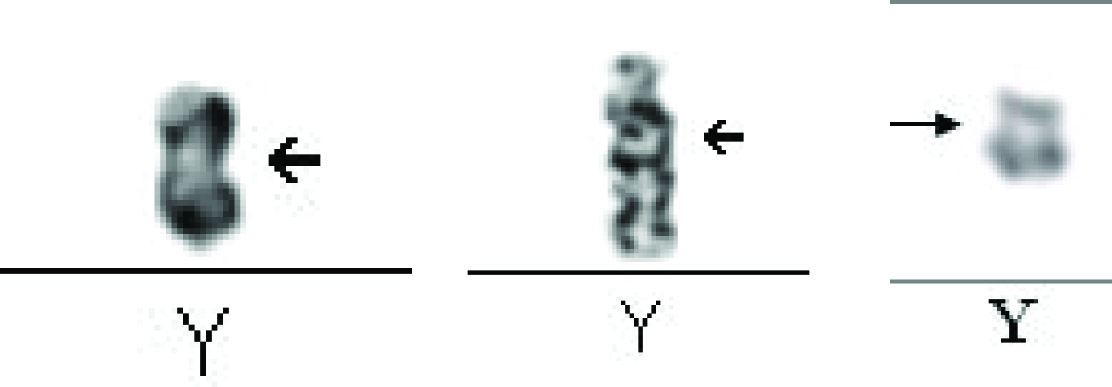
Sex chromosome aberrations were manifested as Klinefelter’s syndrome (47,XXY) [n=1] [Table/Fig-3], 47,XYY Karyotype [n=1] [Table/Fig-4], and Mosaic 45,X/46,XY Karyotype [n=1][Table/ Fig-5] observed in azoospermic men. Among five cases of autosomal abnormalities, two cases of balanced translocations i.e. 46,XY,t(13;14)(q14;p11) karyotype [Table/Fig-6] observed in azoospermic men and 46,XY,t(8;12)(p23;q15) karyotype [Table/ Fig-7] detected in oligospermic men and all three cases of Robertsonian translocations i.e. two with 45,XY, t (13;14) [Table/ Fig-8] and one with 45,XY,t(15;22) karyotype [Table/Fig-9] observed in oligospermic men. Chromosomal polymorphic variants were identified 16.7% (13/78), which included inv(9), 15pstk+, 22pstk+, 22ps+, Yqh+, Yqh- and inv(Y) [Table/Fig-10a,b,c].
Karyotype of Klinefelter’s syndrome patient showing 47,XXY
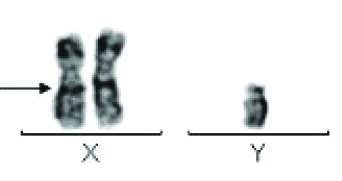
Mosaic karyotype showing mos 45,X[45]/46,XY [5]
Karyotype showing translocation between chromosomes 13 and 14- 46,XY,t(13;14)(q14;p11)
Karyotype showing translocation between chromosomes 8 and 12-46,XY,t(8;12)(p23;q15)
Karyotype showing Robertsonian translocation between chromosomes 13 and 14 - 45,XY,t(13;14) (q10;q10)
Karyotype showing Robertsonian translocation between chromosomes 15 and 22- 45,XY,t (15;22)
Inversion in chromosome 9, inv 9
Structural abnormalities of Y chromosome
In cumulative data published from India of 1736 infertile men, the frequency of chromosomal abnormalities was found to be 8.4% . Since the patients included in our study are from the western part of India and as there are geographic differences in the prevalence of chromosomal abnormality in different parts of the country, we pooled the data from the papers published from India and estimated the overall frequency. To this end information on 1814 infertile individuals were available, 153 infertile men had chromosomal defects resulting in prevalence of 8.4%., with an incidence of 10.8% (76/706) in azoospermia, 7.3% (21/288) in oligospermia and 7.3% (51/697) in OAT respectively from India [Table/Fig-11,12].
Frequency of chromosomal polymorphic variants observed in infertile men and control men in the present study
| Sr. No. | No. of individuals | Chromosomal Polymorphic Variants | Percentage of variants |
|---|
| inv(9) | 9qh+ | Yqh+ | Yqh- | inv(Y) | D/G group |
|---|
| 1 | 78 | 13 (16.7%) | 3 (3.8%) | - | 2 (2.5%) | 1 (1.3%) | 4 (5.12%) | 3 (3%) |
| 2 | 30 | 5 (16.6%) | 1 (3.3%) | 3 (10%) | - | - | - | 1 (3.3%) |
Frequency of chromosomal abnormalities in infertile men with abnormal sperm parameters reported by different authors from India
| Author | No. of patients | Percentage | Azoospermia | Oligospermia | Asthenospermia | OAT |
|---|
| Rao Kl et al.,[7] | 251 | 28 (11.5%) | 9/104 (3.6%) | 5/90 (2.0%) | – | 14/57 (5.6%) |
| Rao KL et al.,[10] | 744 | 59 (7.9%) | 30/272 (11.0%) | – | – | 29/ 472 (6.1%) |
| Nagvenkar P et al.,[8] | 88 | 9 (10.2%) | 6/42 (14.3%) | 3/46 (6.5%) | – | – |
| Gupta A, [11] | 91 | 10 (10.9%) | 7/45 (15.7%) | 346 (6.6%) | – | – |
| Gagare D et al.,[12] | 112 | 13 (11.6%) | 8/ 44 (18.2%) | 5/68 (7.4%) | – | – |
| Sreenivasa G et al.,[13] | 200 | 15 (7.5%) | 8/ 48 (16.6%) | 1/19 (5.3%) | – | 1/ 17 (5.8%) |
| Vijayalakshmi J et al., [14] | 150 | 5 (3.3%) | 4/ 125 (3.2%) | – | – | 1/44 (2.2%) |
| Muthiah SS et al., [15] | 100 | 6 (6%) | – | – | – | 6/100 (6%) |
| Total | 1736 | 145 (8.4%) | 72/680 (10.6%) | 17/269 (6.3%) | | 51/668 (7.6%) |
Discussion
Chromosomal abnormalities have emerged as one of the major genetic factors contributing to male infertility. In present study, the frequency of major chromosomal anomalies was 10.2% in infertile males with primary infertility; with an incidence of autosomal chromosome abnormalities was 6.4% and sex chromosome abnormalities was 3.8% [Table/Fig-1]. Various cytogenetic studies have reported variable frequency (5-15%) of major chromosomal anomalies in male infertility.
Sex chromosome abnormalities are the most frequent chromo- some related cause of infertility. In our study, we found one azoospermic male patient with Klinefelter’s syndrome (47,XXY karyotype). Klinefelter’s syndrome males can be identified only when they undergo fertility assessments. Van Assche et al., reported 11% azoospermic individuals with Klinefelter syndrome Sreenivasa et al., [13]. Infertility in these patients is because of the direct harmful effect of an extra X chromosome causing lethal gene dosage effect in the cells in the testis resulting in azoospermia [6]. A 47,XYY karyotype was found in one azoospermic male. Men with a 47,XYY karyotype are fertile and there is no evidence of transmission of the extra Y chromosome to their progeny because the supernumerary Y- chromosome is eliminated during meiosis [16]. A Mosaic 45,X/46,XY karyotype was found in one azoospermic male. The formation of mosaic 45,X/46,XY leads to spermatogenic defects. 45,X/46,XY males carry an increased risk for gonadal tumors and must be followed closely [17]. Gonosomal mosaicism may be a probable cause for the failure of assisted reproduction [8].
Autosomal abnormalities interfere with normal chromosome pairing and segregation at meiosis I, thus formation of unbalanced gametes and subsequent unbalanced abnormal offspring [8]. Two cases of autosomal balanced translocation were detected; one with 46,XY,t (13;14)(q14;p11) karyotype in azoospermic male and another 46,XY,t (8;12)(p23;q15) karyotype in oligospermic male. The structural chromosome autosomal abnormalities in men often lead to low sperm concentrations, abnormal sperms with male infertility and increased miscarriages [18]. Three cases of oligospermic males with Robertsonian translocation, two with 45,XY,t (13;14) karyotype and one with 45,XY,t (15;22) karyotype were detected in our study. The association of acrocentric chromosomes with the X-Y sex chromosome results in severe spermatogenic defects and significantly increases risk of unbalanced spermatozoa and miscarriages [6].
The overall occurrence of chromosomal abnormalities in infertile males depends on a number of factors; the most important of these is the selection of patients based on the sperm count. In present study the prevalence of major chromosomal anomalies, in males with azoospermia was 15.4%, the findings which was similar with 15.6% [6] and 17.4% [9]; and in males with oligospermia containing only autosomal chromosome abnormalities was 21%, which was higher than other studies 6.9% [9] and 12.1% [6].
Previous studies reported from India have revealed a wide geographic variation (3.3%-11.6%) in the frequency of chromosomal abnormalities in infertile men, with the average being 8.4% (145/1736). Also, many international studies have documented the chromosomal abnormalities which range from 4% to 15.5% for infertile men, with the average being 8.2% (268/3295). By comparing present study with an Indian data, a significantly higher frequency (10.2%) of chromosomal abnormalities was observed, with an incidence of azoospermia was 15.4% and oligospermia was 21%; whereas in Indian data shows 8.4% of chromosomal abnormalities in infertile men, with an occurrence of azoospermia was 10.6% and oligospermia was 6.3%. This difference in present study was observed may be due to ethnicity, the selection criteria and sample size. Thus, to nullify the multiple confusing variables including the ethnicity and determine the actual frequency of chromosomal abnormalities in infertile men from Indian population, we combined the data from our present study and Indian published data with uniform patient selection criteria. The results revealed an overall frequency of chromosomal abnormalities to be 8.4% (153/1814) in the infertile men, with an occurrence of azoospermia10.8% (76/706), oligospermia 7.3% (21/288) and OAT 7.3% (51/697) respectively from India. These observations imply that the chromosomal abnormalities are an important factor in male infertility in the Indian population, somewhat similar overall frequency observed in the western countries.
Polymorphic chromosomal variants: In the present study, the overall occurrence of chromosomal polymorphic variants in infertile males with primary infertility was 16.7% which is higher than 7.9% (Sahin FI et al.,) and less than 28.82% (Madon PF et al.,); 37.5% [8]; 58.68% [19].
Y Chromosome Variations: In present study, the occurrence of long Y (Yqh+) in infertile males was 2.5% and short Y (Yqh-) was 1.3%. Sahin FI et al., hypothesis states that polymorphic heterochromatic regions could interfere with male meiosis which leads to oligospermia or azoospermia eventually causing infertility. Deletion of the entire heterochromatin and part of euchromatin of Y chromosome was detected in infertile men [1].
In present study, 5.12% cases of inversion of Y chromosome were observed in infertile men. Individual with inversion carries its own risk for unbalanced offspring [8].
Chromosome 9 Variations: In present study the incidence of pericentric inversion of chromosome 9, in infertile males was 3.8% comparable with control group 3.3%. Lissitsina J, suggested that inv (9) may often cause infertility in men due to spermatogenic disturbances, which have arisen by the loops formed in meiosis.
Variants of short-arms of acrocentric chromosomes of d/g groups: In present study, the incidence of presence of satellites and stalk in D/G group of acrocentric chromosome in infertile males was 3% and in the control group 3.3%, which correlates with 2.2% [6]; 3.3% [20].
Chromosomal polymorphic variation was considered normal for a long period of time. In recent years, more and more studies have shown an increased incidence of chromosomal polymorphism in infertile couples. There seems to be some relationship between chromosomal polymorphism and decreased fertility. However, some past studies indicate that chromosome polymorphisms may cause infertility [21–23]. Increased rates of chromosomal polymorphic variants have been shown to be associated with poor spermatogenesis [24]. Variants have also been shown to occur in one or both partners of couples with idiopathic infertility [25]. Polymorphic chromosomal variants may also increase the risk of production of unbalanced gametes resulting in infertility. It is proposed that a heterochromatic block may cause nondisjunction of chromosomes and subsequently meiotic arrest [6].
However, some other researchers do not agree that chromosome polymorphic variants may affect fertility. The survey results of The Cytogenetics Committee of the College of American Pathologists and The American College of Medical Genetics conclude that common cytogenetic variants are considered to be heteromorphic and of no clinical significance. The majority of clinical cytogeneticists would not even mention these variants in their reports except for pericentric inversions and rare variants. They also presume that there are currently no standards in cytogenetics for reporting heteromorphisms [26]. Chromosomal polymorphic variations appear to have no adverse effects on the outcome of IVF–embryo transfer treatment [27]. The contribution of chromosomal polymorphic variants to alter the carrier’s fertility is still a controversial topic and further studies are required to understand this [Table/Fig-13,14].
Frequency of chromosomal abnormalities in infertile men with abnormal sperm parameters from western countries
| Author | No. of patients | Percentage | Azoospermia | Oligospermia | Asthenospermia | OAT |
|---|
| Tuerlings J et al., [3] | 1792 | 72 (4%) | 4/62 (6.5%) | – | – | 30/865 (3.5%) |
| Pina-Neto J.M et al., [28] | 165 | 16 (9.6%) | 12/60 (20%) | 4/100 (4%) | – | – |
| Iman S et al., [29] | 874 | 136 (15.5%) | 106/444 (23.8%) | 11/175 (6.2%) | – | – |
| Balkan M et al., [30] | 80 | 9 (11.2%) | 7/52 (13.5%) | 2/25 (8%) | – | – |
| Akgul M et al., [9] | 179 | 18 (10.05%) | 15/86 (17.5%) | 2/73 (2.7%) | – | – |
| Kosar PA et al., [5] | 115 | 5 (4.3%) | 5/92 (5.4%) | – | – | – |
| Lissitsina J, [6] | 90 | 12 (13.4%) | 5/32 (15.6%) | 7/58 (12.1%) | – | – |
| Total | 3295 | 268 (8.2%) | 154/828 (18.6%) | 26/431 (6.03%) | | 30/865 (3.5%) |
Chromosomal alterations in infertile men with infertility from India and western countries
| Author | No. of patients | Major Chrom-osomal Abnor-mality | Total Chromosomal Alterations |
|---|
| Major Chromosome Abnormality | Polymorphic Variants |
|---|
| Autosomal Abnormality | Sex Chromosome Abnor-mality |
|---|
| From India |
| Rao KL et al., [7] | 251 | 11.20% | 7.20% | 4% | 3.20% |
| Rao KL et al., [10] | 744 | 7.90% | – | – | – |
| Nagvenkar P et al., [8] | 88 | 10.20% | 4.50% | 5.70% | 37.50% |
| Madon PF et al., [2] | 458 | – | – | – | 28.82% |
| Gupta A [11] | 91 | 10.90% | 1.10% | 9.90% | – |
| From Western Countries |
| Tuerlings J et al., [3] | 1792 | 4.00% | 2.30% | 1.70% | – |
| Meschede D et al., [31] | 432 | 2.10% | 1.60% | 0.50% | – |
| Pina-Neto J.M et al., [28] | 165 | 9.60% | 2.40% | 7.30% | – |
| Iman S et al., [29] | 874 | 15.50% | 2.30% | 13.20% | 1.00% |
| Balkan M et al., [30] | 80 | 11.20% | 2.50% | 8.80% | – |
| Sahin F I et al., [17] | 138 | – | – | – | 7.90% |
| Akgul M et al., 9] | 179 | 10.10% | 1.10% | 9.00% | 1.60% |
| Minocherhomji S et al., [14] | 380 | – | – | – | 58.68% |
| Balkan M et al., [32] | 134 | 15.70% | 3.00% | 12.60% | – |
| Alkhalaf M et al., [33] | 142 | 16.70% | 2.80% | 14.08% | 1.40% |
| Mahjoubi et al., [34] | 1052 | 14.50% | 2.80% | 11.80% | 0.80% |
| Kosar PA et al., [5] | 115 | 4.30% | – | 4.30% | – |
| Lissitsina J, [6] | 90 | 13.40% | 7.80% | 5.60% | 37.80% |
Conclusion
In summary, the data derived in the present analysis suggest a similar frequency of chromosomal abnormalities (8.4%) in infertile men from Indian population as compared to the western countries (8.2%). Our results (10.2%) of chromosomal abnormalities in infertile males indicate that the chromosomal abnormalities are one of the important causes of male infertility. In view of the genetic risks for the next generation, the importance of careful evaluation of karyotype is essential. We found balanced translocation to be the most frequent structural aberration among infertile patients. The patient with the balanced translocation has a high risk for producing offspring with partial trisomy/ monosomy of the relevant chromosomal fragments. In these cases the prenatal diagnosis for the resultant embryos is highly recommended with follow up of maternal trimester screening and fetal anomaly scan. Preimplantation genetic diagnosis (PGD) is considered a good option for such cases, especially when there is a co-existing fertility problem. Therefore conventional chromosomal analysis is an important investigative tool for male infertility, especially prior to use of any assisted reproductive techniques.