A Comparative Study of Lateral Sphincterotomy and 2% Diltiazem Gel Local Application in the Treatment of Chronic Fissure in ANO
Giridhar C. M.1, Preethitha Babu2, K. Seshagiri Rao3
1 Ex-Resident, Department of General Surgery, Bangalore Medical College and Research Institute, Bangalore, India.
2 Resident, Department of General Surgery, Bangalore Medical College and Research Institute, Bangalore, India.
3 Professor, Department of General Surgery, Bangalore Medical College and Research Institute, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Giridhar C. M, Flat No. 004,# 30/1, Mathias Mansion, II Cross, Vivekanandanagar, Bangalore-560033, India. Phone : 9448565522, E-mail : cmgiridhar@gmail.com
Introduction: Anal fissures are commonly encountered in routine clinical practice. Anal fissure has traditionally been treated surgically. Developments in the pharmacological understanding of the internal anal sphincter have resulted in more conservative approaches towards treatment. In this study we compare symptomatic relief, healing and side effects of topical 2% Diltiazem gel and lateral internal sphincterotomy in the treatment of chronic fissure in ano.
Materials and Methods: In this prospective trial, 60 surgical out patients and/or admitted patients with chronic fissure in ano were randomly divided into Group 1 (Diltiazem gel) and Group 2 (internal sphincterotomy) with 30 patients in each Group. Patients were followed up at weekly intervals for six consecutive weeks and biweekly for subsequent 3 months.
Results: Fissure was completely healed in 88.46% of patients in Group 1 and in 100% in Group 2. The mean duration required for healing of fissure was 5.04 weeks in Group 1 and 3.6 weeks in Group 2. 78.26% patients were free from pain in Group 1 whereas 85.18% patients were free from pain in Group 2. No patient had any side effects in either group.
Conclusion: Topical Diltiazem should be considered as first line treatment in chronic fissure in ano. Internal sphincterotomy should be reserved for patients with relapse and therapeutic failure to prior pharmacological treatment.
Anal fissure, Chemical sphincterotomy, Surgical sphincterotomy
Introduction
Anal fissures are considered one of the commonest causes of severe anal pain. An anal fissure is a longitudinal tear or ulcer in the distal anal canal. It is usually located in the posterior or anterior midline and extends from the level of dentate line to the anal verge. Acute fissure is one which presents within 3-6 weeks of symptom onset. It has the appearance of a clean longitudinal tear in the anoderm with little surrounding inflammation. Acute fissure usually heals spontaneously within 6 weeks. A chronic fissure, with more than 6 weeks of symptoms, is usually deeper and generally has exposed internal sphincter fibers in its base. It is frequently associated with a hypertrophic anal papilla at its upper aspect and sentinel pile at its distal aspect. Based on etiology it is classified as primary (idiopathic) or secondary. Secondary fissures are those that occur due to some other pathology such as Crohn’s disease, anal tuberculosis, AIDS. Patients usually present with pain during defecation and passage of bright red blood per anus. The precise etiology of anal fissure is unknown. Fissure is most commonly attributed to trauma from the passage of a large hard stool, but it is also seen after acute episodes of diarrhea. Painful fissures are generally associated with involuntary spasm of the internal sphincter with high resting pressure in the anal canal. So it seems that chronic over activity of the internal sphincter may be the cause. Reduction of anal sphincter spasm results in improved blood supply and healing of fissure. Surgical techniques like manual anal dilatation or lateral internal sphincterotomy, effectively heal most fissures within a few weeks [1,2], but may result in permanently impaired anal continence. This has led to the research for alternative non-surgical treatment, and various pharmacological agents such as nitrates (glyceryl trinitrate, isosobide dinitrate), calcium channel blockers (nifedepine, diltiazem) have been shown to lower resting anal pressure and heal fissures without threatening anal continence [3]. The present study compares the effectiveness and side effects of 2% Diltiazem gel local application and internal sphincterotomy in the treatment of chronic fissure in ano.
Materials and Methods
This prospective, comparative study was undertaken at Bowring and Lady Curzon Hospitals attached to Bangalore Medical College and Research Institute, Bangalore, India, from September 2009 to September 2011. Sixty patients with symptoms of fissure in ano for more than 6 weeks were labeled as having chronic fissure in ano and were enrolled in this study after obtaining an informed written consent. Ethical approval was obtained from the local ethical committee. Inclusion criteria included patients between 20 to 60 years of age of both sexes. Exclusion criteria included children and mentally handicapped patients, recurrent fissures, fissures with hemorrhoids and fistula, fissures associated with malignancies, fissures secondary to specific diseases like Tuberculosis, Crohn’s disease etc., and pregnant women. Patients in Group 1 were advised to apply 1.5 to 2 cms length of gel twice daily at least 1.5 cm into the anus for 6 consecutive weeks. Patients were instructed to wash hands before and after use of gel.
Cases in Group 2 underwent left lateral internal sphincterotomy under spinal anaesthesia. Cases from both Groups were asked to take mild laxatives like cremaffin (milk of magnesia 11.25 ml, liquid paraffin 3.75 ml, per 15 ml of emulsion) three teaspoons at bedtime, high fiber diet and to use warm sitz baths. Cases were reviewed in Outpatient Department weekly for 6 consecutive weeks and biweekly for subsequent 3 months. At each visit questions were asked regarding pain relief, leakage of flatus/feces, and any side effects. Healing was assessed visually and defined as complete disappearance of fissure. Pain was assessed using a pain score chart graded from 0 (almost pain free) to IV (severe pain). The data was collected and analyzed; p-values were calculated using Chi Square test.
Results
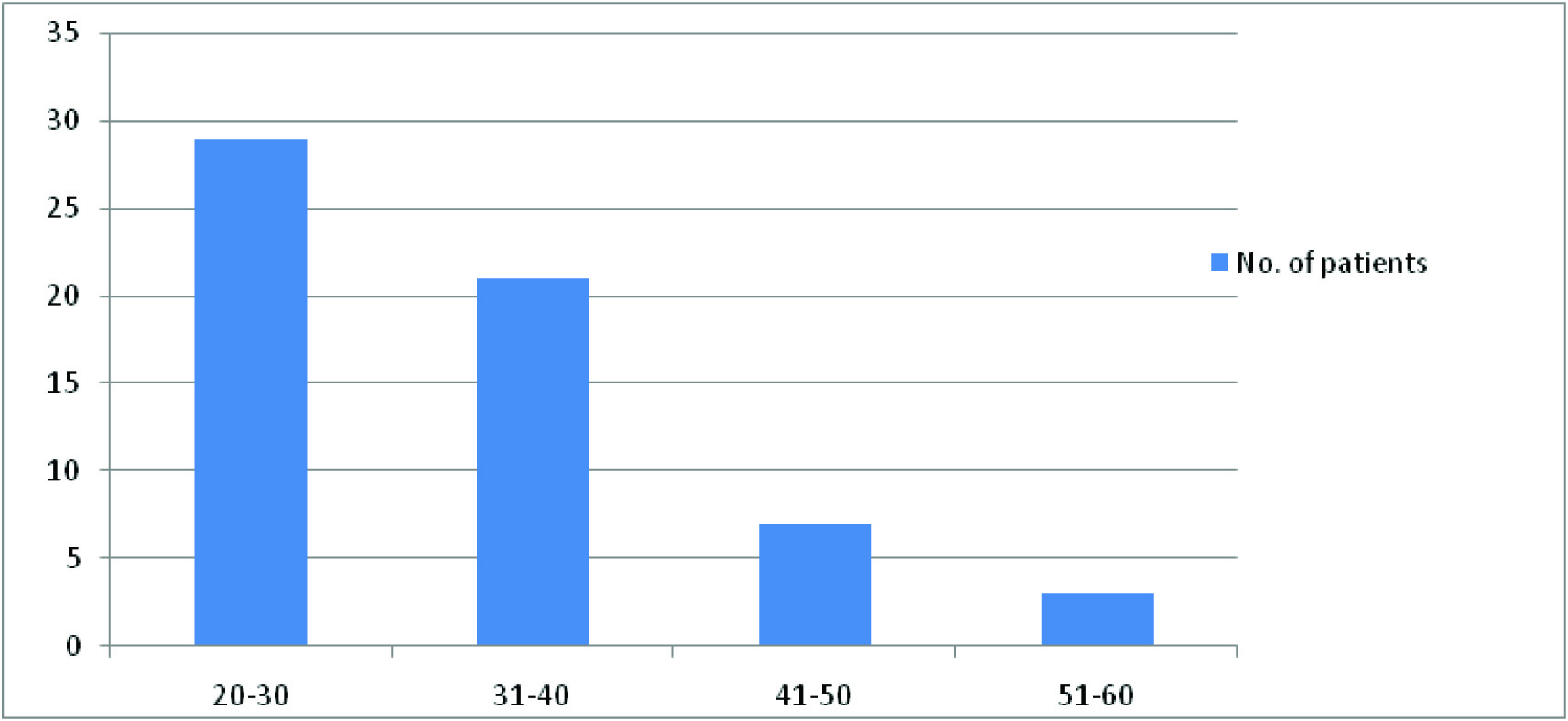
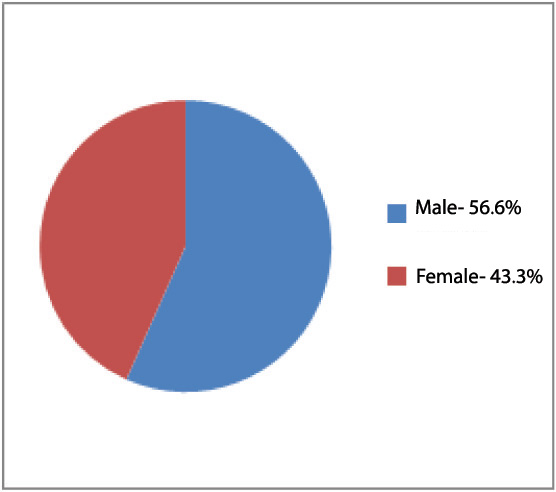
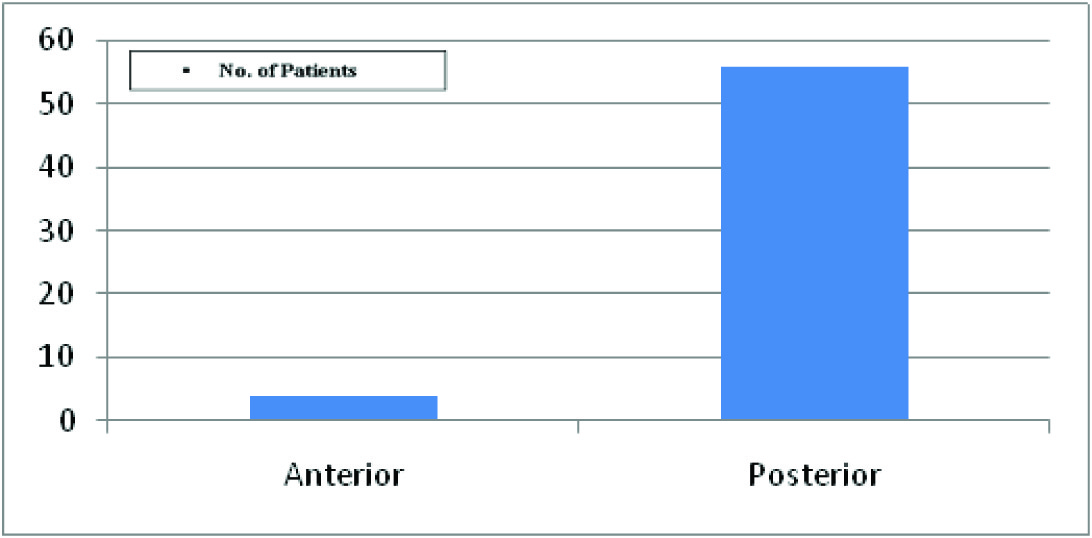
In our study most of the cases belonged to age Group 20-30 years [Table/Fig-1] with slight male preponderance [Table/Fig-2]. Majority of the fissures were posterior in location [Table/Fig-3] with sentinel pile present in 46.6% of cases. Cases were followed up at weekly intervals for 6 consecutive weeks and biweekly for subsequent 3 months. Four cases from Group 1 and 3 cases from Group 2 were lost to follow up and hence not included in statistical analysis. 88.4% of patients in Group 1 and 100% of patients in Group 2 had completely healed fissures at the end of 4 weeks [Table/Fig-4]. 78.26% of patients in Group 1 who were completely healed with Diltiazem gel application and 85.18% of patients in Group 2 were free from pain at the end of 3 months [Table/Fig-5]. Three patients in Group 1, whose fissures did not heal after 6 weeks of Diltiazem application and remained symptomatic, subsequently underwent internal sphincterotomy and fissures healed in 4 weeks after surgery. The mean duration of healing was comparatively longer in Group 1(5.04 weeks) than Group 2 (3.6 weeks). No complications were reported in either Group. Comparison between Group 1 and Group 2 did not show any difference in pain relief (p= 0.5261) or fissure healing (p= 0.0679).
| Healing | No. of patients | Percentage |
|---|
| Diltiazem | 23 | 88.46 |
| Surgery | 27 | 100 |
| Pain free | No. of patients | Percentage |
|---|
| Diltiazem | 18 | 78.26 |
| Surgery | 23 | 85.18 |
Discussion
Anal fissure is a very common problem across the world. It causes considerable morbidity and adversely affects the quality of life. Anal fissure is usually encountered in young or middle aged adults [4, 5] and is equally common in both sexes [4]. It is commonly found in the posterior position, although anterior fissure is comparatively common in females [6].
Therapy focuses on breaking the cycle of pain, spasm, and ischemia thought to be responsible for the development of fissure in ano. Operative management includes anal dilatation and lateral internal sphincterotomy. Lateral sphincterotomy is perhaps the operation of choice to perform in patients with chronic anal fissure needing surgical treatment. Postoperative management is simple and rate of healing is faster. However complication such as permanent anal incontinence is associated with the surgery.
Chemical sphincterotomy is now the first line of treatment in many centers [7–9]. Calcium channel blockers like nifedipine and diltiazem have been shown to lower resting anal pressure [10], promote fissure healing and are associated with good healing rate [7,11,12]. They are associated with side effects such as headache and perianal dermatitis [7]. Healing rates of chronic anal fissure in various studies ranged from 47%-80% [3,10,11,13], while that seen in our study is 88.46%. Side effects due to Diltiazem ranged from 0%-10% [3,10,13] in various studies while no patient developed side effect in our study. In contrast to surgery, chemical sphincterotomy with Diltiazem is reversible and therefore unlikely to have adverse effects on continence. Patients who are hypertensive, diabetic and medically unfit for surgery can be recommended treatment with Diltiazem. Though fissure healing rate is comparatively slower with Diltiazem, the trauma caused by surgery can be avoided and hospital stay is not required. Treatment works out to be very cost effective.
Conclusion
Chemical Sphincterotomy with Topical 2% Diltiazem should be advocated as the first option of treatment for chronic anal fissure. Internal sphincterotomy should be offered to patients with relapse and therapeutic failure of prior pharmacological treatment.
[1]. Scouten WR, Ischemic nature of anal fissureBritish Journal of Surgery 1996 83:63-65. [Google Scholar]
[2]. Tocchi Adriano, Mazzoni Gianluca, Miccini Michelangelo, Cassini Diletta, Bettelli Elia, Brozzetti Stefania, Total lateral sphincterotomy for anal fissureInternational Journal of Colorectal Disease 2004 19(3):245-49. [Google Scholar]
[3]. Jonas Marion, Scholefield JH, Anal fissure and chemical sphincterotomyTaylor I, Johnson CD. Recent advances in Surgery 2001 24th EditionChurchill Livingstone:115 [Google Scholar]
[4]. Goligher John, Anal Fissure, John Goligher, Surgery of the Anus, Rectum & ColonAITBS 1992 5th Edition:150 [Google Scholar]
[5]. Udwadia T.E, The prophylaxis of fissure in anoIndian Journal of Surgery 1978 40(11):560 [Google Scholar]
[6]. Boulos PB, Araujo JGC, Adequate internal sphincterotomy for chronic anal fissure: subcutaneous or open technique?British Journal of Surgery 1984 71(5):360-62. [Google Scholar]
[7]. Knight J. S, Birks M, Farouk R, Topical Diltiazem ointment in the treatment of chronic anal fissureBritish Journal of Surgery 2001 88(4):553-56. [Google Scholar]
[8]. Bhardwaj R, Parker M. C, Modern perspectives in the treatment of chronic anal fissuresAnnals of the Royal College of Surgeons of England 2007 89(5):472-78. [Google Scholar]
[9]. Haq Z, Rahman M, Chowdhury RA, Baten MA, Khatun M, Chemical sphincterotomy – first line of treatment for chronic anal fissureMymensingh Medical Journal 2005 14(1):88-90. [Google Scholar]
[10]. Carapeti E, Kamm M, Evans B, Phillips R, Topical Diltiazem and Bethanechol decrease anal sphincter pressure and heal anal fissures without side effectsDiseases of the Colon and Rectum 1999 43(10):1359-62. [Google Scholar]
[11]. Srivastava UK, Jain BK, Kumar Praveen, Saifee Yusuf, A comparison of the effects of Diltiazem and Glyceryl trinitrate ointment in the treatment of chronic anal fissure: a randomized clinical trialSurgery Today 2007 37(6):482-85. [Google Scholar]
[12]. Nash GF, Kapoor K, Saeb-Parsy K, Kunanadam T, Dawson PM, The long term results of Diltiazem treatment for anal fissureInternational Journal of Clinical Practice 2006 60(11):1411-13. [Google Scholar]
[13]. Dasgupta R, Franklin I, Pitt J, Dawson PM, Successful treatment of chronic anal fissure with Diltiazem gelColorectal Disease4:20-22. [Google Scholar]