Introduction: Lesions of salivary gland are quite common. Clinical examination alone is not able to differentiate between them and pinpoint the exact cause. It would definitely benefit the patient as well as the doctor if they could get an idea of the exact type of lesion affecting the salivary gland. Hence, this retrospective study was undertaken to demonstrate how high resolution ultrasound imaging (HRUSG) can be useful in evaluation of salivary gland lesions.
Materials and Methods: In this retrospective study, imaging findings in patients who underwent HRUSG of salivary glands in the past five years were compiled. Analysis of the imaging findings and clinico-pathological correlation was then performed in this descriptive study.
Results: Out of the 87 patients referred for HRUSG of salivary glands in the last five years, characteristic findings were found in 53 patients. HRUSG diagnosis of Acute Inflammation was made in 19 cases, Chronic Inflammation in 13 cases and Primary Neoplastic Lesions in 11 cases, Metastatic deposits in 3 cases and Salivary Calculus in 7 cases. No obvious abnormality was seen in rest of the 34 patients. HRUSG was found to be 93.33 % sensitive and 98.07% specific for diagnosing neoplastic lesions in salivary glands.
Conclusion: Patients with salivary gland pathologies may present either with clinically assessable symptoms or just with cosmetic deformities due to bulge in the salivary gland. Clinical examination alone cannot pinpoint the etiology. Sonography can satisfactorily enable visualization of the abnormality noninvasively. It not only confirms the presence or absence of pathology but also enables image guided tissue retrieval for final pathological diagnosis.
Salivary glands, Sialoadenitis, Sialolithiasis, Salivary tumour, Ultrasound
Introduction
Problems of salivary gland are quite common in people of all age groups. Clinical examination alone is not able to differentiate between the true nature, location, extent and exact cause of such lesions, as they are not visible to naked eye. It would definitely benefit the patient as well as the doctor if they could get an idea of the exact type of lesion affecting the salivary gland. Hence, this retrospective study was undertaken to demonstrate how high resolution ultrasound imaging (HRUSG) can be useful in evaluation of salivary gland lesions.
Materials and Methods
In this retrospective study, imaging findings in patients who underwent High resolution ultrasound (HRUSG) of salivary glands in the past five years (from May 2009 to February 2014] in the Ultrasound wing of Rural Medical College, Pravara Institute of Medical Sciences (DU), Loni were compiled. Appropriate consent from Institutional Ethical Committee was obtained for the study. The examination was carried out using high frequency linear transducer (5-11 MHz) of Sonoline G-60 Siemens Color Doppler Ultrasound Machine. Analysis of the imaging findings and clinico-pathological correlation was then performed in this descriptive study.
The aim was to find the common salivary gland lesions presenting in our setup and to study the spectrum of such lesions using HRUSG.
Results
In this study there were total 87 patients, 54 males and 33 females. The range of age group was between 5 to 68 y of age.
Out of the 87 patients referred for HRUSG of salivary glands in the last 5 year, characteristic findings were found in 53 patients. HRUSG diagnosis of Acute Inflammation was made in 19 cases (35.84%), Chronic Inflammation in 13 cases (24.52%) and Primary Neoplastic Lesions in 11 cases (20.75%), Metastatic deposits in 3 cases (5.66%) and Salivary Calculus in 7 cases (13.20%). No obvious abnormality was seen in rest of the 34 patients. HRUSG was found to be 93.33 % sensitive and 98.07% specific for diagnosing neoplastic lesions in salivary glands. One case was labeled as neoplasm on HRUSG but was subsequently found to be an enlarged lymph node on cytology (False Positive). Similarly, one case was labeled as an enlarged node on HRUSG but was subsequently proven to be a metastatic deposit on cytology (False Negative).
HRUSG could satisfactorily diagnose all the salivary gland lesions. However, it could not differentiate between different types of malignant lesions. Benign neoplasms and enlarged lymph nodes with loss of internal architecture could also not be differentiated satisfactorily.
Discussion
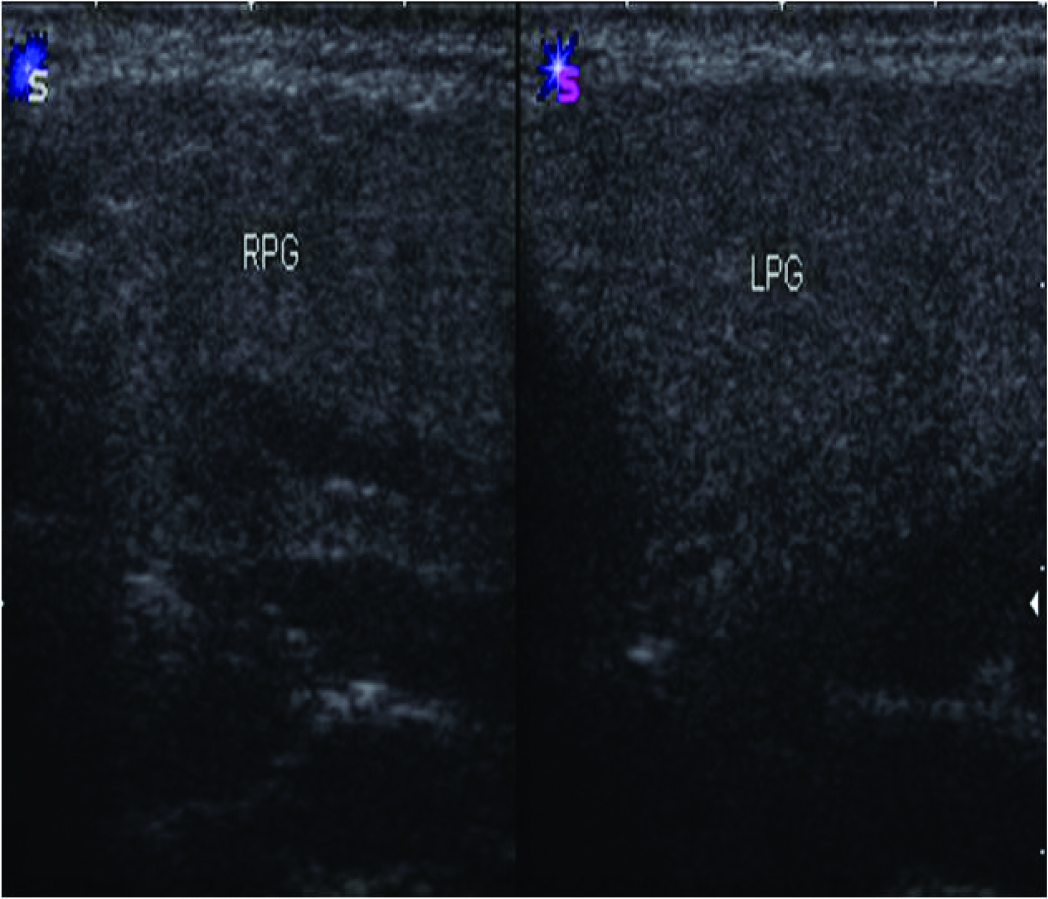
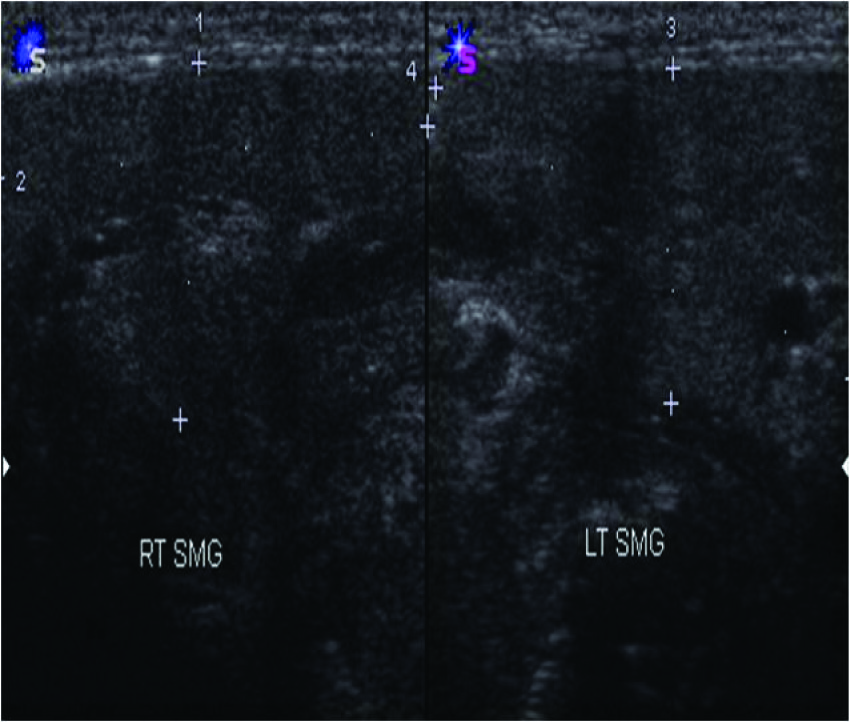
The parotid and submandibular salivary glands can be visualised satisfactorily with High Resolution Ultrasound (HRUSG) [1-4]. The parotid salivary glands are seen in retromandibular region as echogenic triangular structure[Table/Fig-1]. Normal parotid gland appears homogenous and of increased echogenicity relative to adjacent muscles on ultrasound. This increased echogenicity is due to its fatty glandular tissue composition. The retromandibular vein differentiates between the superficial and deep part of the parotid gland [1]. The submandibular salivary glands are located in the submandibular fossa of the body of mandible, within the submandibular triangle in the plane of anterior belly of digastric muscle. It has homogenous echo texture on ultrasound which is slightly hyper echoic compared with surrounding muscle [Table/Fig-2].
Occasionally, bean-shaped, hypo echoic structures may be seen in the substance of salivary glands, more commonly in the parotid gland indicative of reactive, hyperplastic lymph nodes. Normal facial nerve branches are not demonstrated on HRUSG routinely [5]. Blood flow pattern in the glands can be assessed by Colour Doppler Ultrasound[5,6].
Panorama of salivary gland lesions as seen on HRUSG in this study was as follows: (A) Inflammations of the salivary glands [7]
1) Acute Sialoadenitis [Table/Fig-3] is seen on HRUSG as enlargement of the involved salivary gland and increased vascularity on color Doppler. Enlarged lymph nodes can be seen within the gland. HRUSG can demonstrate abscess formation in the gland. Sialoadenitis of viral aetiology is usually bilateral, while that of bacterial cause is unilateral.
2) Chronic Sialoadenitis [Table/Fig-4] has almost same appearance on HRUSG as Acute Sialoadenitis, but the enlargement gland and the increase in vascularity on color Doppler is comparatively less. More enlarged lymph nodes can be seen within and around the gland. This entity is usually unilateral. When bilateral and associated with dryness of mouth and marked heterogeneous appearance of glands; Sjögren’s syndrome must be considered [8]. Tuberculosis may present as an ill-defined hypo echoic mass in the salivary glands demonstrating acid fast bacilli when biopsied [9].
3) Sialolithiasis Occurrence of calculi is common in the submandibular gland than in the parotid gland. When the ducts of these glands get blocked, the patients become symptomatic [5].
The calculus is seen as linear or curvilinear echogenic structures having a strong posterior acoustic shadowing [Table/Fig-5]. Tiny 2-3 mm sized calculi may be seen as hyper echoic foci without any posterior acoustic shadowing.
B) Tumors of the salivary glands [7]
Most of the salivary gland tumours are benign in nature. Commonest site of salivary tumor is the parotid gland. Malignant tumors are common in smaller salivary glands [10]. HRUSG can enable the assessment of benignity and malignancy of parotid masses [11].
1) Pleomorphic adenoma
It is the commonest tumor of the salivary gland. Most common site is the parotid gland. HRUSG demonstrates them as solid, homogeneous, hypo echoic, well marginated and multilobulated lesions within the substance of salivary gland [Table/Fig-6]. Cystic appearance and occurrence of calcifications is rare. Peripheral as well as intralesional vascularity with typical “basket pattern” flow is diagnostic.
2) Acinar cell carcinoma
It is a malignant tumor of the salivary gland. HRUSG typically demonstrates it as a round lesion [Table/Fig-7], having almost similar sonographic appearances as a Pleomorphic adenoma. Low grade malignancies are well-defined whereas high grade lesions have ill-defined margins.
3) Metastatic Lesions
Primaries in region of head and neck, commonly metastasise to nodes in salivary gland. Squamous cell carcinoma of face and neck and malignant melanoma of the head and face are known to
metastasise to salivary glands [Table/Fig-8].
C) Miscellaneous Lesions of the Salivary Glands [7]
1) AIDS related lymphoepithelial cysts are seen as multiple anechoic lesions in the swollen glands[Table/Fig-9]. These lesions are usually bilateral and the patient is positive for Human Immuno- Deficiency virus infection [12].
2) Post Radiotherapy Changes are seen in the form of inflammation of salivary glands. Sialoadenitis occurring in patients who have received radiotherapy for head and neck cancers, presents in two stages. In the acute stage on HRUSG glands are enlarged and appear diffusely hypo echoic [Table/Fig-10]. In the chronic form the glands are small and shrunken and difficult to differentiate from adjacent soft tissues [13,14]. Postradiotherapy xerostomia is commonly seen in patients on radiotherapy for head and neck malignancies. It adversely affects the quality of life. HRUSG shows increased conspicuity of intraparotid ducts and altered heterogeneous appearance of the post-radiotherapy glands might and few hyper echoic lines indicating fibrosis.
Comparative analysis of the findings in our study was performed with other similar studies in which findings on ultrasound were compared with cytology/biopsy reports and statistical parameters of sensitivity and specificity were arrived at
[Table/Fig-11] shows that different studies across the world [15-18] have found that Ultrasound has a high sensitivity and high specificity in evaluating neoplastic lesions of salivary glands. The results in present study too shows high sensitivity (93.33%) and high specificity (98.07%) and are thus are in agreement with findings of other studies[19].
HRUSG appearance of Normal Parotid Glands., HRUSG appearance of Normal Submandibular Glands
HRUSG appearance of Normal Submandibular Glands
HRUSG appearance of acute inflammation in salivary glands

HRUSG appearance of chronic inflammation in salivary glands

HRUSG appearance of sialolithiasis

HRUSG appearance of parotid adenoma

HRUSG appearance of acinar cell carcinoma

HRUSG appearance of metastases in salivary glands

HRUSG shows HIV associated lymphoepithelial cysts

HRUSG shows HIV associated lymphoepithelial cysts

Comparative analysis of the findings in present and other similar studies
| Study et al., | n | True Positive | False Positive | True Negative | False Negative | Sensitivity (%) | Specificity (%) |
| Wan [15] | 31 | 05 | 00 | 01 | 25 | 83 | 100 |
| Taki [16] | 18 | 05 | 01 | 02 | 10 | 71 | 91 |
| Naqvi [17] | 108 | 25 | 00 | 01 | 82 | 96 | 100 |
| Breeze [18] | 114 | 30 | 00 | 01 | 84 | 97 | 100 |
| Present Study | 87 | 14 | 01 | 51 | 01 | 93.33 | 98.07 |
Conclusion
HRUSG is thus an important and often the first imaging modality for the evaluation of the salivary glands. It can easily demonstrate normalgland as well as any abnormalities in the glands as shown in thisstudy. Moreover it is economical, widely available and radiation free.Hence it forms the backbone of imaging of the salivary glands. Onlylimitation is that this is an operator dependent imaging modality.
[1]. N Gritzmann, Sonography of the salivary glands.AJR Am J Roentgenology 1989 153(1):161-66. [Google Scholar]
[2]. R Chandak, S Degwekar, RR Bhowte, M Motwani, P Banode, M Chandak, An evaluation of efficacy of ultrasonography in the diagnosis of head and neck swellingsDentomaxillofacial Radiology. 2011 40(4):213-21. [Google Scholar]
[3]. S H Liyanage, S P Spencer, K M Hogarth, J Makdissi, Imaging of salivary glandsImaging 2007 19(1):14-27. [Google Scholar]
[4]. F Alyas, K Lewis, M Williams, AB Moody, KT Wong, AT Ahuja, Diseases of the submandibular gland as demonstrated using high resolution ultrasoundThe British Journal of Radiology. 2005 78(928):362-69. [Google Scholar]
[5]. C Martinoli, LE Derchi, L Solbiati, G Rizzatto, E Silvestri, M Giannoni, Color Doppler sonography of salivary glands. AJR Am J Roentgenol. 1994 163(4):933-41. [Google Scholar]
[6]. C Martinoli, F Giovagnorio, F Pretolesi, LE Derchi, Identification of feeding arteries to establish the intra- or extraparotid location of jugulodigastric nodules: value of color Doppler sonography.AJR Am J Roentgenol. 2000 175(5):1357-60. [Google Scholar]
[7]. RC Kamble, AN Joshi, PJ Mestry, Ultrasound Characterization of Salivary Lesions.Int J Otorhinolaryngol Clin. 2013 5(1):2013-90. [Google Scholar]
[8]. Y Takagi, Y Kimura, H Nakamura, M Sasaki, K Eguchi, T Nakamura, Salivary gland ultrasonography: can it be an alternative to sialography as an imaging modality for Sjogren’s syndrome? Ann Rheum Dis. 2010 69(7):1321-24. [Google Scholar]
[9]. R Feld, LN Nazarian, L Needleman, AS Lev-Toaff, SR Segal, VM Rao, Clinical impact of sonographically guided biopsy of salivary gland masses and surrounding lymph nodesEar Nose Throat J. 1999 78(12):905-908. [Google Scholar]
[10]. N Gritzmann, A Hollerweger, P Macheiner, T Rettenbacher, E Hubner, Sonography of the salivary glands.European Radiology 2003 13:364-75. [Google Scholar]
[11]. S Wu, G Liu, R Chen, Y Guan, Role of ultrasound in the assessment of benignity and malignancy of parotid masses.Dentomaxillofacial Radiology. 2012 41(2):131-35. [Google Scholar]
[12]. C Martinoli, F Pretolesi, B Del, LE Derchi, D Mecca, M Chiaramondia, Benign lymphoepithelial parotid lesions in HIV-positive patients: spectrum of findings at gray-scale and Doppler sonography.AJR Am J Roentgenol 1995 165(4):975-79. [Google Scholar]
[13]. S Cheng, V Wu, D Kwong, M Ying, Assessment of post-radiotherapy salivary glands. The British Journal of Radiology 2011 84(1001):393-402. [Google Scholar]
[14]. M Imanimoghaddam, M Rahrooh, Z Tafakhori, S Zahedanaraki, F Homaeieshandiz, Changes of parotid and submandibular glands caused by radiotherapy—an ultrasound evaluationDentomaxillofacial Radiology. 2012 41(5):379-84. [Google Scholar]
[15]. Y-L Wan, S-C, Chan, Y-L, Chen, Ultrasonography-guided core-needle biopsy of parotid gland masses.AJNR Am J Neuroradiol. 2004 25:1608-12. [Google Scholar]
[16]. S Taki, T Yamamoto, A Kawai, Sonographically guided core biopsy of the salivary gland masses: safety and efficacy.Clin Imaging. 2005 29:189-94. [Google Scholar]
[17]. SQH Naqvi, S Shaikh, SQA Shah, Ultrasound-guided core needle biopsy for salivary gland lesions.Gomal J Med Sci. 2008 :6 [Google Scholar]
[18]. Y Breeze, Y Andi, H Williams, The use of fine needle core biopsy under ultrasound guidance in the diagnosis of a parotid massBr J Oral Maxillofac Surg 2009 47:78-79. [Google Scholar]
[19]. N Gritzmann, Sonography of the neck: current potentials and limitations.Ultraschall Med. 2005 26(3):185-96. [Google Scholar]