Background: Intra-operative cytology is an important diagnostic tool. It has shown to play an important role especially in the diagnosis of central nervous system tumours. The study was done to assess the feasibility of squash cytology as standalone diagnostic test in setting where frozen section facility is not available.
Materials and Methods: Total 48 patients with various intracranial lesions were initially enrolled in the study. Patients were investigated by various radio-imaging techniques and routine blood investigations. Forty-one patients were operated at Netaji Subhash Chandra Bose medical college, Jabalpur. Intra-operative squash cytology diagnosis was performed and was correlated with histology diagnosis as gold standard.
Results: Out of 41 patients, inflammatory lesions were diagnosed in nine patients while benign lesions [most common neurilemmoma and meningioma] were observed in 21 and malignant lesions [astrocytoma was most common] were diagnosed in 11 patients. Diagnostic accuracy of intra-operative squash cytology irrespective of lesion & site was 95%. We were able to inform about the diagnosis to neurosurgeon in 15 minutes in all cases and within 12 minutes in >85% cases
Conclusion: Squash smear cytology is reliable and rapid standalone diagnostic method and it can assist for intra-operative decision-making diagnosis of intracranial lesions in resource-limited settings where frozen section facility is not available.
Introduction
Intracranial tumors account for 10-17 per 1,00,000 persons [1-2] . In developing countries like India, intracranial lesions can result from inflammation/infection [3] to life-threatening malignancies. An accurate diagnosis of intracranial lesions is necessary for therapeutic and prognostic reasons. The presenting clinical features of intracranial lesions are usually varied and similar for many diseases, which often results in diagnostic delays. The radiological features may not always be conclusive about etiology of the lesions. The overall inaccuracy of preoperative radiographic diagnosis ranges between 10 and 30%, thus making it impossible for the surgeon to provide the patient with adequate therapy [4] .
The explicit diagnosis of lesions is based on histological confirmation. Since fine needle aspiration of intracranial space occupying lesions is difficult due to closed architecture, neurosurgeons often need rapid intra-operative diagnosis for immediate critical decisions regarding treatment and the extent of surgical resection. For the last 50 years, imprint cytology, squash cytology and frozen sections are the mainstay for the diagnosis. Although, the choice of the method depends on individual experience and preference, and these methods were considered as complementary procedures to assist neurosurgeon in diagnosis [5] . In developing countries, frozen section has limited use in routine diagnostic practice because of limited laboratory resources either in terms of human or technical reasons [6] . Nevertheless, often the clinical and therapeutic decisions need to be made before the histological diagnosis is proven conclusive and a trial of more invasive procedures to obtain a biopsy is recommended. In such cases, cytology thus remains the only possible way to provide a rapid and reliable diagnosis even with small samples.
In view of the importance of squash cytology in diagnosis of intracranial lesions, the current study was planned to assess the feasibility and efficacy of intra-operative squash cytology as standalone method in the rapid intra-operative diagnosis of intracranial tumor and tumor-like lesions in setting where frozen section facility is not available.
Materials and Methods
Patients
The study was carried out at Netaji Subhash Chandra Bose [NS CB] Medical College, India, a 700 bedded referral hospital with tertiary care facility. All consecutive patients Presented at the Department of Neurosurgery with clinical features of space occupying lesions in central nervous system [CNS ] were enrolled in the study. The patients were investigated with radio-imaging either with CT scan [64 slice contrast/non-contrast] or MRI scan [1.5 tesla]. Complete blood count, screening for HIV were also done in all the patients. The patients were operated according to the clinical need. The final diagnosis of lesion was established on fulfillment of histological features along-with special stains such as immuno-histochemistry, wherever needed. The patients with history of traumatic concussion injury to head were excluded from the study population.
Informed written consent was obtained, and the patients were ensured of confidentiality. The decision to do surgical procedure was made on clinical demand and not for the sake of participation in the study. Ethical approval was obtained from the Institutional ethical committee at NS CB Medical College, India.
Intra-operative procedure: The investigator [MA] followed the case during the operative procedure. The mass was provided to the investigator after removal from the body. The mass was cut open and bisected in slices according to size of the mass and the surgical biopsy protocol. Two to three tissue bits, from different sites of the mass, were taken to prepare squash cytology smear. The main tissue bulk was then preserved in 10% formalin for routine paraffin embedded histology processing.
Squash smear and staining: Two squash smears were prepared from the tissue bits taken from the mass before embedding it in formalin. One squash smear was immediately fixed with 95% ethyl alcohol before drying for rapid haematoxylin & eosin [H&E]. Briefly, the smears were quick rinse in water followed by dip in Harris’s haematoxylin for one minute, then in acid alcohol [1% hydrochloric acid in 70% alcohol], and in scott’s tap water and counter stained with 0.5% eosin for 30 seconds. The second smear was air dried and kept for Giemsa stain which was done when needed. An opinion regarding the nature and type of lesion was informed to the surgeon. The time for entire procedure was noted. As frozen section facility was not available, intra-operative cytology diagnosis was compared with the histology diagnosis and the diagnostic indices of cytology were calculated on decision matrix.
Results
Forty-eight patients with intracranial tumor and tumor-like lesions were initially enrolled in the study of which seven patients either refused for operative procedure or referred to other centers. Thus, 41 patients were operated at our centre and were finally analyzed in the study. Of these, nine patients had non-neoplastic and 32 had neoplastic [21were benign and 11were malignant] lesions. The different lesions diagnosed are shown in [Table/Fig-1].
Clinical characteristics: Patients with age range of 14 to 60 years were seen with a male to female ratio of 1.3:1. Patients presented mainly with seizures, headache, nausea, vomiting, vertigo, tinnitus and difficulty of hearing. Some patients presented with local symptoms according to the site of involvement as difficulty in speech, disorientation, paralysis of right side of body, or falling suddenly. Almost any part of the brain was found involved but left cerebello-Pontine angle [80%] was the most common site of involvement followed by left frontal lobe [13.4%], right cerebello-pontine angle and right parietal lobe [10%].
Cytology diagnosis [Table/Fig-1]
The cytological features of various lesions are mentioned in [Table/Fig-1].
Non- neoplastic lesions [Table/Fig-2a-f]
Inflammatory lesions such as abscess and tuberculoma were seen. Epidermal cyst and hydatid cyst were also seen [Table/Fig-2e,f].
On gross, hydatid cyst was pearly white slippery membranous which was difficult to smear on squash. Microscopically, smear revealed scanty eosinophilic laminated structure. A wet smear examination was done from the cystic fluid that showed presence of scolex. The case was confirmed as hydatid cyst on histology.
Neoplastic lesions [Table/Fig-1]
Benign lesions were diagnosed in 21 cases, which include pituitary adenoma, schwannoma [neurilemmoma WHO grade I], transitional meningioma, meningioma [WHO grade I]. Malignant lesions were diagnosed in 11 cases [10 primary tumors and one secondary tumor]. The cytology features of type and grade of lesion were correlated with histological examination and the diagnostic accuracy of squash cytology was 95%. Intra-operative time interval of diagnosis by squash cytology was between 10-12 minutes in 85% of cases and within 15 minutes in all patients.
Discussion
Several studies [Table/Fig-3] have shown the importance of squash cytology for offering intra-operative diagnosis of intracranial lesions [7-10] . In the present study, however, we have shown that using squash cytology as standalone diagnostic procedure, it is possible to achieve consistently high sensitivity and specificity for intra- operative diagnosis of intracranial lesions even in resource-limited setting where frozen section facility is not available.
The strength of squash cytology is that it is simple, rapid, robust, provides good cellular details, allows tissue to be preserved for paraffin embedding, need minimum equipment and technical skill personnel. It can easily be availed at the operative site. One of the most important advantages is that even very tiny specimens are suitable for smear preparation, which is extremely important in surgical procedure from intracranial lesions which are localized in functionally important areas of brain [10] . In addition, it also provides excellent teaching material for cytopathologist.
According to some studies which correlated squash cytology with histopathology, the diagnostic accuracy of squash cytology was ranging from 87% to 97% [11-13] . In our study, the overall diagnostic accuracy of squash cytology was 95% when compared with histology as the gold standard, which correspond to or even better than some of the studies [11-13] . Few studies also compared results of squash cytology with frozen section and concluded that the accuracy of cytology was as good as frozen section [14-16] . In fact, studies have shown that the use of intra-operative cytology has great value in providing diagnostic information when frozen section was equivocal or when frozen-section evaluation could not be done [e.g., excessively small sample] [17] . According to Nigam et al., a well-prepared squash smear may eliminate the need for frozen section or at least influence its interpretation [18] . Further, elimination of freezing artifact [12] and reduced cryostat contamination from potentially infected tissue make squash cytology superior over frozen section [10] . Some authors suggest that cytological preparation provides better morphology than frozen section with even minute biopsy material [11,14,19] . Thus, though frozen section was considered complementary to squash cytology [5] , the latter alone can guide neurosurgeon during intra-operative period in many of the institutes where frozen section is not performed routinely for various logistic and technical reasons [9] .
One of the important finding of our study is that we could provide grading in most of the lesions with squash cytology. A good histological and grading correlation was seen in almost all types of intra-cranial lesions such as neurilemmoma, astrocytoma, craniopharyngioma, glioblastioma multiforme and pituitary aden-oma. As suggested by Powell et al., a squash cytology prepared with good amount of tissue is enriched with good cytological and histological details and a pathologist get benefits of both cytology as well as histology [20]. The cell type with differentiation of nuclear and cytoplasmic features of neurons, oligodeandroglial cells and astrocytes are well appreciated with this technique [8,20] .
In our study, we misinterpreted one case of meningioma where we over-diagnose the atypia and we could not diagnose one metastatic adenocarcinoma [with occult primary malignancy] as there was excessive degeneration and necrosis with no obvious cellular yield. In literature, misdiagnosis was seen in diagnosis of metastatic carcinoma, undifferentiated malignant tumours and rare types of histology such as gliomatosis and xanthomatous lesions, suggesting that the type and grade of lesions might be responsible for misdiagnosis [8-111421] . According to some authors, grading of intracranial lesions should not be attempted on squash smear because of the small bit of tissue and heterogeneous nature of some lesions [9] . Apart from misinterpretation, sometimes the intra-operative diagnostic difficulties could arise due to technical problems depending on the type and consistency of the tissue received. A soft and friable tissue is easier to squash then a firm tissue. We found difficult to prepare a good cellular squash smear in case of hydatid cyst because of slippery tissue. We simultaneously examine a wet preparation from the cystic fluid. The role of pathologists, however, in the intra-operative setting should be to provide sufficient preliminary information for optimal surgery rather than to provide a precise diagnosis and accurate grade for each case [9] . The limited number of patients studied in our study restricts us for evaluation of the true value of squash cytology as standalone intra-operative procedure. Our study, however, once again confirms the reliability of squash cytology and further multicentre study with larger number of patients may help to decide its use in clinical practice.
Details of intracranial lesions diagnosed on intra-operative squash cytology (N=41)
| Histology diagnosis | No. of cases n (%) | Cytology features observed on squash smear | Time * for diagnosis(minutes |
| Inflammatory (n=9) |
| Epidermal Cyst | 2 (4.9) | Clumps of anucleated squames | 10-12 |
| Abscess | 3 (7.3) | Necrosis, abundant neutrophils | 10-12 |
| Tuberculoma | 3 (7.3) | Lymphocytes, histiocytes, epithelioid cells, necrosis | 12-15 |
| Hydatid Cyst | 1 (2.4) | Eosinophilic laminated layers | 15 |
| Benign (n=21) |
| Lipoma | 1 (2.4) | Adipocytes and fat globule background | 10 |
| Neurilemmoma | 9 (21.9) | Cohesive uniform spindle, ‘twisted rope’ appearance, palisading nuclei, no nucleoli | 10-12 |
| Meningioma | 8 (19.5) | Sheets of plump spindle nuclei, whorl pattern, abundant granular cytoplasm, few psammoma bodies | 12-15 |
| Pituitary Adenoma | 2 (4.9) | Sheets of uniform round cells, eosinophilic cytoplasm, vesicular nuclei, bi- and tri-nucleate cells are also seen | 10-12 |
| Craniopharyngioma | 1 (2.4) | Clumps of uniform cells, distinct large amount of cytoplasm, round to oval nuclei | 10 |
| Malignant (n=11) |
| Astrocytoma (Grade 2) | 4 (9.7) | Moderate cellular, irregular clusters, vague papillae, cytoplasmic glial processes, no mitoses | 10-12 |
| Astrocytoma (>grade 2) | 2 (4.9) | Cellular smear, nuclear pleomorphism, mitotic figures | 12-15 |
| Glioblastoma | 1 (2.4) | Cellular, nuclear pleomorphism, mitotic figures, vascular proliferation and tumour necrosis | 15 |
| Multiforme oligodendroglioma | 1 (2.4) | Nuclear pleomorphism, scant cytoplasm, perivascular aggregates of tumour cells, calcification, mitoses, vascular proliferation, and necrosis | 12 |
| Malignant meningioma | 2 (4.9) | Plump spindle nuclei, hyper chromatic nuclei, mitoses | 12 |
| Secondaries from breast | 1 (2.4) | Abundant necrosis, no cells – Cytology conveyed to surgeon as inconclusive | 15 |
*time interval between removal of mass from the body till intra-operative diagnosis given to surgeon
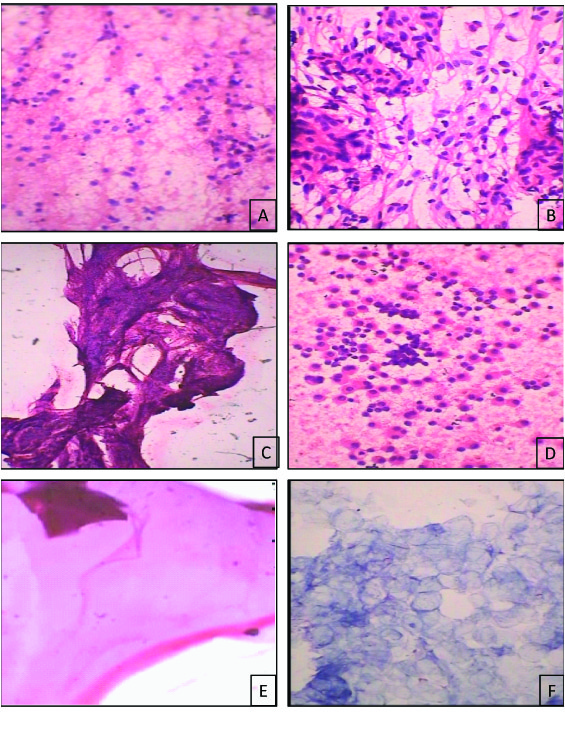
Morphology of squash cytology in various intracranial lesions [A] astrocytoma grade II, [B] transtitional meningioma , [C] neurilemmoma, [D] pituitary adenoma , [E] hydatid cyst, [F] epidermal cyst. [rapid H&E, a,c –X100, b,d,e,f-X400]
The diagnostic accuracy and discrepancies for intra-operative diagnosis of intracranial lesions from various studies
| Authors (Year) | No. of cases | Period of study (years) | Intra-operative Methods used | Diagnostic accuracy (%) | Causes of discrepancies |
| Katrina S. Firlik et al., [8] | 595 (retrospective) | 19 | Squash smear & frozen section | 90 | Inadequate or non-diagnostic sample as only red blood cells |
| Di Stefano D [19] | 85 | - | Squash smear & frozen section | 95.29 | Technical-staining defects, difficult tumor differentiation, marked tumor heterogeneity |
| Pratima Savargaonkar et al., [21] | 103 (retro spective) | 2 .5 | Squash smear & frozen section | 94 | Failure to recognize atypia in meningiomas |
| Sumit mitra et al., [5] | 114 | 1.5 | Squash smear & frozen section | 88.5 | Sampling error, under grading of gliomas & error in recognition of cell type |
| Nasir Ud Din et al., [21] | 171 | 6 .5 | Cytology* & frozen section | 94.1 | Typing of glial neoplasm & sampling error |
| Roessler et al.,[10] | 4172 (retro spective) | 15 | Cytology* | 95 | Grading variation |
| Tilgner Johannes et al. | 4589 (retro spective) | 11 | Cytology* | 90.3 | Divergence in the grade of malignancy |
| D. Goel et al.,[6] | 3057 (retros pective) | 17 | Squash smear | 85 | Difficult to spread tissue & obtain representative sample, difficult to grade & diagnose mixed tumors |
| N . Krishnani et al., [7] | 334 | 3.5 | Squash smear | 94.9 | Nature of tissue, non-representative samples. |
| Present study | 41 | 1.0 | Squash smear | 95 | Over diagnosis of atypia in meningioma, degeneration in metastatic adenocarcinoma |
*type of cytology is not specified in the study
Conclusion
our study provides the insight for the feasibility of using the technique as standalone diagnostic technique for better management of patients in setting where frozen section facility is not available. We believe the squash cytology findings if interpreted in an algorithm together with the clinical picture and radio-imaging findings will help to reach an accurate and rapid diagnosis of intracranial lesions.
*time interval between removal of mass from the body till intra-operative diagnosis given to surgeon
*type of cytology is not specified in the study
[1]. WS Parkin, J Ferlay, L Raymond, J Young, Cancer incidence in five continents.IARC. L 1997 8(143):127-29. [Google Scholar]
[2]. AA Kumar V, N Fausto, JA Aster, Tathologic basis of disease.Cotran R, editor. 2004 7th EditionPhiladelphiaElsevier [Google Scholar]
[3]. C Sundaram, Diagnostic utility of squash [smear] technique in the inflammatory lesions of central nervous system.Indian Journal of Pathology & Microbiology 2003 46(4):569-72. [Google Scholar]
[4]. D Kondziolka, LD Lunsford, AJ Martinez, Unreliability of contemporary neurodiagnostic imaging in evaluating suspected adult supratentorial [low-grade] astrocytoma.Journal of Neurosurgery. 1993 79(4):533-36. [Google Scholar]
[5]. I Wilson, A method for the rapid preparation of fresh tissues for the microscope.JAMA 1905 45:1737 [Google Scholar]
[6]. BJ Olasode, JW Ironside, The brain smear, a rapid affordable intraoperative diagnostic technique for brain tumours appropriate for Africa. Tropical Doctor. 2004 34(4):223-25. [Google Scholar]
[7]. S Mitra, M Kumar, V Sharma, D Mukhopadhyay, Squash preparation: A reliable diagnostic tool in the intraoperative diagnosis of central nervous system tumors. Journal of cytology / Indian Academy of Cytologists. 2010 27(3):81-85. [Google Scholar]
[8]. D Goel, C Sundaram, TR Paul, SG Uppin, AK Prayaga, MK Panigrahi, Intraoperative cytology [squash smear] in neurosurgical practice - pitfalls in diagnosis experience based on 3057 samples from a single institution. Cytopathology Official Journal of the British Society for Clinical Cytology 2007 18(5):300-08. [Google Scholar]
[9]. N Krishnani, N Kumari, S Behari, C Rana, P Gupta, Intraoperative squash cytology: accuracy and impact on immediate surgical management of central nervous system tumours. CytopathologyOfficial Journal of the British Society for Clinical Cytology 2012 23(5):308-14. [Google Scholar]
[10]. KS Firlik, AJ Martinez, LD Lunsford, Use of cytological preparations for the intraoperative diagnosis of stereotactically obtained brain biopsies: a 19- year experience and survey of neuropathologists.Journal of Neurosurgery. 1999 91(3):454-58. [Google Scholar]
[11]. LF Bleggi-Torres, L de Noronha, E Schneider Gugelmin, AP Martins Sebastiao, B Werner, E Marques Maggio, Accuracy of the smear technique in the cytological diagnosis of 650 lesions of the central nervous system.Diagnostic Cytopathology. 2001 24(4):293-95. [Google Scholar]
[12]. K Roessler, W Dietrich, K Kitz, High diagnostic accuracy of cytologic smears of central nervous system tumors. A 15-year experience based on 4,172 patients. Acta Cytologica. 2002 46(4):667-74. [Google Scholar]
[13]. T Asha, SK Shankar, TV Rao, S Das, Role of squash-smear technique for rapid diagnosis of neurosurgical biopsies--a cytomorphological evaluation.Indian Journal of Pathology & Microbiology 1989 32(3):152-60. [Google Scholar]
[14]. LA Guarda, Intraoperative cytologic diagnosis: evaluation of 370 consecutive intraoperative cytologies.Diagnostic Cytopathology 1990 6(4):235-42. [Google Scholar]
[15]. Y Liu, JF Silverman, CD Sturgis, HG Brown, DJ Dabbs, SS Raab, Utility of intraoperative consultation touch preparations. Diagnostic Cytopathology. 2002 26(5):329-33. [Google Scholar]
[16]. LF Scucchi, D Di Stefano, L Cosentino, A Vecchione, Value of cytology as an adjunctive intraoperative diagnostic method. An audit of 2,250 consecutive cases. Acta Cytologica. 1997 41(5):1489-96. [Google Scholar]
[17]. v Kim, KG Lee, TS Kim, Cytologic characteristics of subependymal giant cell astrocytoma in squash smears: morphometric comparisons with gemistocytic astrocytoma and giant cell glioblastoma.Acta Cytologica. 2007 51(3):375-79. [Google Scholar]
[18]. J Nigam, V Misra, V Dhingra, S Jain, K Varma, A Singh, Comparative study of intra-operative cytology, frozen sections, and histology of tumor and tumor-like lesions of nose and paranasal sinuses. Journal of Cytology / Indian Academy of Cytologists. 2013 30(1):13-17. [Google Scholar]
[19]. EM Cahill, DF Hidvegi, Crush preparations of lesions of the central nervous system. A useful adjunct to the frozen section.Acta Cytologica. 1985 29(3):279-85. [Google Scholar]
[20]. SZ Powell, Use of cytological preparations for the intraoperative diagnosis of stereotactically obtained brain biopsies: a 19- year experience and survey of neuropathologists.Archives of Pathology & Laboratory Medicine. 2005 129(12):1635-52. [Google Scholar]
[21]. N Ud Din, A Memon, R Idress, Z Ahmad, S Hasan, Central nervous system lesions: correlation of intraoperative and final diagnoses, six year experience at a referral centre in a developing country, Pakistan.Asian Pacific Journal of Cancer Prevention : APJCP 2011 12(6):1435-37. [Google Scholar]