Context: This study is about documentation of a technique which includes a combination of both hernioplasty and Herniorrhaphy, and its outcome in terms of recurrence rate and postoperative complications. It also compares the outcome of this method with routinely used techniques reported in the literature.
Materials and Methods: LR with Herniorrhaphy was performed in the patients admitted with inguinal hernia under concerned surgeon. Their follow-up was assessed after 12 months. Incidences of recurrence rate and other postoperative complications like painful scar, atrophy of testis, urinary retention, hematoma, sinus and infection were noted and compared with other techniques of repair from published data.
Statistical Analysis: was carried out by calculating the mean, standard deviation (SD), percentage and incidence rates.
Results: LR with Herniorrhaphy performed in 475 patients showed recurrence rate of <<0.01% (n=1) and very low incidences of other postoperative complications like painful scar (0.01%, n=5), sinus (0%, n=0), atrophy of testis (0%, n=0), retention of urine (0.01%, n=6), hematoma (<<0.01%, n=1) and infection (0%, n=0); as compared to published data with different techniques.
Conclusion: LR with Herniorrhaphy can be used for open inguinal hernia repair as the gold standard procedure as it has got low recurrence rate and other postoperative complications as compared to other techniques. However, the result of this study is based on the data from a single center, thus we recommend multicentric trials to test the efficacy of this technique.
Complication, Direct, Groin, Haematoma, Hernioplasty, Herniorrhaphy, Inguinal, Indirect, Painful scar, Sinus, Swelling
Introduction
Inguinal hernia is one of the biggest challenges in surgical practice because of its frequency, complexity as well as the socio-economic consequences. The incidence and prevalence of inguinal hernia are not precisely known [1]. Inguinal hernia repair is the only cure; spontaneous recovery has never been reported [2]. The chance of a person having to undergo an inguinal hernia operation during his/her life is quite high, 27% in the case of men and 3% in the case of women [3].
Inguinal Hernia repair includes various techniques such as Herniotomy only in children and in adults Bassini’s repair, different types of Darnings, mesh plug, Lichtenstein’s repair, Prolene Hernia System (PHS) and many more modifications. More recently laparoscopic approach has been added. The most important criteria for the choice of repair methods are recurrence rates, postoperative pain, testicular atrophy and the length of convalescence and ease of performance. Until the last decade Shouldice technique 1945 (double breasting of tissues) was regarded as the standard for open hernia repair in Europe [4]. The low recurrence rate as claimed by Shouldice could not be achieved by surgeons in non-specialised centres [5,6]. Using patches and plugs tension-free techniques repair have produced excellent results, with low morbidity compared with conventional methods [7,8].
In our center, Dhiraj General Hospital which is a 1,200 bedded hospital catering to rural population of Vadodara and Waghodiya of Gujarat state, most teams in the general surgery service under both emergency and elective settings undertake open inguinal hernia repairs. In our unit we adopted the Lichtenstein method along with posterior wall repair, which uses a nonabsorbable mesh along with nonabsorbable suture to achieve tension repair, for open inguinal hernia surgery. In the present study, we sought to report our experience in inguinal hernia operation by using Lichtenstein Repair with Herniorrhaphy (posterior wall repair) over a four-year period.
The primary objective of this study was to compare the hernia recurrence rate and other post-operative complications with our method against published data, and our secondary objective was to report the incidence of post- operative complications after hernia repair such as painful scar, sinuses, atrophy of testis, infection, hematoma/seroma and urinary retention.
Materials and Methods
The Study Setting
This was a prospective study, which was carried out over a period of four years (September 01, 2009 to August 31, 2013) in the Department of Surgery of Dhiraj General Hospital, which is a 1200-bedded multispecialty hospital, which caters to the rural population of Vadodara and Waghodiya, Gujrat, India.
All the surgical patients with inguinal hernia, admitted to the hospital during September 01, 2009 to August 31, 2013, and were willing to participate, were enrolled for the study.
Before their enrolment, all the participants were explained about the nature and the purpose of the study. Consents were obtained from the patients.
The Study Subjects
A total of 479 patients who fulfilled the below mentioned criteria were enrolled in the study. Four patients missed the follow-up after surgery and hence, were excluded from the study. Thus, a total of 475 patients were enrolled in the study. Out of which 16 were emergency cases, while remaining 459 were electives.
All the patients above 20 years of age with inguinal hernia and those who were willing to give informed consent were included in the study.
While, the patients who were not willing to give informed consent for open surgery, those who were suffering from critical or terminal illness, those who were already enrolled in the study and the patients with immune-compromised statuses were excluded from the study.
The demographic profile, complete histories, information on the vitals and relevant systemic examinations of all the patients who were fitting in the inclusion criteria and willing to participate in the study were recorded in a proforma and the patients were subjected to the following investigations – X-ray chest, PA view, complete blood count (CBC) with the use of a ‘Sysmex KX21 Three Part Differential Automated Hematology Analyser’, Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein (CRP) by the latex agglutination method (the CRP Latex Kit was manufactured by Rapid Diagnostics, Pvt. Ltd.) and other relevant investigations in case required to rule out secondary pathology.
Procedure of Repair
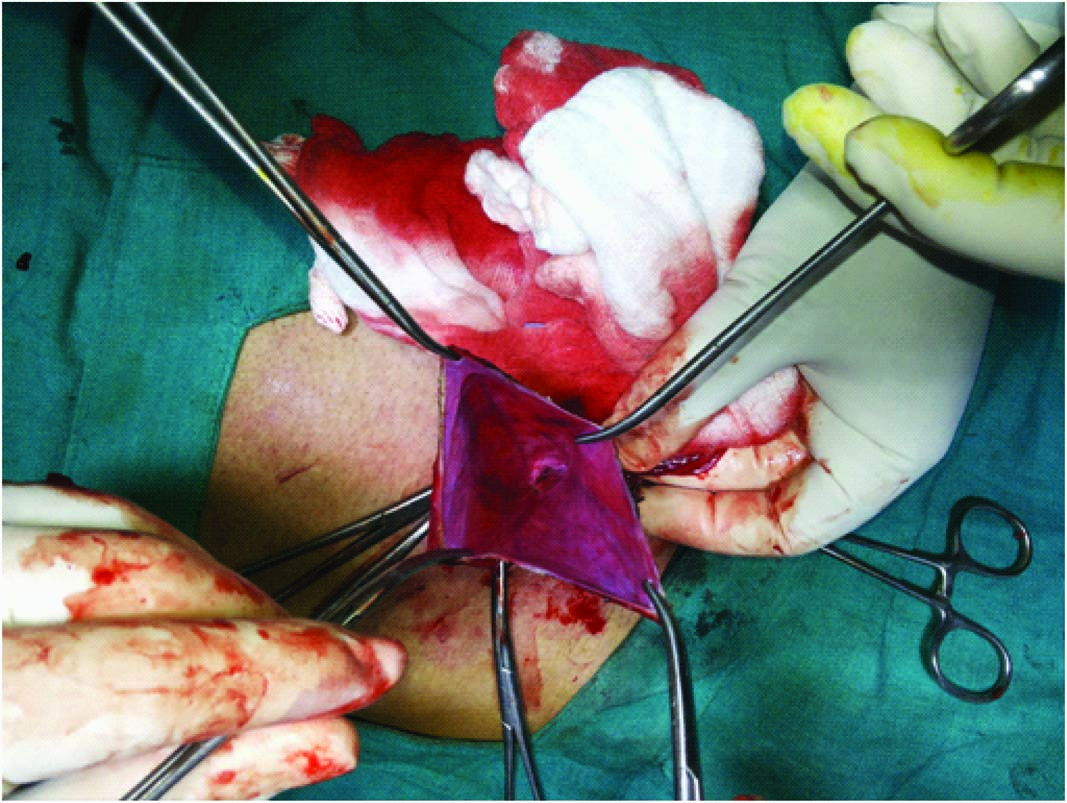
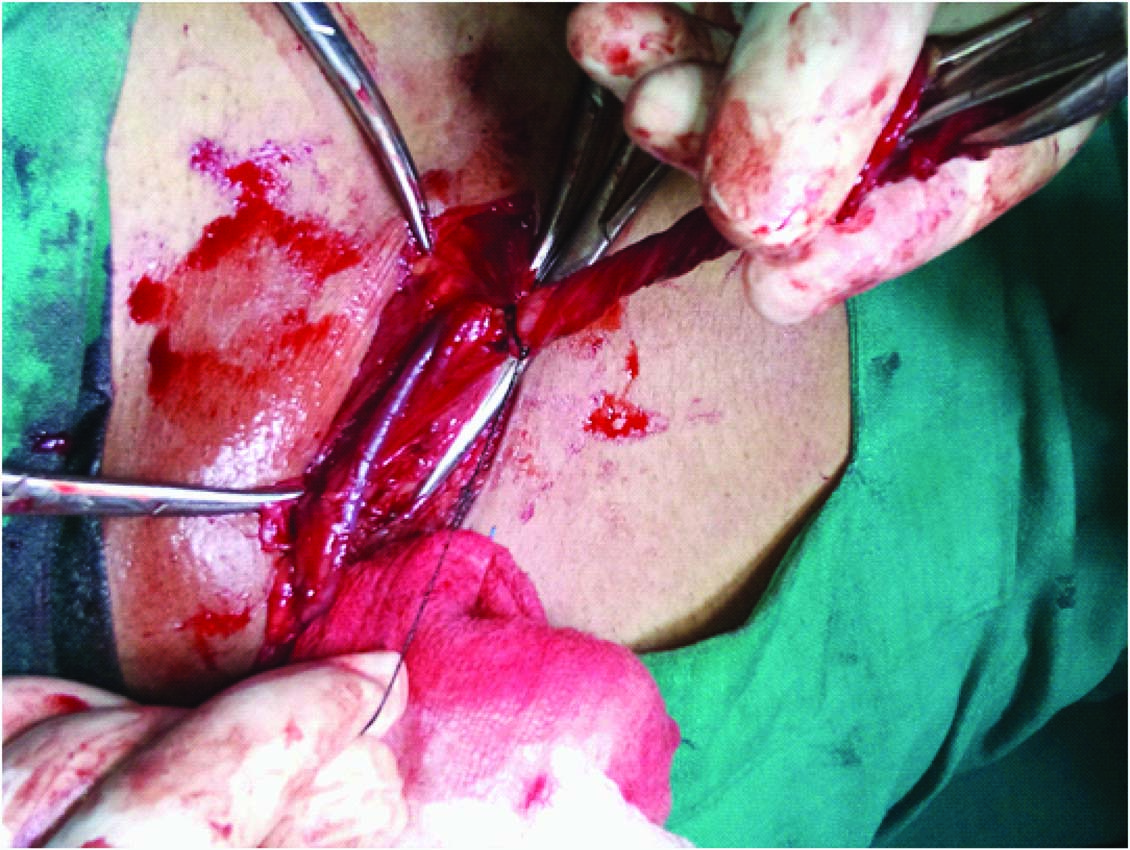
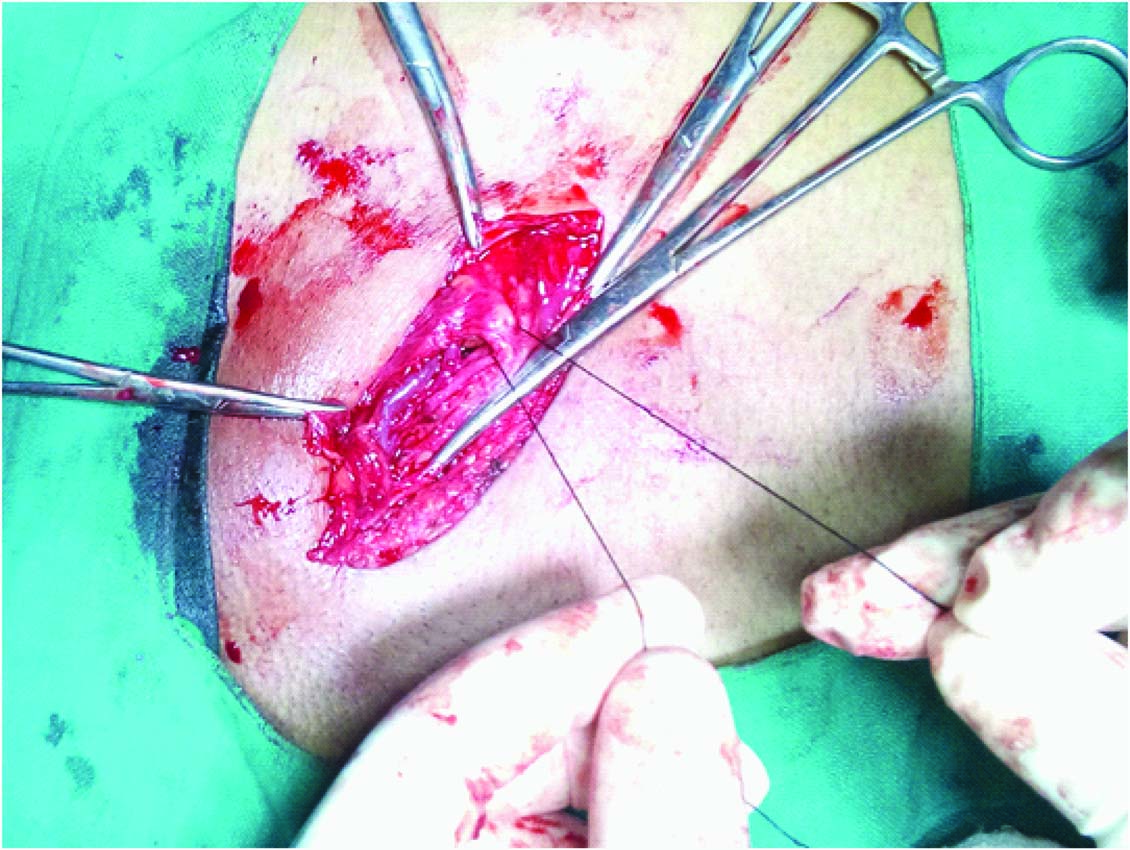
The inguinal hernia repair was performed using following steps: Under complete aseptic precautions parts cleaned, painted and draped, Skin Incision taken at 2cm above and parallel to inguinal ligament extending from superficial to deep inguinal ring [Table/Fig-1]. External oblique aponeurosis is exposed [Table/Fig-2] and incisised along the line of skin incision extending medially till superficial inguinal ring, superomedial flap is separated from conjoint tendon and Inferolateral flap is dissected upto upturn part of inguinal ligament. Then, Cord structures are hooked and sac is separated [Table/Fig-3]. Then, Sac is opened, Contents are reduced, [Table/Fig-4] then Sac is twisted, transfixed, ligated with Vicryl No. 2 round body needle [Table/Fig-5] and excised. Then, the stump of sac is fixed to the muscles forming the deep inguinal ring that is Internal Oblique and Transverse Abdominis Muscle [Table/Fig-6]. Then, Cord sructures are lateralised and Posterior wall repair is done starting from pubic tubercle to deep ring taking continuous interlocking sutures using prolene 2/0 round body needle [Table/Fig-7]. Prolene Mesh is kept and fixed to the posterior wall of inguinal canal, that is fixed medially to the periosteum of pubic tubercle, inferiorily to the inguinal ligament, superomedially to the conjoint tendon and laterally it is fixed to the internal oblique muscle and beyond the deep inguinal ring medially, engulfing the cord structures and is sutured proximal to the deep inguinal ring with prolene 2/0 round body needle. [Table/Fig-8] Then, Cord structures are reposited, external oblique aponeurosis is sutured by taking continuous interlocking suture starting from beyond the angle of external oblique muscle incison laterally and superficial inguinal ring medially [Table/Fig-9] using prolene 1/0 round body needle and finally the skin is sutured with ethylon 3/0.
Skin Incision taken at 2cm above and parallel to inguinal ligament extending from superficial to deep inguinal ring

External aponeurosis is exposed and incised
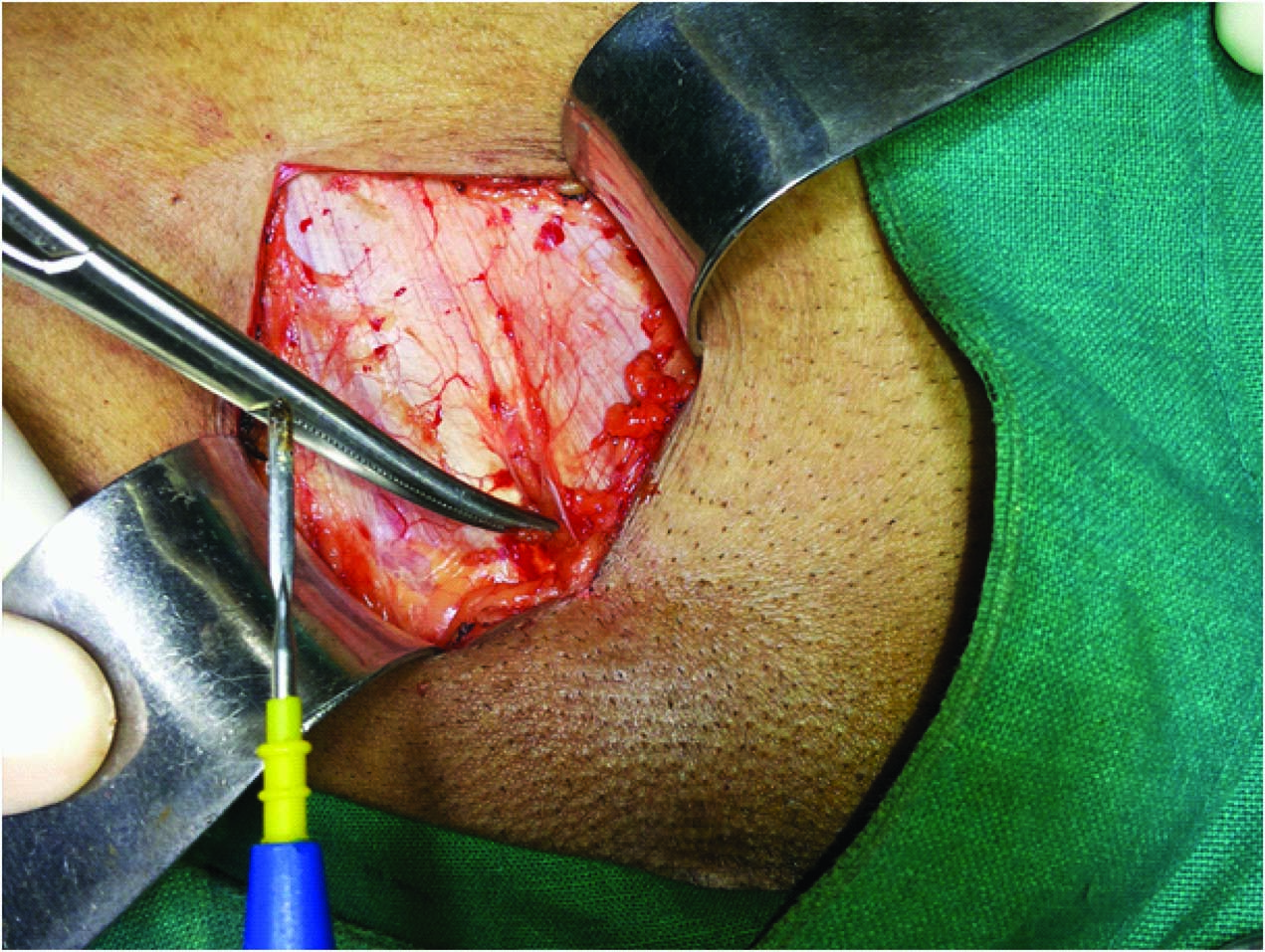
Cord structures are hooked and sac is separated
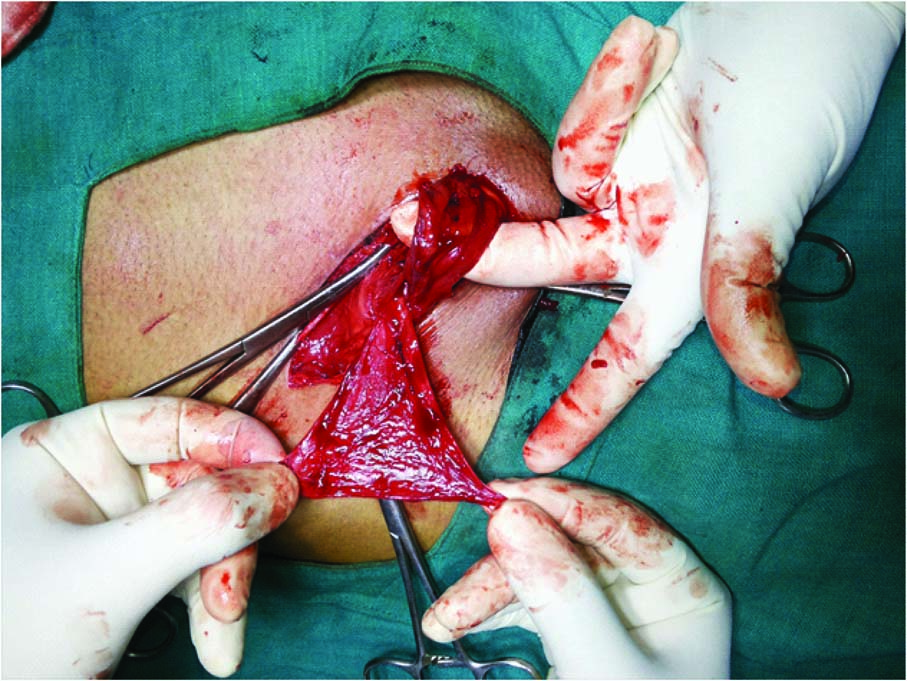
Sac is opened and contents are reduced
Sac transfixed and ligated
The stump of sac is fixed to the muscles forming the deep inguinal ring that is internal oblique and transverse abdominis muscle
Cord sructures are lateralised and posterior wall repair is done starting from pubic tubercle to deep ring taking continuous interlocking sutures

Mesh is fixed to posterior wall and cord structure reposited

External oblique aponeurosis sutured

Duration of Surgery
In the beginning author took around 45-48 min for unilateral indirect inguinal hernia repair, while 38-40 min for unilateral direct hernia by this technique. After completing around 100 surgeries it took around 30-32 min for indirect while 25-27 min for direct hernia; after 475 surgeries author is completing indirect hernia repair in 16-18 min and direct hernia in 12-13 min from skin incision to skin suture.
Follow-up of Study Participants
After their discharge, patients were asked for follow up after a period of 6-12 mnth, for routine assessments and investigations. Four patients out of 479 skipped the follow-up and therefore were excluded from the study.
Stastical Analysis
It was carried out by using mean, standard deviation (SD), incidence rate and percentage.
Results
A total of 475 patients were enrolled in the study, the characteristics of study participants and Inguinal hernia are described in [Table/Fig-10] and [Table/Fig-11] respectively. After their repair, post operative complications were noted on their follow-up. The characteristics and incidences of post-operative complications are mentioned in [Table/Fig-12] and [Table/Fig-13].
Characteristics of study participants (n=475)
| Age (in years) | Male (%) | Female (%) | Over all (%) |
|---|
| 20-30 | 137 (28.84%) | 0 (0%) | 137 (28.84%) |
| 30-40 | 151 (31.79%) | 2 (0.01%) | 153 (32.21%) |
| 40-50 | 78 (16.42%) | 1 (0.01%) | 79 (16.63%) |
| >50 | 99 (20.84%) | 5 (0.01%) | 104 (21.89%) |
| Over all | 467 (98.32%) | 8 (0.02%) | 475 (100%) |
| Mean Age at Surgery (in years) | | | 42.8 ± 14.3 |
| Diabetics | 52 (11.1%) | 1 (12.5%) | 53 (11.16%) |
| Smokers | 84 (17.9%) | 1 (12.5%) | 85 (17.89%) |
| Body Mass Index (kg/m2) | Number (Percentage) |
| <18.5 | 189 (39.79%) |
| 18.5 – 22.9 | 214 (45.05%) |
| >23.0 | 72 (15.16%) |
| Overall (Mean ± Standard Deviation) | 19.8 ± 4.6 |
| ASA Grade (American Society of Anesthesiologists) |
| ASA I | 290 (61.05%) |
| ASA II | 178 (34.47%) |
| ASA III | 6 (0.01%) |
| ASA IV | 1 (<0.01%) |
Characteristic of inguinal hernia in study participants (n=475)
| Characteristic | Study Participants (Percentage) |
|---|
| Side of Inguinal Hernia |
| Right | 217 (45.68%) |
| Left | 189 (39.79%) |
| Bilateral | 69 (14.53%) |
| Type of Unilateral Hernia (n=406) |
| Direct | 122 (30.04%) |
| Indirect | 256 (63.05%) |
| Pantaloon | 28 (6.89%) |
| Episode |
| Primary | 427 (89.89%) |
| Recurrent | 48 (10.11%) |
| Presentation |
| Swelling | 338 (71.16%) |
| Swelling, pain | 97 (20.42%) |
| Swelling, pain, incarceration | 34 (7.16%) |
| Sweling, pain, strangulation | 6 (1.26%) |
Late post operative complications of study participants
| Late Post-Operative Complication | Direct Inguinal Hernia | Indirect Inguinal Hernia | Pantaloon Inguinal Hernia | Over all |
|---|
| Recurrence | 1 (16.67%) | 0 (0%) | 0 (0%) | 1 (16.67%) |
| Sinuses | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Painful Scar | 1 (16.67%) | 3 (50%) | 1 (16.67%) | 5 (83.33%) |
| Atrophy of Testis | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Over all | 2 (33.33%) | 3 (50%) | 1 (16.67%) | 6 (0.01%) |
Early post operative complications of study participants
| Early Post Operative Complication | Direct Inguinal Hernia | Indirect Inguinal Hernia | Pantaloon Inguinal Hernia | Over all |
|---|
| Retention of Urine | 4 (57.14%) | 1 (14.28%) | 1 (14.28%) | 6 (85.71%) |
| Haematoma | 0 (0%) | 0 (0%) | 1 (14.28%) | 1 (14.28%) |
| Infection | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Over all | 4 (57.14%) | 1 (14.28%) | 2 (28.56) | (0.01%) |
Discussion
Although, along time many types of surgical procedures have been tried to treat inguinal hernia, the high number of recurrences couldn’t be avoided. There is no consensus regarding the “best” surgical treatment of hernia. Based on medical publications [9–12] we have witnessed that recurrence persists with or without the use of meshes. The recurrence rate of inguinal hernia following primary repair has been reported to be 0.5%–10.0% [13–16]. The reported rates of chronic pain (0.7%–62.9%) [17–19], wound infection (1.0%– 7.0%), [20] urinary retention (0.2%–22.2%) [21,22], hypoesthesia (4.3%–67.0%) [23,24] and other postoperative complications after hernia repair also extend over wide ranges. Such wide variations in incidences may be attributed to differences in patient factors (e.g. gender, age, comorbidities and the subjective perception of symptoms) and institutional factors (e.g. surgeon’s experience, method of repair, type of anaesthesia and duration of follow-up). Thus, choice of repair method for inguinal hernia remains controversial.
Nowadays, mesh repair of inguinal hernia is the most common operation. Approximately 20 million groin hernioplasties are performed each year worldwide, over 17,000 operations in Sweden, over 12,000 in Finland, over 80,000 in England and over 8,00,000 in the USA [25–29]. Countless studies have been reported in the medical literature in attempts to improve the overall out- comes following hernia operations and, due to this fact, the procedure has evolved immensely, especially over the last few decades. Recurrence of inguinal hernia was initially a significant problem; however with the advent of the tension-free mesh repair as described as Lichtenstein Repair (LR) [30], recurrence rate has consistently been reported as low as 1–4% [31–34], a drop from up to 50–60%.
The postoperative complications with LR + Herniorrhaphy [Table/Fig 14] in the study subjects approximate to 0.02% (n=13), that is very less. Of that retention of urine was found in 0.01% (n=6) cases, painful scar in 0.01% (n=5) cases, hematoma in <0.01% (n=1) cases and recurrence was also found in <0.01% (n=1) cases. While 0% cases were reported for sinuses, mesh migration, infection and atrophy of testis in the study participants.
Comparison of outcome of different techniques used for open hernia repair
| Studies | Techniques | Recurrence | Painful Scar | Sinus | Atrophy of Testis | Retention Urine | Haematoma | Infection |
|---|
| Current Study | LR+ HR | 1/475 | 5/475 | 0/475 | 0/475 | 6/475 | 1/475 | 0/475 |
| 2014, Kai Xiong Cheong [35] | LR | 20/520 | 6/520 | 0/520 | 0/520 | 7/520 | 25/520 | 3/520 |
| 2012, Berrevoet et al., [36] | TIPP | 3/72 | - | - | - | - | - | - |
| LR | 2/70 | - | - | - | - | - | - |
| 2006, Dogru et al., [37] | TIPP | 0/69 | - | - | - | - | - | - |
| LR | 1/70 | - | - | - | - | - | - |
| 2007, Gunal et al., [38] | TIPP | 1/39 | - | - | - | - | - | - |
| LR | 1/42 | - | - | - | - | - | - |
| 2007, Nienhuijs et al., [39] | TIPP | 2/86 | - | - | - | - | - | - |
| LR | 2/85 | - | - | - | - | - | - |
| 2004, Muldoon et al., [40] | TIPP | 1/121 | - | - | - | - | - | - |
| LR | 5/126 | - | - | - | - | - | - |
| 2012, Koning et al., [41] | TIPP | 2/143 | - | - | - | - | - | - |
| LR | 4/159 | - | - | - | - | - | - |
| 1999, Kawji et al., [42] | TIPP | 0/21 | - | - | - | - | - | - |
| LR | 0/83 | - | - | - | - | - | - |
| 2008, Karatepe et al., [43] | TIPP | 0/19 | - | - | - | - | - | - |
| LR | 0/21 | - | - | - | - | - | - |
| 2010, Hamza et al., [44] | TIPP | 0/25 | - | - | - | - | - | - |
| LR | 0/25 | - | - | - | - | - | - |
| 2008, Erhan et al. [45] | TIPP | 1/24 | - | - | - | - | - | - |
| LR | 0/70 | - | - | - | - | - | - |
| 2007, Farooq et al., [46] | TIPP | 0/33 | - | - | - | - | - | - |
| LR | 0/34 | - | - | - | - | - | - |
| 2013, Paulo Kasab et al., [47] | MV | 2/75 | - | - | - | - | - | - |
| BT | 2/69 | - | - | - | - | - | - |
| 2013, L. Timisescu et al., [48] | LR | 1/91 | 0/91 | 0/91 | 0/91 | 4/91 | 9/91 | 5/91 |
| 2001, George H Sakorafas et al., [49] | LR | 1/540 | - | - | - | - | - | - |
| 2011, Anuradha Anand et al., [50] | LR | 4/489 | 11/489 | - | 2/489 | - | - | 1/489 |
| PHS | 0/190 | 2/190 | - | 3/190 | - | - | 1/190 |
| DR | 1/88 | 4/88 | - | 1/88 | - | - | 0/88 |
| MP | 1/50 | 1/50 | - | 0/50 | - | - | 0/50 |
| HT | 2/9 | 0/9 | - | 0/9 | - | - | 0/9 |
| 2012, G. G. Koning et al., [51] | TREPP | 0/50 | - | - | - | - | 18/50 | 0/50 |
| 2013, Motohito Nakagawa et al., [52] | MR | 0/46 | 30/46 | - | - | - | 2/46 | - |
| PHS | 0/45 | 31/45 | - | - | - | 1/45 | - |
| 2011, Konrad Pielacinski et al., [53] | LR | 2/59 | - | - | - | - | 6/59 | - |
Abberation: HR: Herniorrhaphy, TIPP: Open Transinguinal Pre-peritoneal Mesh Repair, LR: Lichtenstein Repair, MV: McVay Technique, BT: Bassini Technique, DR: Darn Repair, MP: Mesh Plug, PHS: Prolene Hernia System, HT: Herniotomy, TREPP: Transrectus sheath peritoneal technique, MR: Marcy Repair
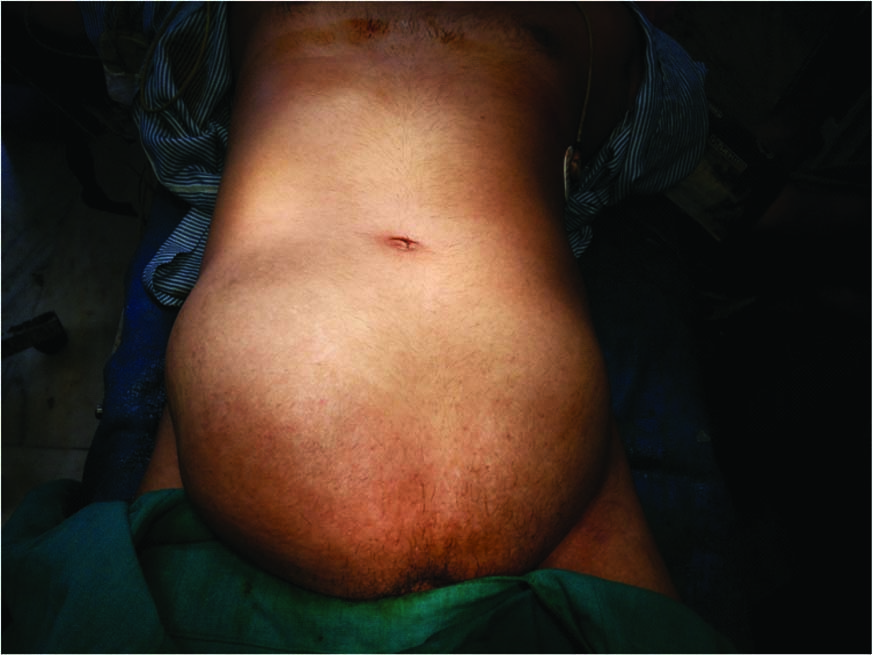
There were two unusual cases encountered in the study, one in which there was bilateral huge direct inguinal hernia with the defect more than 7cm on both the sides [Table/Fig-15] and in second case complete indirect hernia with congenital sac containing appendix [Table/Fig-16]. In both the cases repair was done by this technique, with no postoperative complications.
Preoperative picture shows huge bilateral inguinal hernia.
Intra-operative picture shows appendix in hernia sac (Amyand’s Hernia)

[Table/Fig-17] suggests that LR with Herniorrhaphy is better than LR alone in terms of low recurrence rate and low incidences of post operative complications. Study noted similar recurrence rate as that of TREPP, MR and PHS but those techniques have high incidences of other postoperative complications like atrophy of testis, hematoma and painful scar which limits the use of the same in routine practice.
Comparison of recurrence and postoperative complications with various techniques
| Technique | Recurrence | Atrophy Testis | Retention | Painful Scar | Hematoma |
|---|
| Current Study | <0.01% | 0% | 0.01% | 0.01% | 0.01% |
| LR [35–50, 53] | 1.73% | 1% | 1.8% | 1.5% | 5.97% |
| TIPP [36–46] | 1.83% | - | - | - | - |
| MV [47] | 2.67% | - | - | - | - |
| BT [47] | 2.89% | - | - | - | - |
| DR [50] | 1.14% | 4.54% | - | 4.54% | - |
| MP [50] | 2% | 2% | - | 2% | - |
| TREPP [51] | 0% | - | - | - | 36% |
| MR [52] | 0% | 65.2% | - | 65.2% | 4.35% |
| PHS [50,52] | 0% | 14.04% | - | 68.8% | 2.22% |
Conclusion
LR with Herniorrhaphy can be used for open inguinal hernia repair as the gold standard procedure as it has got very low recurrence rate (<0.01%) and other postoperative complications like Retention of urine, Painful scar, Hematoma and Atrophy of testis as compared to other techniques. However, the result of this study is based on the data from a single center, thus we recommend multicentric trials to test the efficacy of this technique.
Abberation: HR: Herniorrhaphy, TIPP: Open Transinguinal Pre-peritoneal Mesh Repair, LR: Lichtenstein Repair, MV: McVay Technique, BT: Bassini Technique, DR: Darn Repair, MP: Mesh Plug, PHS: Prolene Hernia System, HT: Herniotomy, TREPP: Transrectus sheath peritoneal technique, MR: Marcy Repair
[1]. Rutkow IM, Epidemiologic, economic, and sociologic aspects of hernia surgery in the United States in the 1990sSurg Clin North Am 1998 78(6):941-51.:v-vi. [Google Scholar]
[2]. Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, European Hernia Society guide- lines on the treatment of inguinal hernia in adult patientsHernia 2009 13(4):343-403.doi: 10.1007/s10029-009-0529-7. Epub 2009 Jul 28 [Google Scholar]
[3]. Primatesta P, Goldacre MJ, Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortalityInt J Epidemiol 1996 25(4):835-39. [Google Scholar]
[4]. Kingsnorth AN, Mr G, Nott DM, Prospective randomised trial comparing the shouldice technique and placation darn for inguinal herniaBr J Surg 1992 79:1068-70. [Google Scholar]
[5]. Panos RG, Beck DE, Maresh JE, Hardford FJ, Preliminary results of a perspective randomised study of Cooper’s ligament versus shouldice hernioplasty techniqueSurg Gynecol Obstet 1992 175:315-19. [Google Scholar]
[6]. Beetls GL, Oosterhius KJ, PM GO, Baetin CG, Kootstra G, Long term follow up (12–15 years) of a randomized controlled trial comparing Bassini—Stellen, shouldice and high ligation with narrowing of the internal ring for primary inguinal hernia repairJ Am Coll Surg 1977 185:352-57. [Google Scholar]
[7]. Scott NW, McCormack K, Graham P, Go PMNYH, Ross SJ, Grant AM, Open mesh versus non-mesh repair of inguinal herniaCochrane Database Syst Rev 2002 4:CD 002197 [Google Scholar]
[8]. EU Hernia Trialist Collaboration Mesh compared with non-mesh methods of open groin hernia repair: systematic review of randomised controlled trialsBr J Surg 2000 87:854-59. [Google Scholar]
[9]. Maggiore D, Müller G, Hafanaki J, Bassini vs Lichtenstein: two basic techniques for inguinal hernia treatmentHernia 2001 5(1):21-24. [Google Scholar]
[10]. Aroori S, Spence RA, Chronic pain after hernia surgery--An Informed Consent IssueUlster Med J 2007 76(3):136-40. [Google Scholar]
[11]. Staal E, Nienhuijs SW, Keemers-Gels ME, Keemers-Gels ME, Rosman C, Strobbe LJ, The impact of pain on daily activities following open mesh inguinal hernia repairHernia 2008 12(2):153-57. [Google Scholar]
[12]. Shin D, Lipshultz LI, Goldstein M, Barmé GA, Fuchs EF, Nagler HM, Herniorrhaphy with polypropylene mesh causing inguinal vasal obstruction: a preventable cause of obstructive azoospermiaAnn Surg 2005 241(4):553-58. [Google Scholar]
[13]. Bay-Nielsen M, Kehlet H, Strand L, Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide studyLancet 2001 358:1124-28. [Google Scholar]
[14]. Flum DR, Horvath K, Koepsell T, Have outcomes of incisional hernia repair improved with time? A population-based analysisAnn Surg 2003 237:129-35. [Google Scholar]
[15]. Jansen PL, Klinge U, Jansen M, Junge K, Risk factors for early recurrence after inguinal hernia repairBMC Surg 2009 9:18 [Google Scholar]
[16]. Butters M, Redecke J, Köninger J, Long-term results of a randomized clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal hernia repairsBr J Surg 2007 94:562-65. [Google Scholar]
[17]. Kingsnorth AN, Bowley DM, Porter C, A prospective study of 1000hernias: results of the Plymouth Hernia ServiceAnn R Coll Surg Engl 2003 85:18-22. [Google Scholar]
[18]. The MRC Laparoscopic Groin Hernia Trial GroupLaparoscopic versus open repair of groin hernia: a randomised comparisonLancet 1999 354:185-90. [Google Scholar]
[19]. Cunningham J, Temple WJ, Mitchell P, Cooperative hernia study. Pain in the postrepair patientAnn Surg 1996 224:598-602. [Google Scholar]
[20]. Jenkins JT, Dwyer O PJ, Inguinal herniasBMJ 2008 336:269-72. [Google Scholar]
[21]. Finley RK Jr, Miller SF, Jones LM, Elimination of urinary retention following inguinal herniorrhaphyAm Surg 1991 57:486-88. [Google Scholar]
[22]. Koch CA, Grinberg GG, Farley DR, Incidence and risk factors for urinary retention after endoscopic hernia repairAm J Surg 2006 191:381-85. [Google Scholar]
[23]. Beldi G, Haupt N, Ipaktchi R, Wagner M, Candinas D, Postoperative hypoesthesia and pain: qualitative assessment after open and laparoscopic inguinal hernia repairSurg Endosc 2008 22:129-33. [Google Scholar]
[24]. Forte A, D’Urso A, Gallinaro LS, [Complications of inguinal hernia repair]G Chir 2002 23:88-92.Italian [Google Scholar]
[25]. Heikkinen TJ, Haukipuro K, Hulkko A, A cost and outcome comparison between laparoscopic and Lichtenstein hernia opera- tions in a day-case unit. A randomized prospective studySurg Endosc 1998 12:1199-203. [Google Scholar]
[26]. Cheek CM, Black NA, Devlin HB, Groin hernia surgery: a sys- tematic reviewAnn R Coll Surg Engl 1998 80(1):S1-80. [Google Scholar]
[27]. Rutkow IM, Demographic and socioeconomic aspects of hernia repair in the United States in 2003Surg Clin North Am 2003 83:1045-51. [Google Scholar]
[28]. Swedish Hernia Register. http://www.svensktbrackregister.se (10 June 2007, date last accessed) [Google Scholar]
[29]. Amid PK, Lichtenstein tension-free hernioplasty: its inception, evolution and principlesHernia 2004 8:1-7. [Google Scholar]
[30]. Heikkinen T, Bringman S, Ohtonen P, Five-year outcome of laparoscopic and Lichtenstein hernioplastiesSurg Endosc 2004 18:518-22. [Google Scholar]
[31]. Lepere M, Benchetrit S, Debaert M, A multicentric comparison of transabdominal versus totally extraperitoneal laparoscopic hernia repair using PARIETEX meshesJ Soc Laparoendosc Surg 2000 4:147-53. [Google Scholar]
[32]. Olmi S, Erba L, Magnone S, Prospective study of laparoscopic treatment of incisional hernia by means of the use of composite mesh: indications, complications, mesh fixation materials and re- sults (in Italian)Chir Ital 2005 57:709-16. [Google Scholar]
[33]. MacFadyen BV Jr, Mathis CR, Inguinal herniorrhaphy: complications and recurrencesSemin Laparosc Surg 1994 1:128-40. [Google Scholar]
[34]. McCormack K, Scott NW, Go PM, Laparoscopic techniques versus open techniques for inguinal hernia repairCochrane Database 2003 1:CD001785 [Google Scholar]
[35]. Kai Xiong Cheong, Hong Yee Lo, Jun Xiang Andy Neo, Appasamy Vijayan, Chi Ming Terk, Inguinal hernia repair: are the results from a general hospital comparable to those from dedicated herniacentres?Singapore Med J 2014 55(4):191-17. [Google Scholar]
[36]. Berrevoet F, NCT00323673-unpublished data. Data for combined analysis was taken from the published Cochrane review cited as Willaert W, De Bacquer D, Rogiers X, Troisi R, Berrevoet F. Open Preperitoneal Techniques versus Lichtenstein Repair for elective Inguinal HerniasCochrane Database Syst Rev 2012 7:CD008034 [Google Scholar]
[37]. Dogru O, Girgin M, Bulbuller N, Comparison of Kugel and Lichtenstein operations for inguinal hernia repair: results of a pro- spective randomized studyWorld J Surg 2006 30:346-50. [Google Scholar]
[38]. Gunal O, Ozer S, Gurleyik E, Does the approach to the groin make a difference in hernia repair?Hernia 2007 11:429-34. [Google Scholar]
[39]. Nienhuijs S, Staal E, Keemers-Gels M, Pain after open preper- itoneal repair vs Lichtenstein repair: a randomized trialWorld J Surg 2007 31:1751-57. [Google Scholar]
[40]. Muldoon RL, Marchant K, Johnson DD, Lichtenstein vs anterior preperitoneal prosthetic mesh placement in open inguinal hernia repair: a prospective, randomized trialHernia 2004 8:98-103. [Google Scholar]
[41]. Koning GG, Keus F, Koeslag L, Randomized clinical trial of chronic pain after the transinguinal preperitoneal technique com- pared with Lichtenstein’s method for inguinal hernia repairBr J Surg 2012 99:1365-73. [Google Scholar]
[42]. Kawji R, Feichter A, Fuchsjager N, Postoperative pain and return to activity after five different types of inguinal herniarrha- phyHernia 1999 3:31-35. [Google Scholar]
[43]. Karatepe O, Adas G, Battal M, The comparison of preperito- neal and Lichtenstein repair for incarcerated groin hernias: a ran- domised controlled trialInt J Surg 2008 6:189-92. [Google Scholar]
[44]. Hamza Y, Gabr E, Hammadi H, Four-arm randomized trial comparing laparoscopic and open hernia repairsInt J Surg 2010 8:25-28. [Google Scholar]
[45]. Erhan Y, Erhan E, Aydede H, Chronic pain after Lichtenstein and preperitoneal (posterior) hernia repairCan J Surg 2008 51:383-87. [Google Scholar]
[46]. Farooq O, Batool Z, Din AU, Anterior tension - free repair versus posterior preperitoneal repair for recurrent herniaJ Coll Physicians Surg Pak 2007 17:465-68. [Google Scholar]
[47]. Paulo Kassab, Ettore Ferrari Franciulli, Carolina Kassab Wroclawski, Elias Jirjoss Ilias, Osvaldo Antônio Prado Castro, Carlos Alberto Malheiros, Meshless treatment of open inguinal hernia repair: a prospective studyEinstein 2013 11(2):186-89. [Google Scholar]
[48]. Timiæescu L, Turcu F, Munteanu R, Gîdea C, Drãghici L, Ginghinã O, Treatment of Bilateral Inguinal Hernia - Minimally Invasive versus Open Surgery ProcedureChirurgia 2013 108:56-61. [Google Scholar]
[49]. Sakorafas George H, Halikias Ioannis, Nissotakis Christos, Kotsifopoulos Nikolaos, Stavrou Alexios, Antonopoulos Constantinos, Open tension free repair of inguinal hernias; the Lichtenstein techniqueMC Surgery 2001 1:3 [Google Scholar]
[50]. Anand Anuradha, Sinha Prem A, Kittappa Karthik, Mulchandani Manoj H, Debrah Samuel, Brookstein Roger, Review of Inguinal Hernia Repairs by Various Surgical Techniques in a District General Hospital in the UKndian J Surg 2011 73(1):13-18. [Google Scholar]
[51]. Koning GG, Andeweg CS, Keus F, Tilburg MW A van, Laarhoven CJ H M van, Akkersdijk WL, The transrectus sheath preperitoneal mesh repair for inguinal hernia: technique, rationale, and results of the Wrst 50 casesHernia 2012 16:295-99. [Google Scholar]
[52]. Nakagawa Motohito, Nagase Takeshi, Akatsu Tomotaka, Imai Shun, Fujimura Naoki, Asagoe Tatsuo, A randomized prospective trial comparing clinical outcomes 3 years after surgery by Marcy repair and Prolene Hernia Systemrepair for adult indirect inguinal herniaSurg Today 2013 43:1109-15. [Google Scholar]
[53]. Pielacinski Konrad, Szczepanik Andrzej B, Misiak Andrzej, Wróblewski Tadeusz, Randomized clinical trial comparing inguinal hernia repair with Lichtenstein technique using non-absorbable or partially absorbable mesh. Preliminary reportVideosurgery and Other Miniinvasive Techniques 2011 6(4):190-206. [Google Scholar]