Carcinoma cervix has been reported to be the commonest cancer by nine (Calcutta, Bhopal, Nagpur, Aurangabad, Pune, Barshi, Banglore, Chennai, Karunagappally) out thirteen population based cancer registries in India [1]. It accounts for 80% of total genital cancers in our country [2]. Invasive cancer of the cervix has been considered as preventable because it has a long preinvasive state, cervical cytology screening programmes are available and the treatment of preinvasive lesions is effective. Cervical screening programmes aims to detect women who have an epithelial abnormality that might; if untreated, leads to the development of cervical carcinoma. Most widely used test for cervical carcinoma screening is cervical cytology which has been successful in reducing the incidence of cervical cancer deaths by 70% since 1950 [3]. In India, unhealthy cervix is a common finding on per speculum examination in gynaecology Out Patient Department (OPD) and it is recommended to do the cervical cytology to detect any epithelial cell abnormality.
The current cytological terminology “The Bethesda System” was the result of work of an expert panel which convened in 1988 under the despises of the National Cancer Institute [4]. The Bethesda System replaced the three levels of dysplasia and carcinoma in situ with two levels, Low grade squamous intra epithelial lesion (LSIL) and High grade squamous intra epithelial lesion (HSIL). Minor modifications were incorporated in the 1991 Bethesda System Terminology. The revised 2001 Bethesda System includes changes that are based on clinical input and advances in the understanding of the biology of cervical cancer [5]. While giving statements about specimen adequacy and general categorization (normal, benign cellular change or epithelial abnormality), this system also gives descriptive diagnosis. Histopathology remains the gold standard for diagnosis of the intra-epithelial lesions and invasive cancer of the cervix. This study was planned with the aim to detect epithelial cell abnormalities in unhealthy cervix using Bethesda system of reporting for cervical cytology and to confirm histopathologicaly the findings of Pap smear.
Materials and Methods
In this study, 125 patients with the clinical diagnosis of unhealthy cervix, who attended Gynecology OPD at our institute, were studied over a period of one year. After Hospital ethics committee clearance, informed consent was taken from all the patients under study. The criteria for inclusion of patients with unhealthy cervix in the study were: Erosion, Chronic cervicitis, and Healed lacerations, Hypertrophied cervix, bleeding on touch, suspicious growth / ulcer / polyp on the cervix and Abnormal discharges from the cervix. Women with frank carcinoma cervix, pregnant females, patients with bleeding per vaginum at the time of examination and those who had used vaginal medications, vaginal contraceptives or douches in the last 48 h of examination were excluded from the study. After taking a detailed history and doing thorough clinical examination, Pap smear was taken using conventional method for cervical cytology in all the patients. After asking the patient to empty the urinary bladder, they were put on the examination table in dorsal position and speculum was introduced into the vagina to expose the cervix. A Medscand Cell Sampling Kit (manufactured by Medscand Medical AB, Sweden) was used for taking cervical cytology. The endocervical cell sampling was done by using the cytobrush which was introduced into the cervical os along its axis till few bristles remained outside the os. The brush was rotated by 180o, maintaining the contact with the cervical canal. The sample was unrolled onto the slide in the opposite direction from which it was collected by twirling the handle of the brush. The slide was fixed immediately in 95% ethyl alcohol in Coplin’s jar. Next, the pointed end of the plastic Colin’s Ayres spatula was introduced into the cervical os and rotated 360o about the circumference of the os maintaining constant contact with the ectocervix and both surfaces of the spatula were smeared on a new slide and fixed immediately. After this, using the blunt end of the Ayres spatula, sample was taken from the posterior fornix and the material obtained was spread on a next slide and fixed immediately. All the three slides obtained were numbered as 1, 2 and 3 in the sequence in which they were prepared. After fixing, the slides were sent to the Pathology Department, stained with the Papnicolaou staining method [6]. Reporting of the slides was done according to The 2001 Bethesda system [5] by the consultant pathologist as follows:
Specimen Adequacy
Satisfactory for evaluation (note presence / absence of endocervical. The Transformation zone component)
Unsatisfactory for evaluation (specify reason)
Specimen rejected / not processed (specify reason)
Specimen processed and examined, but unsatisfactory for evaluation of epithelial abnormality because of Specific reason
General Categorization (Optional)
Negative for intraepithelial Lesions or Malignancy
Epithelial cell abnormality
Others
Interpretation / Result
Negative for intraepithelial Lesions or Malignancy
Organisms
* Trichomonas vaginalis
* Fungal organisms morphologically consistent with Candida species
* Shift in flora suggestive of bacterial vaginosis.
* Bacteria morphologically consistent with Actinomyces species
* Cellular changes consistent with herpes simplex virus
Other non neoplastic findings (Optional to report; list not comprehensive)
* Reactive cellular changes associated with Inflammation (includes typical repair)
Radiation
Intrauterine contraceptive device
* Glandular cells status post-hysterectomy
Atrophy
Epithelial Cell Abnormalities
Squamous cell
Atypical squamous cells (ASC)
* of undetermined significance (ASC-US)
* Cannot exclude HSIL (ASC-H)
Low grade squamous intraepithelial lesion (LSIL)
* Encompassing: human papillomavirus / mild dysplasia/ cervical intraepithelial neoplasia
(CIN)
High grade squamous intraepithelial lesion (HSIL)
* Encompassing: moderate and severe dysplasia, carcinoma in situ: (CIN2 and CIN 3)
Squamous cell carcinoma
Glandular cell
Atypical glandular cells (AGC) (specify endocervical, endometrial, or not otherwise specified)
Atypical glandular cells, favour neoplastic (specify endocervical or not otherwise specified)
Endocervical adenocarcinoma in situ (AIS)
Adenocarcinoma
Other (List not comprehensive)
* Endometrical cells in a woman > 40 y of age.
Automated Review and Ancillary Testing (Include as Appropriate) Educational Notes and Suggestions (Optional)
Under all aseptic precautions, colposcopy directed cervical punch biopsy was taken in patients with abnormal colposcopic findings. The biopsy specimen was sent in 10% formalin solution for histopathological examination to the pathology department. Reports of Pap smear and histopathology were collected, tabulated and analyzed using SPSS, version 17 and presented as simple percentages. Sensitivity, specificity and predictive values were calculated using 2 x 2 tables and standard formulae.
Results
In this study the age of the patients ranged from 21 to 62 y. 42.40% of patients were in 31 - 40 y of age group. Maximum number of women (53.60%) belonged to middle class, followed by 25.60% in lower and 20.80% patients in upper class of socio economic status. Sikh and Hindu population with 61 patients (48.80%) each dominated the study. Urban population was 63.20% as compared to the rural population which was 36.80%. One hundred one (80.80%) women were premenopausal and 24 (19.20%) were postmenopausal. 44.80% women were married at the age of 18 to 20 y and 32 (25.60%) were married at the age of 21 to 23 y. Eighteen patients got married at the age less than 17 y. Mean age of marriage was 20.42 ± 3.082 y. Most of the women (44%) had not used any contraceptive method. Barrier method was the commonest (25.60%), followed by tubal ligation (20.80%), copper-T (6.40%) and the least used contraceptive method was injection Depo-Provera. [Table/Fig-1] shows the distribution of women according to per speculum examination. The most common findings on clinical examination of the cervix were chronic cervicitis (41), erosion (34) and hypertrophied cervix (18). In all these patients inflammatory Pap smears were present in 73.17%, 61.76% and 83.33% cases respectively. ASC-US was seen in 6 patients; with clinical diagnosis of erosion (1), hypertrophy with bleeding on touch (2), congestion with bleeding on touch (1), suspicious cervix (1) and suspicious with bleeding on touch (1). LSIL (HPV) in Pap smear was seen in three patients; in whom one patient each had clinical diagnosis of chronic cervicitis, erosion and erosion with bleeding on touch. Out of 4 LSIL Pap smears, two were seen in patients with chronic cervicitis and one each in patient with hypertrophy with bleeding on touch and healed laceration respectively. One patient with HSIL had a clinical diagnosis of erosion. Squamous cell carcinoma in Pap smear was seen in one patient with cervical polyp. Atypical glandular cells of endocervical cells were seen in one patient with congestion with bleeding on touch. Adenocarcinoma on Pap smear was seen in one patient with suspicious cervix. Three unsatisfactory smears were seen in two patients with clinical diagnosis of chronic cervicitis and one with erosion.
Distribution of women according to Perspeculum examination
Bot - Bleed on touch
| Examination | No. of Patients (N=125) | %age |
|---|
| Vagina |
| Healthy | 106 | 84.80 |
| Vaginitis | | |
| Bacterial | 11 | 8.80 |
| Trichomonal | 4 | 3.20 |
| Candidasis | 1 | 0.80 |
| Cystocele | 2 | 1.60 |
| Vaginal cyst | 1 | 0.80 |
| Cervix |
| Chronic cervicitis | 41 | 32.80 |
| Erosion | 34 | 27.20 |
| Erosion, bleeds on touch | 5 | 4.00 |
| Hypertrophied | 18 | 14.40 |
| Hypertrophied, bleeds on touch | 5 | 4.00 |
| Congestion, bleeds on touch | 7 | 5.60 |
| Healed laceration | 4 | 3.20 |
| Cervical Polyp | 3 | 2.40 |
| Congestion | 2 | 1.60 |
| Suspicious | 2 | 1.60 |
| Flushed with Vagina, Bot | 1 | 0.80 |
| Suspicious, Bot | 1 | 0.80 |
| Irregular Contour, Bot | 1 | 0.80 |
| White Plaque on Anterior Lip | 1 | 0.80 |
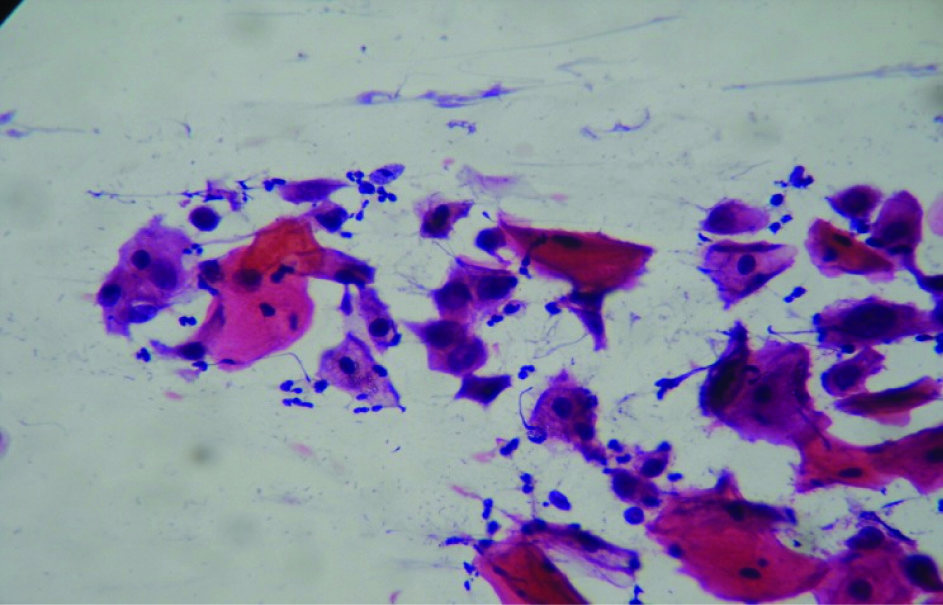
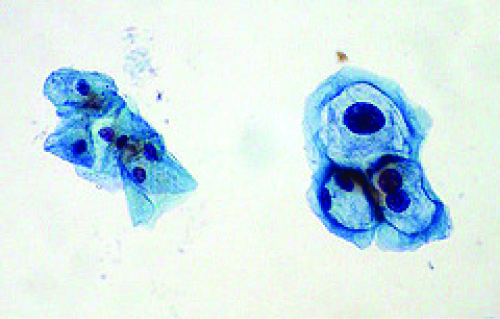
Distribution of women according to The 2001 Bethesda system Pap smear reports is shown in [Table/Fig-2] and pictomicrographs of the different grades of the system in [Table/Fig-3,4,5,6,7,8]. Out of 125 Pap smears, 122 were satisfactory for evaluation (19 normal, 86 negative for intraepithelial lesion or malignancy and 17 with epithelial cell abnormality) and rest 3 were unsatisfactory (one hemorrhagic and two severe inflammatory). Out of 17 (13.60%) cases with epithelial cell abnormality, ASC-US was seen in 6 (4.80%), LSIL in 7 (5.60%) {Total LSIL = LSIL HPV in 3 (2.40%) + LSIL in 4 (3.2%)}, HSIL in 1 (0.80%), squamous cell carcinoma in 1 (0.80%), AGC endocervical in 1 (0.80%) and adenocarcinoma in 1 (0.80%) patients. Three women with unsatisfactory smears were excluded from the study and rest 122 patients with satisfactory cervical smears were further assessed by colposcpoy and cervical biopsy was taken in 67 women with abnormal colposcopic findings.
Distribution of women according to The 2001 Bethesda system Pap smear reports
| Pap Smear Report | No. of Patients (n=125) | %age |
|---|
| SPECIMEN ADEQUACY |
| a)Unsatisfactory for evaluation | 3 | 2.40 |
| b)Satisfactory for evaluation 122 (97.60%) |
| INTEPRETATION / RESULTS |
| a)Normal | 19 | 15.20 |
| b) Abnormal 103 (82.40%) |
| 1) NILM 86 (68.80%) |
| Trichomonas vaginalis | 1 | 0.80 |
| Candida species | 3 | 2.40 |
| Altered Bacterial Flora | 2 | 1.60 |
| Inflammatory | 76 | 60.80 |
| Atrophic Pattern | 4 | 3.20 |
| 2) Epithelial Cell Abnormality 17 (13.60%) |
| Squamous |
| ASC-US | 6 | 4.80 |
| LSIL | 7 | 5.60 |
| HSIL | 1 | 0.80 |
| Squamous cell carcinoma | 1 | 0.80 |
| Glandular |
| AGC-endocervical | 1 | 0.80 |
| Adeno carcinoma | 1 | 0.80 |
| Total | 125 | 100 |
NILM (Negative for intraepithelial lesions or malignancy), ASC-US(atypical squamous cells of unknown origion), LSIL (low grade squamous intraepithelial lesion), HSIL (high grade squamous intraepithelial lesion), AGC (atypical glandular cells)
Inflammatory smear (Pap stain, 400x)

LSIL - HPV (Pap stain, 400x)
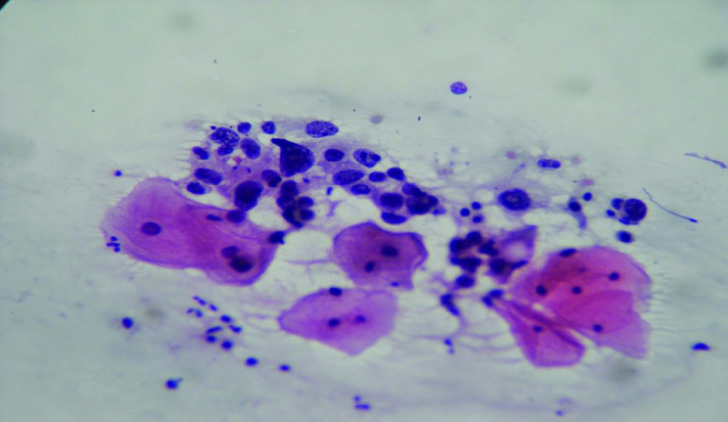
Squamous Cell Carcinoma (Pap stain, 400x)
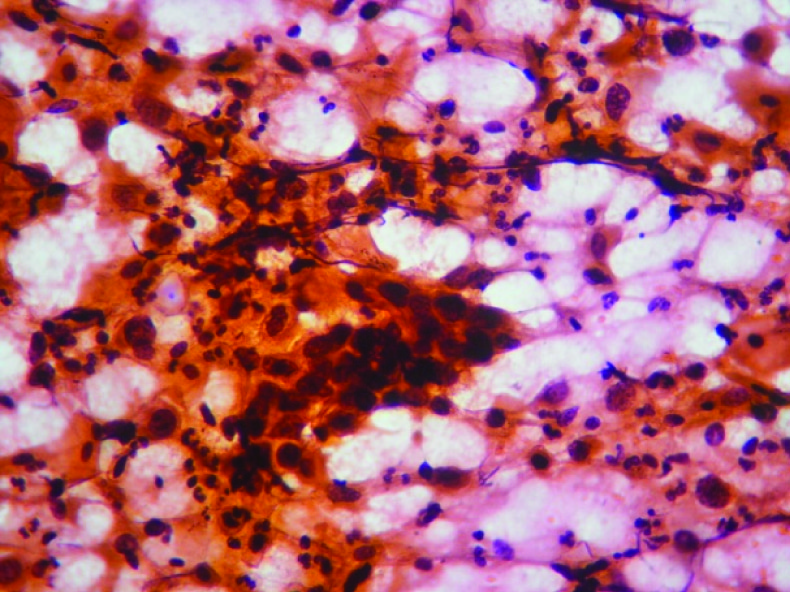
Adenocarcinoma (Pap stain, 400x)

The results of histopathology (n=67) are shown in [Table/Fig-9]. Pap smear with HSIL in one patient showed squamous cell carcinoma on biopsy of the cervix. One smear with AGC showed CIN 1 on cervical biopsy and one smear with adenocarcinoma was shown to have CIN 2/3 and endometrial adenocarcinoma on further investigations. Pap smear of one patient with squamous cell carcinoma revealed microinvasive squamous cell carcinoma on cervical biopsy.
Association of Cervical biopsy and Pap smear reports of 67 women
| Biopsy | No. of patients | Pap Smear Report |
|---|
| WNL | Inf | Atr | ASCUS | LSIL-HPV | LSIL | HSIL | sq c ca | AGC | ACA |
|---|
| Chc | 39 | 4 | 27 | 3 | 5 | | | | | | |
| Chc, sq met | 7 | 1 | 6 | | | | | | | | |
| Chc,ecp | 5 | 1 | 4 | | | | | | | | |
| Chc,ero | 1 | | | | 1 | | | | | | |
| Ehf | 1 | | 1 | | | | | | | | |
| CIN 1 (HPV) | 2 | | | | | 2 | | | | | |
| CIN 1 | 9 | | 3 | | | 1 | 4 | | | 1 | |
| CIN 2/3 | 1 | | | | | | | | | | 1 |
| MISCCa | 1 | | | | | | | | 1 | | |
| sq c ca | 1 | | | | | | | 1 | | | |
| Total | 67 | 6 | 41 | 3 | 6 | 3 | 4 | 1 | 1 | 1 | 1 |
Chc - chronic cervicitis, sq met - squamous metaplasia, ecp - endocervical polyp, ero - erosion, Ehf - epithelial hyperplasia with fibrosis, CIN – cervical intraepithelial neoplasm, HPV - human papilloma virus, MISCCa - micro invasive squamous cell carcinoma, sq c ca - squamous cell carcinoma, WNL – within normal limits, Inf- inflammation, Atr - atrophic, ASCUS - atypical squamous cells of unknown origion, LSIL - low grade squamous intraepithelial lesion, HSIL - high grade squamous intraepithelial lesion, AGC - atypical glandular cells endocervical, ACA - adenocarcinoma
[Table/Fig-10] shows that 67 women in whom cervical biopsy was done, the overall sensitivity and specificity of Pap smear for pre-invasive and invasive disease was78.57% and 88.67% respectively with a predictive value of 64.71%. Pap smears overestimated the pre invasive and invasive diseases in 35.29% of cases and was not able to detect in 6.00% of the cases. Diagnostic accuracy of Pap smear for pre-invasive and invasive disease was 81.15%.
Overall sensitivity, specificity and diagnostic accuracy of Pap smear for preinvasive and invasive disease in (67) women in whom cervical biopsy was done
| | Histopathology | |
|---|
| Positive | Negative |
|---|
| Pap Smear | Positive | 11(a) | 6(b) | 17 |
| Negative | 3(e) | 47(d) | 50 |
| Total | 14 | 53 | 67(f) |
| Sensitivity = ax100/a+e = 11 x100/(11+3)=78.57% |
| Specificity = d x100/(b+d) = 47 x100/6+47=88.67% |
| Predictive value = a x100/(a+b) =11 x100/6+11=64.71% |
| False +ve rate = b x100/(a+b) = 6 x100/6+11=35.29% |
| False -ve rate = e x100/(e+d) = 3 x100/3+47=6.00% |
| Diagnostic accuracy = [a+d]x100/f = [11+47]100/67 = 81.15% |
Discussion
Cancer of the cervix is a preventable disorder as the different screening, diagnostic and therapeutic procedures are effective. One of the essential responsibilities of the gynaecologist is to detect neoplasm of the genital tract at the earliest. Since the introduction of cytology into clinical practice by Papanicolaou and Traut in 1944, it has become possible to detect cervical cancer in its preinvasive stages, thus reducing the morbidity and mortality from this disease.
The present study was conducted on 125 patients with the clinical diagnosis of unhealthy cervix. Conventional cervical cytology was done in all the women. One hundred twenty two smears were found to be satisfactory for evaluation. For confirmation of the cytology report all women underwent colposcopic examination and biopsies were taken in those with abnormalities. Final diagnosis was made according to the histopathology reports.
In this study, maximum patients (42.40%) belonged to age group of 31- 40 y. 25.60% women were from lower socio-economic status. Most of the women (81.60%) were housewives. Mean age at time of marriage was 20.04± 3.26 y and 12% of them conceived before the age of 18 y. 56% of the women were using contraceptive measures. Most of the women were (80.80%) were premenopausal and rest (19.20%) was post menopausal. Most common presenting complaint was discharge per vaginum (54.40%), followed by pain abdomen (45.60%) and post coital bleeding (16.80%).
Our study demonstrated 17 cases of epithelial cell abnormality on cervical cytology out of total 125 cases examined. In these 17 cases, the clinical diagnosis was chronic cervicitis, erosion, hypertrophied cervix which bled on touch (17.65% each); congestion bleeding on touch, suspicious (11.76% each); erosion bleeds on touch, healed laceration, polyp and suspicious bleeding on touch (5.88% each). Padambhan et al., also found the same type of findings in 80 cases of CIN he studied [7]. He reported the clinical diagnosis of erosion in 31.25% cases, unhealthy cervix in 18.75%, hypertrophied cervix in 23.75%, hypertrophy with erosion in 2.5%, bleeding on touch in 10% and miscellaneous findings in rest 15% of the cases.
In the present study 97.6% (122) Pap smears were satisfactory for evaluation. 15.20% (19) were normal smears, 68.80% (86) were negative for intraepithelial lesion or malignancy and epithelial cell abnormality was found in 13.6% (17) smears. Three smears (2.4%) were unsatisfactory for evaluation (one hemorrhagic and two severe inflammatory). Epithelial cell abnormalities reported on cervical cytology were ASC-US in six smears (4.8%), LSIL in 7 smears (5.6%), HSIL in one smear (0.8%), squamous cell carcinoma in one smear (0.8%), atypical glandular cells in one smear (0.8%) and adenocarcinoma in one smear (0.8%). Similar study was done by Das et al., on 960 women with clinically diagnosed as having unhealthy cervix [8]. In their study all were married, had low socio economic status, majority of them in age group of 25to 45 y with parity of 3 or 4. Common presenting symptoms were vaginal discharge and irregular vaginal bleeding and 13.53% of smears had abnormal cytological pictures. Normal smears were 3.96%, inflammatory 82.50%, mild dysplasia 5.62%, moderate dysplasia 3.23%, severe dysplasia 1.98%, carcinoma in situ 1.14% and invasive carcinoma 1.56%. Presenting complaints and prevalence of abnormal cytology in our study is comparable to that reported by Das et al., Sankaranarayanan et al., reported that the test positivity rates of cytology were 8.8% at ASCUS, 6.2% at LSIL and 1.8% at HSIL thresholds, and 355 women had histologically confirmed HSIL while 74 had invasive cancer amongst 22,663 women aged 25–65 y with conventional cytology in a multicentre screening study in India [9]. Manjit et al., observed that maximum number of patients (45.3%) were in the age group of 31- 40 y (fourth decade) in their study on detection of abnormal cervical cytology in 300 papnicolaou smears [10]. The most common presenting complaint was discharge per vaginum present in 177 (59%) patients which is same as our results. They observed that epithelial cell abnormalities were found in 5% smears, atypical squamous cells of undetermined significance (ASCUS) in 0.3%, squamous intraepithelial lesion (SIL) in 3.4% which includes low grade squamous intraepithelial lesion (LSIL) (2.7%) and high grade squamous intraepithelial lesion (HSIL) 0.7%. Invasive carcinoma was seen in 1.3% cases. The prevalence of positive cytology (13.6%) was more in our study as compared to that reported by Manjit et al., (5%) because our study was done in women presenting with unhealthy cervix who were referred to our institute. [Table/Fig-11] shows the comparison of epithelial cell abnormalities in Pap smears using the revised Bethesda system in recent studies [9–12] from India and abroad. In our study, diagnostic accuracy of Pap smear for preinvasive and invasive disease was 81.15%. In 67 patients, in whom cervical biopsy was done, the overall sensitivity and specificity of Pap smear for preinvasive and invasive disease was 78.57% and 88.67% respectively with a predictive value of 64.71%. Pap smears overestimated the pre invasive and invasive diseases in 35.29% of cases and was not able to detect in 6.00% of the cases. Sankaranarayanan et al., reported the conventional cytology sensitivity between 37.8–813% at ASCUS, 28.9–769% at LSIL and 24.4–723% at HSIL thresholds [9].
Comparison of epithelial cell abnormalities in Pap smears using the revised Bethesda system in recent studies from India and abroad
| Study | Year | Method | % US | % ECA | % of revised Bethesda categories |
|---|
| ASC-US | ASC-H | LSIL (+HPV) | HSIL | SCC | AGC | ADC |
|---|
| Sankara-narayanan et al.,[9] | 2004 | C | 3.8 | 17.02 | 8.8 | - | 6.2 | 1.8 | 0.22 | - | - |
| Bal et al.,[10] | 2012 | C | 4.1 | 5 | 0.3 | - | 2.7 | 0.7 | 1.3 | - | - |
| Altaf and Mufti [11] | 2012 | C + L | 0.85 | 17.3 | 9.3 | 0.8 | 2.7 | 0.9 | 0.06 | 3.38 | - |
| Mulazim et al., [12] | 2012 | C | 1.8 | 10.2 | 1 | - | 4.6 | 2.2 | 1.4 | 0.4 | 0.6 |
| Present | 2014 | C | 2.4 | 13.6 | 4.8 | - | 5.6 | 0.8 | 0.8 | 0.8 | 0.8 |
C (conventional), +L (liquid based cytology), US (unsatisfactory), ECA (epithelial cell abnormalities), ASC-US(atypical squamous cells of unknown origin), LSIL (low grade squamous intraepithelial lesion), +HPV (human papilloma virus), HSIL (high grade squamous intraepithelial lesion), SCC (squamous cell carcinoma), AGC (atypical glandular cells), ADC (adenocarcinoma)
In the present study both cytobrush and plastic spatula were used to prepare the Pap smears by the first author and all the smears were reported by a single cytopathologist reducing the bias of technique and observer variation. The percentage of unsatisfactory Pap smears was only 2.4% in our study which is comparable to 3.8% as reported by Sankaranarayanan et al., [9]. ASCUS rate of our study was 4.8% which depicts that the standardized diagnostic criteria for cervical cytological reporting were used by cytopathologist, so that the rate of atypical squamous cells (ASC) was between 3 to 5% of cytological diagnosis for accurate reporting as reported by Kurman et al., [13].
Acknowledgment
We are thankful to Dr R K Gupta, Former Senior Consultant and Head of Department of Pathology, M.D. Oswal Cancer Treatment and Research Foundation Ludhiana, Punjab, for cytology and histopathology reporting.
Conclusion
Women with clinical diagnosis of unhealthy cervix need cervical evaluation to detect any premalignant or malignant lesions of cervix. The Bethesda system used for cervical cytology is not only a uniform and standard method but also gives descriptive diagnosis that helps the gynaecologist in individualized patient management. Communication between gynaecologist and cytopathologist is required for best results of the cervical cytology reporting.
NILM (Negative for intraepithelial lesions or malignancy), ASC-US(atypical squamous cells of unknown origion), LSIL (low grade squamous intraepithelial lesion), HSIL (high grade squamous intraepithelial lesion), AGC (atypical glandular cells)
Chc - chronic cervicitis, sq met - squamous metaplasia, ecp - endocervical polyp, ero - erosion, Ehf - epithelial hyperplasia with fibrosis, CIN – cervical intraepithelial neoplasm, HPV - human papilloma virus, MISCCa - micro invasive squamous cell carcinoma, sq c ca - squamous cell carcinoma, WNL – within normal limits, Inf- inflammation, Atr - atrophic, ASCUS - atypical squamous cells of unknown origion, LSIL - low grade squamous intraepithelial lesion, HSIL - high grade squamous intraepithelial lesion, AGC - atypical glandular cells endocervical, ACA - adenocarcinoma
C (conventional), +L (liquid based cytology), US (unsatisfactory), ECA (epithelial cell abnormalities), ASC-US(atypical squamous cells of unknown origin), LSIL (low grade squamous intraepithelial lesion), +HPV (human papilloma virus), HSIL (high grade squamous intraepithelial lesion), SCC (squamous cell carcinoma), AGC (atypical glandular cells), ADC (adenocarcinoma)