Study of Helminthiasis in Pregnancy and its Correlation with Haemoglobin Level
Shrinivas K.1, Radhika2, Sreelatha R.3, Kavitha K.4
1Assistant Professor, Department of Obstetrics and Gynaecology,Bangalore Medical College and Research Institute, Bangalore, India.
2Assistant Professor, Department of Obstetrics and Gynaecology,Bangalore Medical College and Research Institute, Bangalore, India.
3Assistant Professor, Department of Pathology,Bangalore Medical College and Research Institute, Bangalore, India.
4House Surgeon,Bangalore Medical College and Research Institute, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Radhika, No. 617, B-4, sharavathi block, NGV, Bangalore - 560047, India. Phone : 9481936444,
E-mail: radhikaobg@yahoo.co.in
Objectives: To study types of worm infestation in pregnancy and to correlate helminthiasis with haemoglobin level in antenatal women presenting in 2nd and 3rd trimester.
Materials and Methods: This prospective cross sectional hospital based study conducted at Vanivilas hospital attached to Bangalore medical college, over a period of sixmonths. Study included 500 pregnant women attending antenatal opd in 2nd and 3rd trimester, selected by systematic random sampling method. Parasitic examination and haemoglobin estimation done respectively with Stool and blood samples collected from study group. Presence of parasites was correlated with haemoglobin percentage.
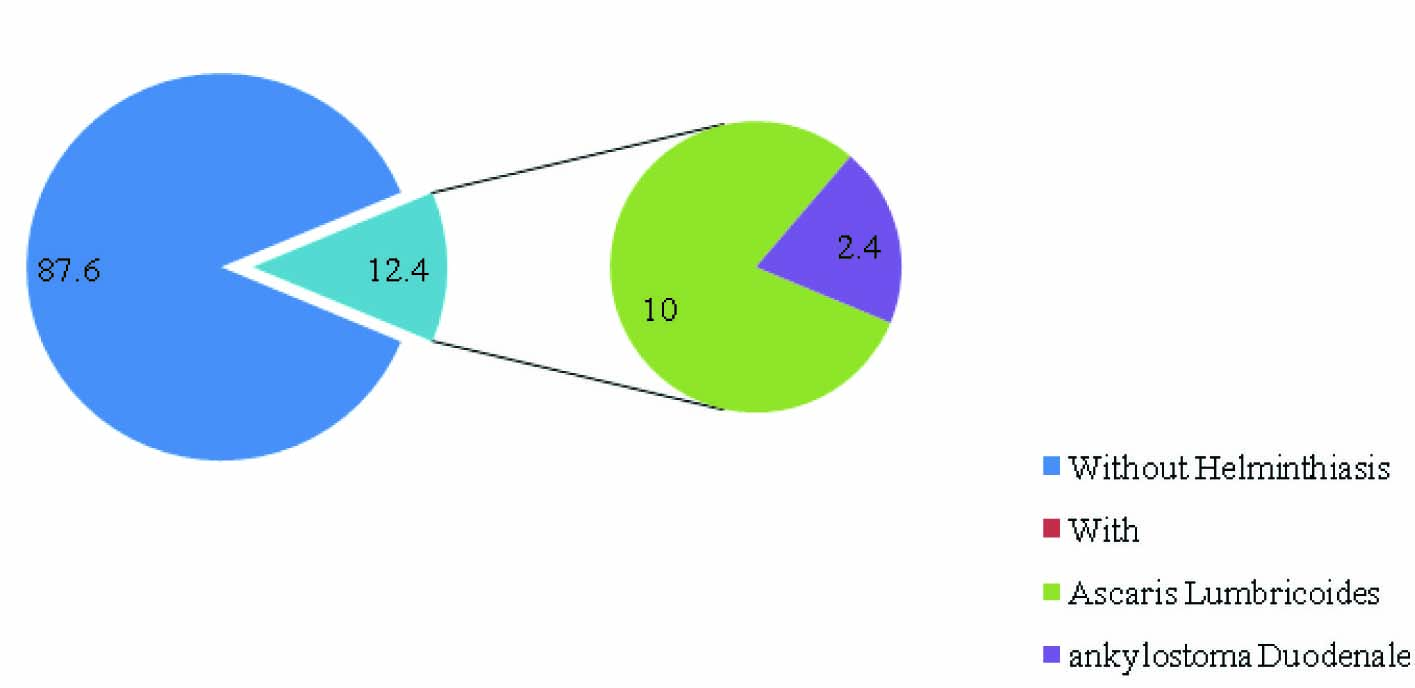
Results: Helminthiasis was found in 62 women (12.4%). All infected women had single type helminth infection. Ascariasis was more commonly found than hookworm (10% Vs 2.4%). Anaemia of various degrees was found in 88.7% of women with helminthiasis as compared to 56.4% women without worm infestation (p-value <0.05).
Conclusion: Helminthiasis is a significant burden in pregnancy and it is associated with anaemia. Hence, the policy of universal administration of anthelminthic drug in pregnancy after first trimester, as recommended by WHO should be practically enforced besides health education.
Introduction
Parasitic disorders particularly soil transmitted helminthiasis (STH) complicating pregnancies have been recognised as important public health problem in developing countries. This is attributable to inadequate attention given to sanitation and personal hygiene [1]. Effects of anaemia on both mother and foetus are well-known.However, understanding helminthiasis as a contributor to anaemia in pregnancy has lagged behind. Bundy and colleagues have estimated that approximately one-third of all pregnant women (44 million out of 124 million pregnancies) in developing countries are infected with hookworm infection [2]. About 1.2 billion people are infected with roundworm (Ascaris lumbricoides) and more than 700 million are infected with hookworm (Necator americans and Ankylostoma duodenale) or whipworm (Trichuris trichura)[3]. Hookworm infection is considered as the leading cause of pathological blood loss in endemic areas [4]. Helminthic infections contribute to severe anaemia through blood loss and micronutrient deficiencies; also malnutrition is associated with helminthiasis [5]. Nutritional deficiency in the setting of pregnancy where there are increased needs can have devastating effects on both mother and foetus.
Materials and Methods
This prospective cross sectional hospital based study was conducted at Department of Obstetrics and Gynaecology of Vanivilas tertiary care hospital attached to Bangalore medical college. Ethical clearance for the study obtained from institute’s ethical committee. Study period was six months (July-December 2010). Study included 500 pregnant women attending antenatal outpatient department selected by systematic random sampling method. Asymptomatic low risk primigravidae with >12 wk of gestation were included in study group after informed consent. Women refusing consent, prior treatment with antheminthics, history of medical disorders, with diagnosis of HIV/HbsAg/syphilis/Toxoplasmosis, on Levamisole treatment and women presenting in labour were excluded from the study. After consent, detailed history and physical examination were done. Participants were provided with labelled screw capped stool sample bottle and labelled blood collection sample bottle. Women were asked to give the stool sample on the same day or the following day. Blood sample for estimating haemoglobin percentage was taken when women returned with stool sample. Collected samples were transported to clinical laboratory attached to medical college within two hours. Microscopic examination of stool sample was done by expert microbiologists. Both saline and iodine preparation of stool samples were made and examined under low power (10x). Confirmation of ova/egg done under high power(40x) magnification. The type of parasite was recorded in format. Haemoglobin percentage was estimated by auto analyser method using blood sample. Haemoglobin less than 10.5g% was taken as anaemia.
Study results were tabulated using EPI-INFO (for student). Chi-square test was used to assess the statistical significance of helminthiasis among study population and its correlation with the haemoglobin level. The variables subjected to the statistical analysis were age, socio-economic status and gestational age.
Results
Five hundred antenatal women who came for prenatal care were subjected to microscopic stool examination for helminthic ova and blood test for haemoglobin estimation. Helminthiasis was found in 62 (12.4%) women [Table/Fig-1].
All women had single type worm infestation.Women belonged to the age group of 18-35 y (mean age – 26.5 y). Majority of women were housewives (86%). About 60% of women had primary and high school educational status.
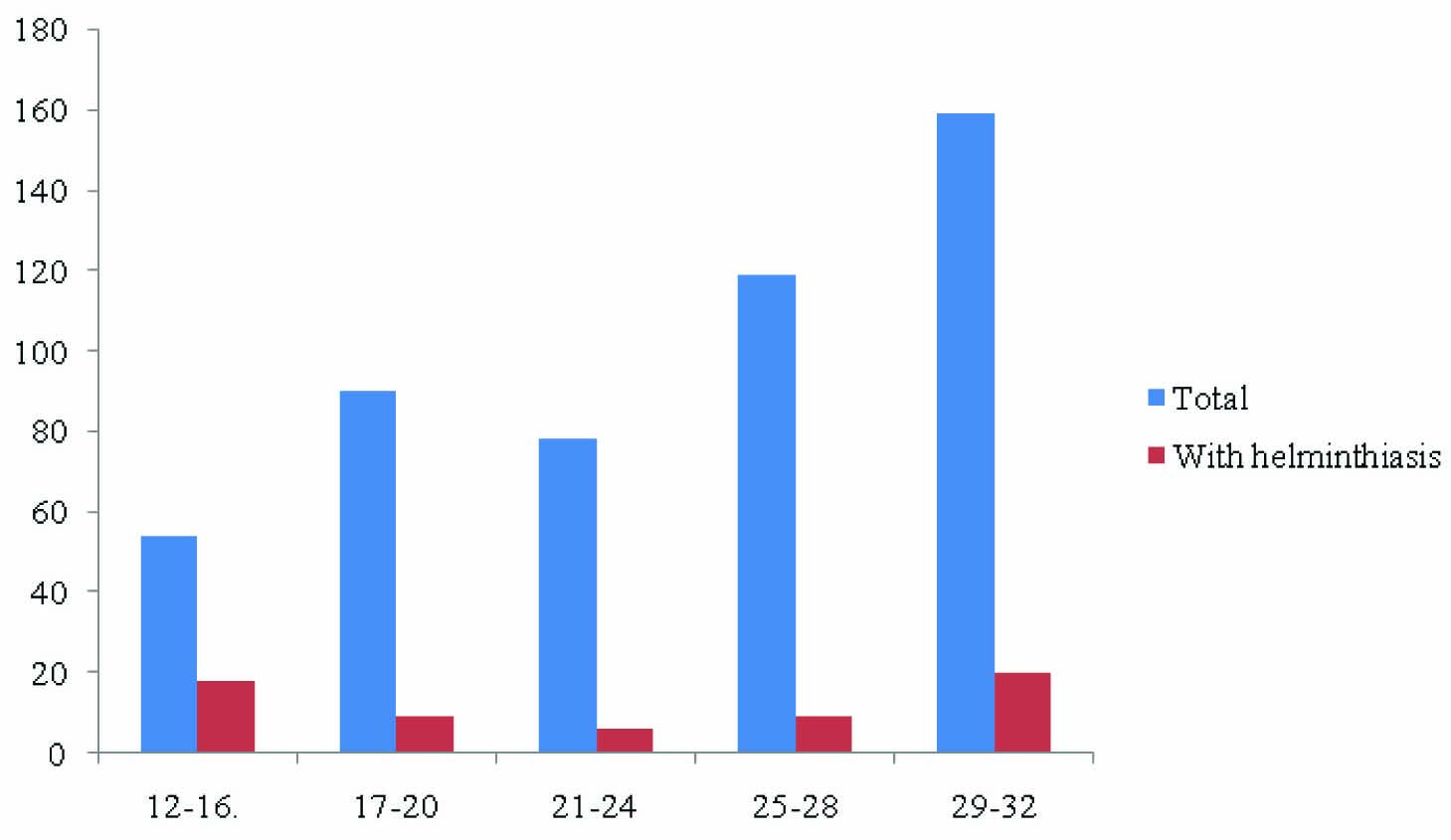
The gestational age of the subjects is depicted in [Table/Fig-2]. Highest prevalence among the groups was noticed in 12-16 wk (33.3%).This indicates that impact of helminthiasis on mother and foetus can be prevented by antenatal screening
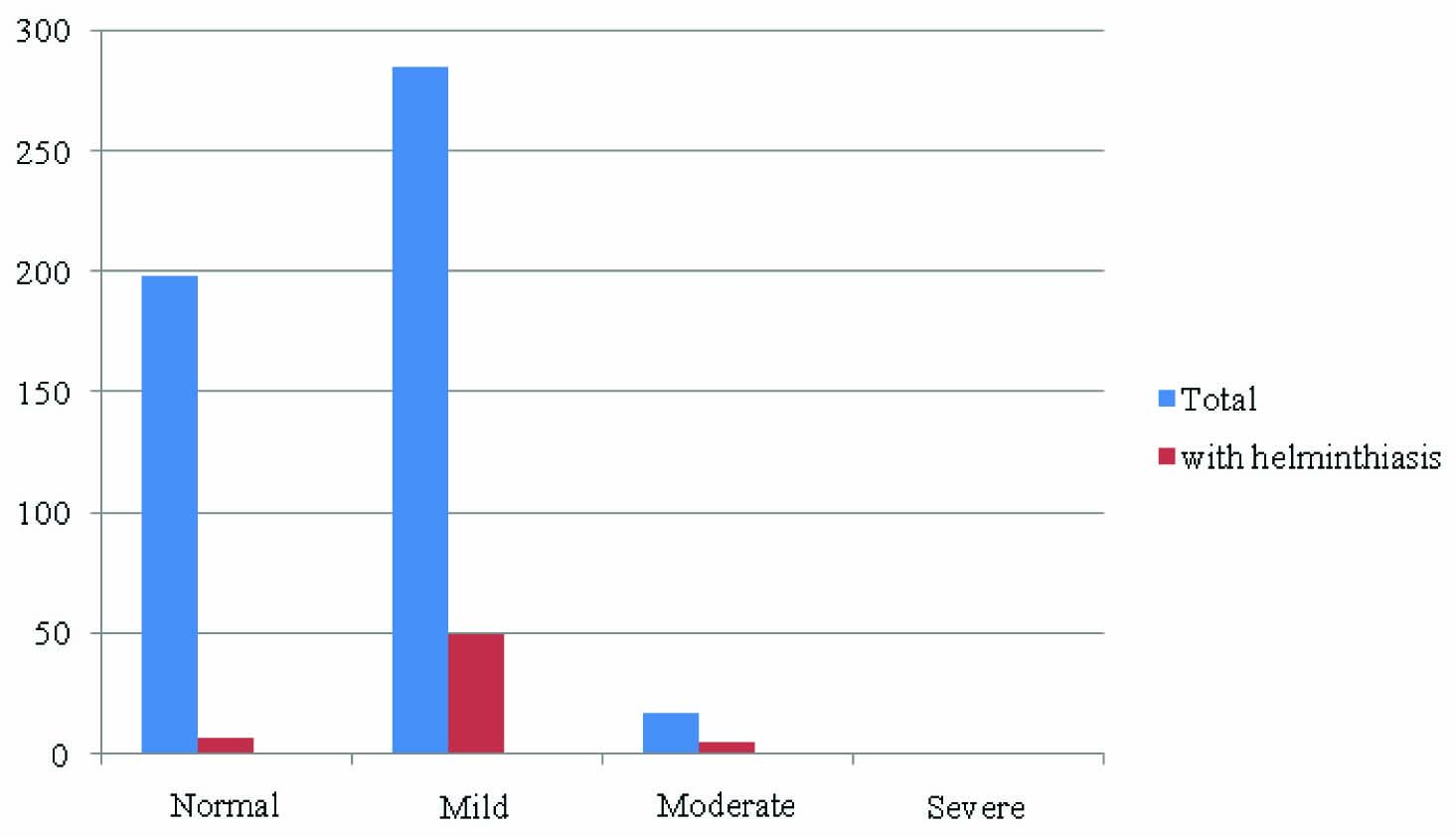
Most of women with helminthiasis had anaemia as compared to women without infestation (88.7% Vs 56.4%), [Table/Fig-3]. Seven women (11.3%) in infected group had normal haemoglobin and all seven had ascariasis. Though anaemia was prevalent among non-infected women majority had only mild anaemia (235 out of 247 women). 80.6% of helminthic infected women had mild anaemia and 8.1% had moderate anaemia. There were no cases of severe anaemia in both groups [Table/Fig-4].
Discussion
Soil transmitted helminthes (STH) though uncommon in developed countries, still commonly encountered in pregnant women in developing countries. There is variation in prevalence among various geographic locations in same endemic area. This study conducted at urban area university College which caters mainly to low socio economic group in urban dwellings. Five hundred asymptomatic primigravidae women who came for routine antenatal check-up were included in the study. 12.4% women had heminthiasis, 10% of whom had ascariasis and 2.4% had hookworm infestation [Table/Fig-5]. Differentiation between type of hookworm ankylostom aduodenale and necator americans not done as it was not practically feasible. All women had single type parasite infection.Species adjusted analysis for this study showed that most important parasite representing a risk, to be found with anaemia in pregnancy was ascaris lumbricoides. A prospective study carried out at university of Nigeria teaching hospital showed that prevalence of 11.8% in pregnant women attending antenatal clinics [1]. A large study conducted on 1042 pregnant women in highly endemic areas of Peru showed overall prevalence rate of 47.22% for hookworm, 82.25% for trichuriasis, 63.92% for ascariasis. Most women in that study had poly parasitic infections [Table/Fig-6]. Only 9.3% of women were free from parasitic infection [6].
In this study anaemia was found in 60%, although those with anaemia did not correspond mainly to infected women. However, those who werenot infected, majority (95%) of women had only mild anaemia. There were no cases of severe anaemia probably because all were booked antenatal cases. Study conducted at Peru showed association between soil transmitted helminthiasis and anaemia in pregnancy [8]. Renee and co-authors studied direct relation between the intensity of hookworm infestation and anaemia and concluded that higher the intensity of hookworm infestation, higher was the proportion of anaemia [6] [Table/Fig-7]. Systematic review of randomised trials by Gulani and colleagues found that deworming increases haemoglobin by 1.71 g/l (95% confidence interval 0.70 to 2.73), which could translate into a small (5-10%) reduction in the prevalence of anaemia [9].
All women were treated with single dose of albendazole (400mg), though it was not part of study criteria. WHO and UNICEF have recommended including anthelminthic treatment in prenatal programs, in areas where the prevalence of hookworm infection exceeds 20–30% [10]. In 2009 a Cochrane review of 9 studies did not produce sufficient evidence to recommend the use of antihelminth medications after the first trimester of pregnancy and highlighted the need for larger-scale randomized controlled trials[11]. Subsequently, in 2010, a large study in Uganda of 2515 pregnant women showed a maternal benefit in preventing anaemia with administration of albendazole during the second and third trimesters of pregnancy only in women with moderate to heavy hookworm infection. In addition, no congenital anomalies were associated with the use of intrapartum anthelminthic medications [12].
Distribution of helminthiasis among study group
Distribution of study group according to gestational age and helminthiasis
Total number of anaemia cases among infected vs noninfected women
| n = 500 | Anaemia - (present) | Anaemia - (Absent) | |
| Helminthiasis – Present | 55 (a) | 7 (b) | (a+b = 62) |
| Helminthiasis - Absent | 247 (c) | 191 (d) | (c+d = 438) |
| (a+c = 302) | (b+d =198) | n = 500 |
Distribution of study group according to severity of anaemia and helminthiasis.Hb( in g% ) Normal >10.5, Mild – 8.5 -10.5, Moderate – 6.5-8.4, Severe – 4.5-6.4
Prevalence of helminthiasis among study group
| Study | Ozumba et al., [1] | Larocque et al., [6] | Dreyfuss et al., [7] | Present study |
| Prevalence among study group | 11.8% | 90.7% | 74.2% | 12.4% |
| Sample size (pregnant women) | 161 | 1042 | 336 | 500 |
Type of parasitic infection among study group
| Type of parasite | Hookworm | Ascariasis | Trichuris |
| Ozumba et al., [1] | Not found | 8.7% | 63.92% |
| Larocque et al., [6] | 47.22% | 63.92% | 82.25% |
| Dreyfuss et al., [7] | 74.2% | Not done | Not done |
| Present study | 2.4% | 10% | Nil |
Prevalence of anaemia among study group
| Larocque et al., [6] | Dreyfuss et al., [7] | Present study |
| Prevalance of Anemia among helminthic pregnant women | 90.7% | 72.6% | 60% |
Conclusion
Soil transmitted helminthiasis in pregnancy is associated with anaemia in pregnancy. Systematic screening for risk factors for anaemia in pregnancy needs to be addressed with emphasis on parasitic infections in developing countries. Universal treatment with deworming agents in pregnant women after first trimester should be practically implemented in developing countries.
[1]. U.C Ozumba, N Ozumba, Patterns of helminthes infections in the gut at the university of Nigeria teaching hospital, Enungu, Nigeria,J Health Sci. 48 :263-268. [Google Scholar]
[2]. DA Bundy, MS Chan, L Savioli, Hookworm infection in pregnancy.Trans R Soc Trop Med Hyg. 1995 89:521-22. [Google Scholar]
[3]. NR De Silva, S Brooker, P Hotez, A Montresor, D Engels, L Savioli, Soil-transmitted helminths: updating the global picture.Trends Parasitol. 2003 19:547-51. [Google Scholar]
[4]. ZS Pawlowski, GA Schad, GJ Stott, Hookworm infection and anaemia - approaches to prevention and control.Geneva: World Health Organization. [Google Scholar]
[5]. LS Stephenson, MC Latham, EA Ottesen, Malnutrition and parasitic helminth infections.Parasitology. 2000 121:S23-38. [Google Scholar]
[6]. R Larocque, M Casapia, E Gotuzzo, TW Gyorkos, Relationship between intensity of soil-transmitted helminth infections and anemia during pregnancy.Am J Trop Med Hyg. 2005 73:789-89. [Google Scholar]
[7]. Dreyfuss Michele L., Stoltzfus Rebecca J., Shrestha Jaya B., Pradhan Elizabeth K., LeClerq Steven C, Hookworms, Malaria and Vitamin A Deficiency Contribute to Anemia and Iron Deficiency among Pregnant Women in the Plains of NepalTrans R Soc Trop Med Hyg. 2007 101(9):899-907. [Google Scholar]
[8]. TW Gyorkos, H Shenker, R Larocque, MR Ugaz, E Gotuzzo, Sociodemographic and dietary correlates of anemia in pregnant women in Peru.Ecol Food Nutr. 2004 43:497-516. [Google Scholar]
[9]. A Gulani, J Nagpal, C Osmond, HPS Sachdev, Effect of administration of intestinal anthelmintic drugs on haemoglobin: systematic review of randomised controlled trials.BMJ 2007 doi: 10.1136/bmj.39150.510475.AE. [Google Scholar]
[10]. WHO, 2002. Prevention and control of schistosomiasis and soil-transmitted helminthiasis. Report of a WHO Expert Committee. Geneva: World Health Organization. WHO Technical Report Series # 912. [Google Scholar]
[11]. BA Haider, Q Humayun, ZA Bhutta, Effects of administration of antihelminthics for soil transmitted helminthes during pregnancy.Cochrane Database Syst Rev. 2009 15:CD005547 [Google Scholar]
[12]. J Ndibazza, L Muhangi, D Akishule, Effects of deworming during pregnancy on maternal and perinatal outcomes in Entebbe, Uganda: a randomized controlled trial.Clin Infect Dis. 2010 50:531-40. [Google Scholar]