HIV/AIDS is one of the most devastating illnesses that humans have ever faced. The pandemic began late in Asia; however the situation is rapidly changing [1]. It is estimated that currently more than 2.54 million people in India are infected with HIV. Epidemiological analysis of reported HIV/AIDS cases reveals that HIV/AIDS is affecting mainly young people in the sexually active age group. The majority of the HIV infections (87.7%) are in the age group of 15-44 y. In the HIV sentinel surveillance (2003), males account for 73.5% of AIDS cases and females 26.5% [2].
Depression is the most commonly reported psychiatric disorder. Despite its prevalence, depression is commonly underdiagnosed and consequently untreated in general medical population. In primary care, physicians miss between one half to two-thirds of patients having depression. Depression is often viewed as an expected reaction to a medical illness [3,4]. Bing et al., reported that as many as one in three persons with HIV may suffer from depression [5].
Depression in PLHA(people living with HIV/AIDS) could be triggered by stress, difficult life events, side effects of medications, or the effects of HIV on the brain and it might even accelerate HIV’s progression to AIDS [6,7].
The economic cost of HIV/AIDS treatment to the people is immense often landing the sufferer and his family in abject penury. At times, this leads to shunning by family, broken homes, loss of employment and sale of assets to pay for treatment. Negative social consequences like stigma is a problem that sufferer almost always faces. This often leads to restricted options for marriage, employment and may even lead to divorce. The stigma attached to the disease is often a leading cause of patient landing up with severe depression [8].
HIV/AIDS though such a big public health problem worldwide, not enough data is available regarding association of HIV and Depression. Therefore this study was undertaken to evaluate the association between HIV/AIDS and depression in an Indian setting.
Materials and Methods
The study was conducted on patients under HIV care at the ART (Anti-retroviral treatment) center of Guru Teg Bahadur Hospital and associated University College of Medical Sciences, Delhi. One hundred sixty patients of age group 14-60 y meeting the selection criteria were recruited.
Informed consent was taken from each patient and full confidentiality was assured. The study was approved by Institutional Ethical committee. The patient was assured that his replies are in no way going to prejudice the treatment given.
The patients refusing to give consent, having past or family history psychiatric illness, bereavement within 3 month, female patient in post-partum period, history of chronic physical disease or on steroid treatment, patient not on ART or on treatment for more than a year were not included.
A detailed history including socio-demographic profile, symptomatology, treatment, past and personal history was also taken. The patients were administered the Centre for Epidemiologic Studies-Depression (CES-D) scale to detect depression. The CES-D scale is a pretested instrument used to assess the risk of depression in patients and has excellent psychometric properties [9,10]. The CES-D instrument contains 20 items (score range 0-60) assessing depressive symptoms. A competitive score of 16 or higher indicate depression.
Once the interview was completed the patient was encouraged to speak out his concerns and queries. He/ She were advised to continue in HIV care with regular visits to the centre’s counselor. The data collected was analysed using SPSS software.
Results
Out of 160 patients surveyed 94 (58.75%) were depressed. The mean age for depressed patients was 30.59 y as compared to 30.03 y of non-depressed indicating that age does not significantly influences depression. The prevalence of depression was higher in females (61.3%) as compared to males (58.1%) and transgender (50%).
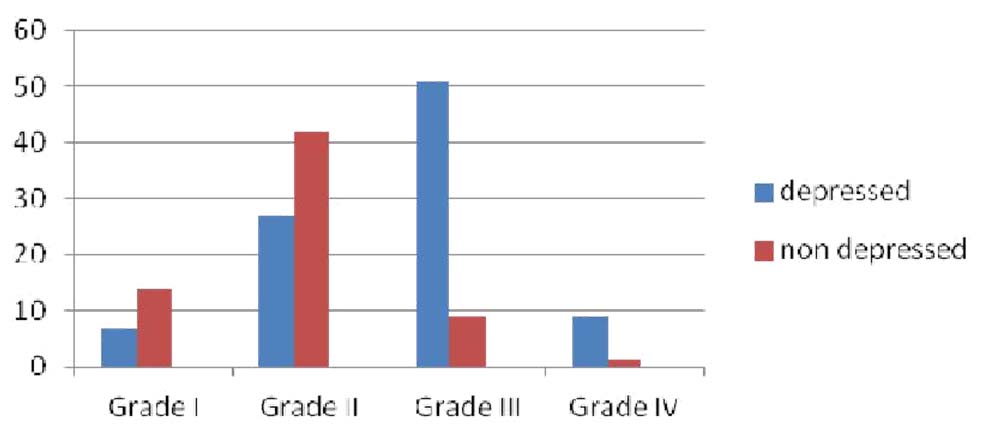
According to WHO staging [11] [Table/Fig-1], depression was found to be increasing according to severity of disease (χ2=37.335. p<0.001).
Depression according to WHO grading of HIV/AIDS
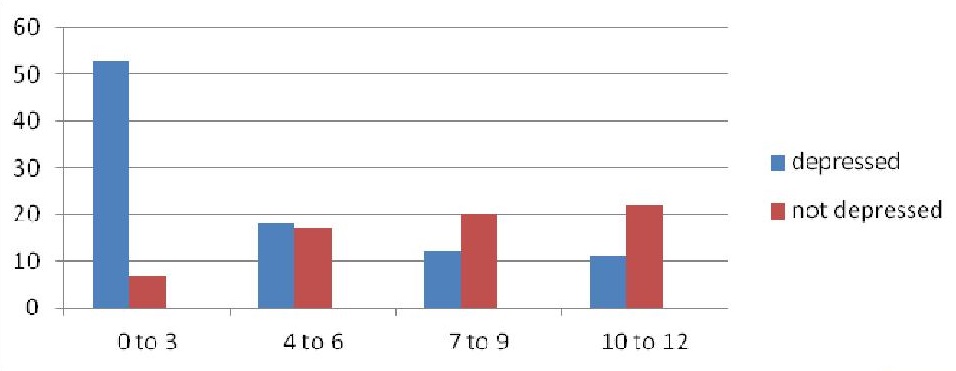
[Table/Fig-2] indicates that the prevalence of depression decreases with duration of treatment with ART (χ2=24.662. p<0.001).
Prevalence of depression (y-axis) according to duration of ART treatment (x-axis)
According to employment, prevalence of depression was higher in unemployed (70.6%) than those working as government employee (46.6%) or in private sector (43.6%) and 71.4% were working as a daily wager. This was statistically significant (χ2=6.466. p=0.01). According to the nature of occupation, a high percentage of depression was found in laborers (84.6%), drivers (91.67%), army personnel (100%) and commercial sex workers (CSW) (80%). It correlates well with the high risk environment of their work (χ2=35.663. p<0.001). Depression was highest in those lost their jobs due to illness followed by those who could not work due to ill health. The longer was the duration, higher was the prevalence of depression.
A high prevalence of depression was found in the uneducated and in patients that attended school till lower standards (χ2=27.685. p<0.001). The rate of depression in patients belonging to joint families was 71.9% as compared to patients belonging to nuclear (49.3%) and three generation (43.75%) families (χ2=6.779. p=0.009).
High prevalence of depression was seen in patients with low income groups i.e. those not earning money or earning upto Rs 5000/- than in higher income groups (χ2=20.123. p<0.001). A similar relationship to family income was also seen. Those with low family income had a greater prevalence of depression as compared to patients with higher family income.
A high prevalence of depression was seen in patients that had migrated to Delhi (74%) and those living outside Delhi (85%) but coming to Delhi to take their medications. Therefore migration is a risk factor for depression in patients (χ2=35.7. p<0.001). No relation to depression was seen regarding the reason for migration. The prevalence of depression was statistically higher in patients who migrated from villages, when migration was recent and in those living in rented houses.
Married had a comparatively lower prevalence of depression as compared to unmarried, divorced or widows/widowers (χ2=5.28 p=0.02). A high prevalence of depression was seen in patients not living with their spouse (100%) as compared to those patients staying with their spouse (47.7%) (χ2=14.15. p=0.002). Depression was high in patients who did not reveal the test result to their spouse (100%).
When family support was analysed, a low prevalence of depression was seen in patients having a good family support (31%) as compared to those having indifferent (80.4%) and bad (80.8%) family support (χ2=39.05. p<0.001). A low prevalence of depression was seen in patients having a good social support (27.5%) as compared to those patients having indifferent (68%) and bad social support (100%) (χ2=48.774 p<0.001).
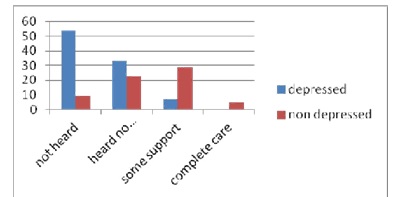
A high prevalence of depression was seen in patients who had not heard of NGO’s (85.7%) and also, heard but not received any support (59%) as compared to patients having received some support (19.4%) and complete care (0%) therefore pointing out the importance of NGO’s in the mental health of the patients taking ART χ2=39.511. p<0.001) [Table/Fig-3].
Prevalence of depression with respect to NGO support
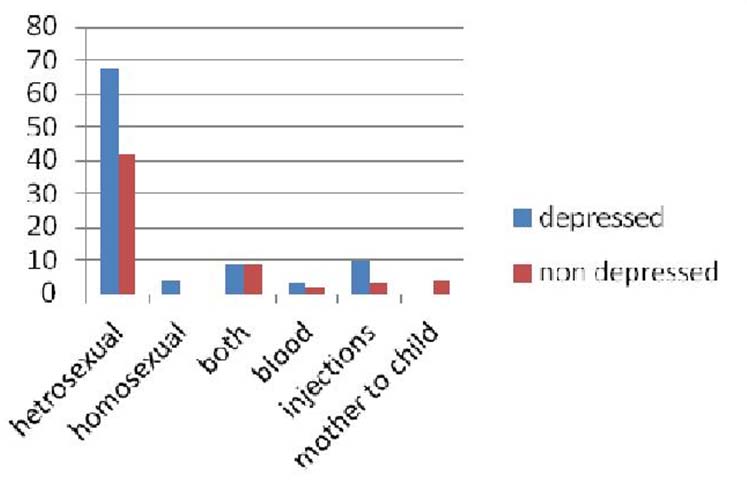
Heterosexual route accounted for most number of patients with HIV/AIDS [Table/Fig-4].
Prevalence of depression according to route of transmission
A high prevalence of depression was seen in patients who visited commercial sex workers (CSW) (70%) as compared to those who did not visit (56.4%). Those who visited commercial sex workers, 70% went to females, 2% to males and 28% to both males and females (χ2=2.524. p=0.1).
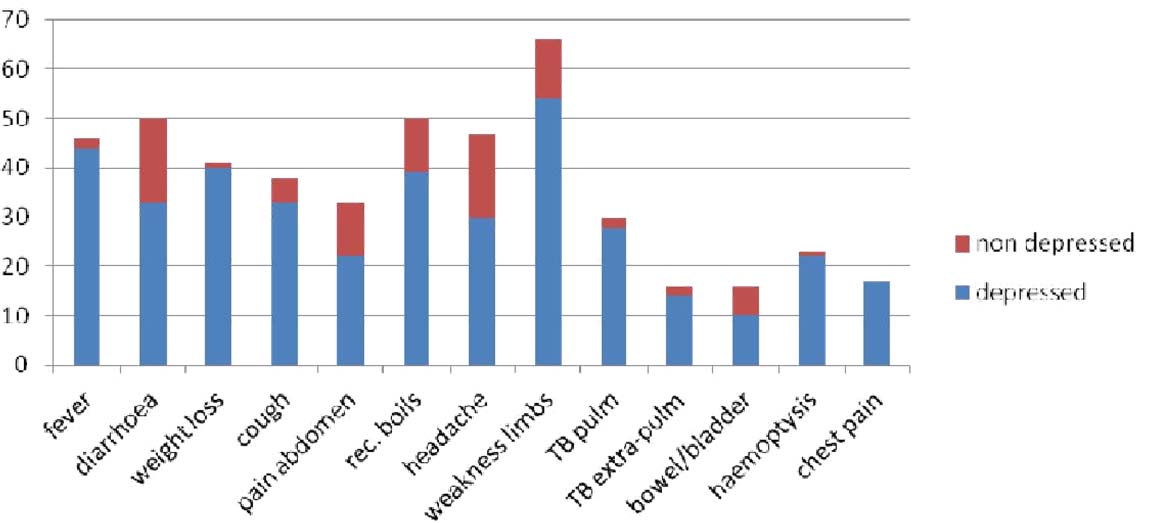
The prevalence of depression according to to physical complaints are shown in [Table/Fig-5].
Prevalence of depression with respect to current illness
A high prevalence of depression was seen in females having irregular menses (82%) or painful menses (χ2=13.237. p=0.003). A high prevalence was found in mothers who had home delivery (95%) and those who did not immunize their children (94%) (χ2=21.604. p<0.001).
Discussion
The prevalence of depression in the present study was 58.75%. This is in comparison to a study by Berger-Greenstein et al., [12] where 72.9% of the patients were found to be depressed but the sample size of the study was small.
Mood disorders, depression in particular, are the most frequent psychiatric complication associated with HIV disease. In fact, lifetime prevalence of depressive disorders range from 22 to 61% in HIV-positive populations. These rates are significantly higher than estimates of lifetime and current diagnosis of major depression in community samples [13]. The prevalence of depression according to gender was not significantly different. But Nogueira et al., [14] had reported an increased prevalence of depression among females.
The prevalence of depression increases with the severity of symptoms. Thus more severe the disease more is its effect on the mental health of the patient. The prevalence of depression decreases with the duration of therapy. This can be attributed to the fact that the treatment decreases the symptoms of the disease and helps the patient to lead a fuller and productive life.
Prevalence of depression was higher in patients who were unemployed and daily wagers. This may be because economical insecurity leads to stress, frustration, dysfunctional family life and feeling of worthlessness. They have a greater chance of developing high risk behavior. According to the nature of occupation, a high percentage of depression was found in laborers, drivers, army personnel, CSW and other daily wagers. It correlates well with the high risk environment of their work. A study by Hutton et al., [15] also reported the direct relationship of unemployment to depression in HIV patients.
A high prevalence of depression was found in the uneducated and lowly educated indicating that the level of education plays an important role in the prevalence of depression in patients. Patients belonging to joint families had a greater prevalence of depression. This can be attributed to the increased scrutiny by the other family members and decreased involvement of the patients in the family matters.
Self and family income plays an important part in the economical and social stability of the person. Patients with nil or low self and family incomes had a greater prevalence of depression. Knowlton et al., [16] stressed upon the importance of financial stability and social support in the mental health of HIV patients.
A high prevalence of depression was seen in patients that had migrated to Delhi. Migration is a risk factor for depression in patients as the people are economically and socially vulnerable. They come to the city for job opportunities and to make money but often indulge in high risk activities. Patients living outside the city are also at an increased risk as they usually have to travel a lot to get to the ART centre. This leads to more frustration and high dropout rates.
Those patients that are divorced or widow/widower have a very high prevalence of depression as they have to deal with stresses of taking care of their children and families by themselves and face the stigma from the society.
More patients who did not reveal the test result of HIV/AIDS to their spouse and those having a bad and indifferent relationship were found to be depressed. In a study by Himelhoch et al., [17], the importance of disclosing their HIV status to their spouse decreases the prevalence of mental health disorders and increases the adherence to treatment.
Family and social support in an illness like HIV/AIDS is very important. It provides mental, economical and social stability to the patients. It also provides warmth and care to the patient in need and decreases the stresses faced by the patient. This is in accordance with the previous studies [14,18] which stated the importance of good family and social support in the mental health of the patient.
NGO’s have a big role to play in the overall health of patients with HIV/AIDS [19]. They form a bridge between the government health services and the patient. They also provide counseling and support to the patient. A high prevalence of depression was seen in patients that had not heard of NGO’s and heard but not received any support.
A high prevalence of depression was seen in patients who visited commercial sex workers. This is due to the fact that the stress and frustration drives them to visit the CSW to have a good time but it affects their mental health as well.
Those patients that lived in rented houses had a greater prevalence of depression [18]. Illness often leads to loss of work and decreased earning capacity of the patient making him unable to pay the rent.
Depression is a very important factor in the adherence of ART regimen. Hutton et al., [15] emphasized that the depressed patients are six times more likely to miss at least one dose of ART regimen. Therefore early detection and effective treatment of depression goes a long way in improving the adherence to ART and thus improving the quality of life.