Introduction: Acute angle closure glaucoma is rarely seen as complication of snake bite.We report three cases of bilateral acute angle closure glaucoma with capillary leak syndrome and acute renal failure secondary to hematotoxic snake bites. We are also briefly discussing the association of capillary leak syndrome and angle closure glaucoma in hematotoxic snake bite. This is the first time an association between angle closure and capillary leak syndrome following snake bite is reported.
Study type: Descriptive case series.
Materials and Methods: Records of all patients admitted to ICU with snake bite were reviewed to identify cases developing acute angle closure glaucoma. These cases with acute angle closure glaucoma are analysed in detail for systemic condition. Diagnosis, management and outcome of cases are described
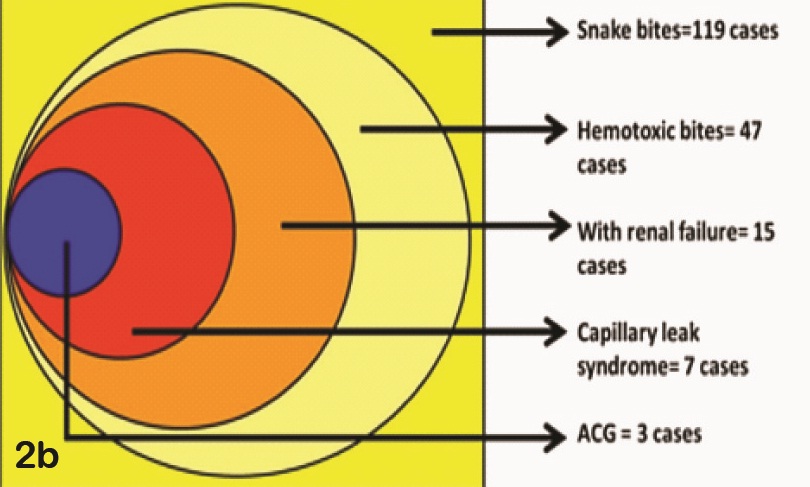
Results: Of the 119 snake bites admitted, 47 patients had confirmed hematotoxic snake bite. Fifteen of these patients underwent hemodialysis for acute renal failure. Seven of them were diagnosed to have capillary leak syndrome and all of them complained of decreased vision. Three of the 7 cases had acute angle closure glaucoma on the second day of bite. One of the patients expired and other two recovered fully, both of them had normal IOP and good vision at one month follow-up.
Conclusion: Acute angle closure glaucoma seems to be associated with systemic capillary leak syndrome in hematotoxic snake bite. High suspicion, early recognition, timely and appropriate treatment can prevent visual loss in this rare complication.
Acute angle closure glaucoma, Capillary leak syndrome, Hemofiltration, Snake bite
Introduction
Snakebite is a major public health problem worldwide. Ocular involvement in snake bite depends on whether the snake is hemotoxic or neurotoxic. Literature review shows the ophthalmic manifestations after hemotoxic snake bites can be optic neuritis [1], optic atrophy [2], uveitis [3], macular infarction [4], central retinal artery occlusion [5], vitreous haemorrhage [6] and rarely acute angle closure glaucoma [ACG] and even endophthalmitis [7]. There are only three cases of acute ACG following snake bite reported in literature [8,9]. We found cases of acute ACG also tend to develop renal failure and systemic capillary leak syndrome. The present study focuses on the patients who underwent hemofiltration after snake bite and those who had eye manifestations. We present analysis of hematotoxic snake bite patients who developed acute ACG and capillary leak together.
Materials and Methods
We did a chart review and analysis of snake bite cases admitted in our tertiary care hospital ICU in northern Kerala from May 2012 to May 2013. Charts of cases confirmed as having hematotoxicity were analysed in detail. Hematotoxic envenomation was diagnosed using the 20 min whole blood clotting test and other coagulation profiles. Patient consent was obtained whenever photographs were taken.
Haematological and biochemical analysis of blood in view of snake bite and its complications were done. Assessment of the severity of envenomation was done as described in previous study [10]. Lyophilised polyvalent enzyme refined equine immunoglobulin(Snake Venom Anti serum. I.P or ASV) was administerd depending on the severity. When necessary, appropriate referrals were done for multidisciplinary management of the patients. Patients with severe envenomation and renal involvement who required dialysis underwent Heparin free hemofiltration in the ICU itself. Ophthalmic consultation was requested whenever patient developed ocular symptoms or signs during course of management.
Bed side ophthalmological evaluation was done as the patients were not ambulant at initial consultation.Visual acuity, gross colour vision, ocular position, extraocular movements, anterior segment evaluation was done. Intra-ocular pressure was recorded using Schiotz tonometer. This was repeated twice daily till patient could be shifted to OPD. Fundus examination was done after dilating with Tropicamide eye drops 0.5% when possible, after physicians’ approval. Later, detailed evaluation was done in Ophthalmology OPD when patient was fit.
The patients with acute angle closure glaucoma were started on intravenous mannitol and topical timolol, dorzolamide eye drops after discussion with nephrologist. They were also started on prednisolone acetate 1% eye drops. The patients were reviewed twice a day till IOP returned to normal and daily thereafter till final evaluation. At each visit, all ocular findings were recorded.
The findings were tabulated in Microsoft Excel 2007 and percentage of each subgroup was derived. Average values for parameters like IOP, time required for control of IOP, final visual acuity were calculated
Results
A total of 119 cases of snake bites were admitted in the medical ICUs during the study period. Of these hemotoxicity by 20 min whole blood clotting time was confirmed in 47 cases. Fifteen of the 47 patients developed renal failure and required heparin free hemofiltration. Whole blood clot time was prolonged (>20 min) and APTT was raised in all patients. Patients without hemodialysis had no ocular symptoms and hence ophthalmological referral was not done. Eleven (73%) of the 15 patients were males. Russel’s viper (Daboia russelii; Malayalam – mandali) bite was noted in five patients, Saw-scaled viper (Echis carinatus; Malayalam – Anali) in five others and in other 5 cases snake was not identified. Reaction to ASV was not reported in any of these patients.
Of the 15 patients 10 cases had ocular symptoms. But only three patients had angle closure glaucoma and the other seven did not have any positive ocular findings. These seven patients had normal vision at recovery and were symptom free. Details of angle closure glaucoma cases are summarised in [Table/Fig-1].
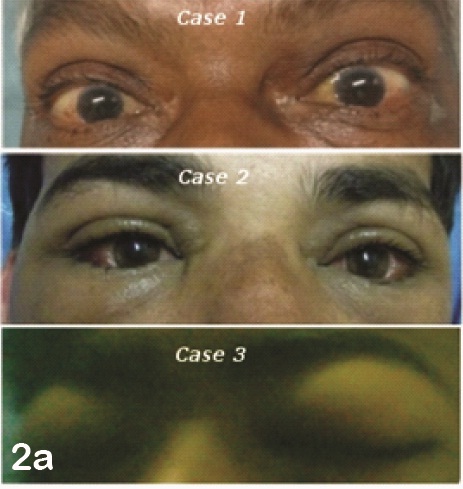
Capillary leak syndrome was diagnosed by nephrologist in seven out of 10 patients with ocular symptoms. Ocular symptoms were reported same day in one patient, on day two in three patients, and day three in another three patients. Four cases among them had facial puffiness, peri orbital oedema and lid oedema. Three of the patients with facial puffiness and periorbital oedema had very shallow anterior chamber and raised IOP [Table/Fig-2a] . Visual acuity recorded at bed side in them was less than 3/60. Two of them had mid dilated fixed pupil and one patient had 3 mm pupils but shallow anterior chamber and high IOP. The subgroups are elaborated in [Table/Fig-2b] .
IOP was lowered using hyperosmotic agents and topical anti glaucoma medications. Topical Prednisolone acetate 1% eye drops were started hourly in them along with systemic low dose Methyl Prednisolone at a dose of 125mg/ kg body weight 8th hourly due to the diagnosis of capillary leak syndrome. All of them improved with medications,IOP was controlled.Vision improved in 2 patients but the other patient expired on third day. At final review, both these patients had good vision and wide open angles on gonioscopy.
Discussion
Angle closure glaucoma (ACG) is rarely reported as complication of snake bite. We could get only two articles with total of 3 patients having this complication. All the cases reported were from south India and the snake identified was some type of Viper species. With such low incidence of complication and incomplete reporting of the snake bite it is difficult to estimate complication rate for ACG. In our case series, of the 119 cases of snake bites, 47 were confirmed hemotoxic snakes and 3 cases went for angle closure, giving a complication rate of 6.38%.
Even when snake is poisonous, systemic envenomation can vary due to various reasons [11]. The venom glands may not be full, the snake may not have injected sufficient quantity of venom, site of injection may not allow systemic entry etc. thus the varying degree of systemic envenomation itself may explain the degree of ocular involvement [12].
Envenomation rate in Kerala is about 34% in proven snake bite cases and renal failure rate is 25.5% [11]. In our series, out of 119 cases 47 had envenomation (39.5%) and 15 (12.6%) developed renal failure. Another study from western India has shown a low rate (6.6%) of hemotoxic snake bites highlighting geographical variation of snake species [13].
All three patients with angle closure had renal failure. Along with this, all the patients had capillary leak syndrome. The progression to angle closure was rapid, with all of them presenting on day 2 of snake bite. The first symptom in all of them was blurred vision. At recovery all of these patients had normal anterior chamber depth and open angles on gonioscopy. This suggests posterior mechanism of angle closure. In presence of widespread capillary leak, Ciliary body oedema resulting in anterior rotation of Ciliary processes and anterior displacement of lens iris diaphragm seems to be the most probable explanation for angle closure. It is also interesting to note that in spite of capillary leak syndrome, IOP was controlled in all patients within 24 hrs, thus ruling out excessive secretion of aqueous as cause of rise in IOP.
Another interesting thing to note is, of the 15 patients with renal failure, seven had visual symptoms and only three went for angle closure. Remaining four patients had normal ocular findings. But all of them presented with blurred vision though acuity could not be recorded in these patients, subclinical Ciliary body oedema can be cause of transient blurring of vision.
Thus, it is evident that most possible explanation of decreased vision in such cases when there is no clinical ocular involvement could be Ciliary body oedema. Ultrasound biomicroscopy would have confirmed this finding but was not feasible at our centre. When the oedema is marked, pupillary block and angle closure ensues. The oedema of Ciliary body results from capillary leak syndrome, which can be of varying severity. In our cases, all had systemic capillary leak syndrome.
The management of ACG in these cases doesn’t differ from other cases. IOP is usually controlled with conventional measures. Use of systemic steroids may have additional advantage in controlling the capillary leak syndrome reducing Ciliary body oedema. Prognosis for vision is good as seen in the two surviving cases.
All the cases of acute ACG reported are from south India. This reflects similar geographical distribution of snake species. But it can also imply that the snake venom may have affinity for Ciliary body or population in this region may be more prone to snake venom. If former is true this can be exploited to identify sites of action of the snake venom on specific vessels.
With this series of cases we conclude that at least in south India, there is a 6% risk of ACG in systemic envenomation by hemotoxic snake. The risk of angle closure increases in presence of renal failure. It reaches nearly 50% when patient has systemic capillary leak syndrome. As physicians are directly involved in care of these patients they should be made aware that a symptom of blurred vision can be first indication of imminent angle closure and hence systemic capillary leak syndrome.
Details of angle closure glaucoma cases
| Case | age/sex | Day 1 | Day 2 | Day 3 | Final Visit | Other ocular signs |
| VA | IOP | VA | IOP | VA | IOP |
| CASE 1 | 53 years male | CF 2 Meters | 50.5 | CF 3 Meters | 11.2 | Patient Died On Day 2 | pupil 4 mm, fibrinous exudates in anterior chamber, chemosis |
| CF 2 Meters | 46.9 | CF 3 Meters | 10.1 |
| CASE 2 | 36 years male | CF 1 Meter | 60 | CF 3 Meters | 25.8 | CF 6 Meters | 14.6 | 6/18 | 12.2 | pupil 6mm, chemosis, ecchymosis, corneal edema |
| CF 1 Meter | 60 | CF 3 Meters | 30.4 | CF 6 Meters | 17.3 | 6/18 | 14.6 |
| CASE 3 | 16 years male | CF 3 Meters | 25.8 | CF 3 Meters | 12.2 | CF 6 Meters | 7.1 | 6/6 | 12.2 | lid edema, pupil 6mm, chemosis, fibrinous exudates in anterior chamber |
| CF 3 Meters | 25.8 | CF 3 Meters | 7.1 | CF 6 Meters | 7.1 | 6/6 | 12.2 |
Conclusion
Acute angle closure glaucoma, though rare can be vision threatening complication of hematotoxic snake bite. The incidence of angle closure rises markedly with capillary leak syndrome and renal failure. Usually decreased vision is first symptom of such cases and has to be kept in mind by emergency room and intensive care unit staff for early recognition of this condition. Finally, if recognised early, this complication has good to excellent visual prognosis.
[1]. V Menon, R Tandon, T Sharma, A Gupta, Optic neuritis following snake bite.Indian J Ophthalmol. 1997 45:236-37. [Google Scholar]
[2]. SK Mustapha, M MubiB, BH Askira, Bilateral blindness following snakebite.Trop Doct. 2010 40:117-18. [Google Scholar]
[3]. GP Buttes, N Ayan, G Cami, Uveitis after snakebite.Arch Pediatr. 1996 3:832-33. [Google Scholar]
[4]. Singh Jatinder, Singh Preetam, Singh Rajbir, Kumar Vipin, Macular Infarction Following Viperine Snake Bite.Arch Ophthalmol. 2007 125(10):1430-31. [Google Scholar]
[5]. N Tungpakorn, Unusual visual loss after snakebite.J Venom Anim Toxinsincl Trop Dis 2010 16(3):519-23. [Google Scholar]
[6]. BM Rao, A case of bilateral vitreous haemorrhage following snake bite.Indian J Ophthalmol. 1977 25(2):1-2. [Google Scholar]
[7]. Iqbal Mustafa, Khan Bakhth Samar, Ahmad Imran, Endogenous Endophthalmitis Associated with Snake Bite.Pak J Ophthalmol 2009 25(2):114-46. [Google Scholar]
[8]. Srinivasan Renuka, Kalaiperumal Subashini, Bilateral angle closure glaucoma following snake bite.JAPI 2005 53:46-48. [Google Scholar]
[9]. Haneef Mohd, Verma Veena, Acute angle closure glaucoma: rare complication of viper bite.KMJ 2008 2:27-28. [Google Scholar]
[10]. RC Dart, KM Hurlbut, R Garcia, Validation of a severity score for the assessment of crotalid snakebites.Ann Emerg Med. 1996 27:321-26. [Google Scholar]
[11]. PV Silveira, A Nishioka S de, T Sharma, A Gupta, Venomous snake bite without clinical envenoming (‘dry-bite’). A neglected problem in Brazil. Trop Geogr Med. 1995 47(2):82-85. [Google Scholar]
[12]. N Suchithra, JM Pappachan, P Sujathan, Snakebite envenoming in Kerala, south India: clinical profile and factors involved in adverse outcomes. Emerg Med J 2008 25:200-04. [Google Scholar]
[13]. W.M, Chavan, K.D Chavan, Ocular Manifestations in Patients with Snakebite in Rural Western Maharashtra.Indian Journal of Forensic Medicine and Pathology. 2011 4(4):169-72. [Google Scholar]