Introduction
Heart failure is one of the leading causes of death worldwide [1]. The actual prevalence of heart failure in the developed countries is 1–2% of the general population [2]. The burden of heart failure and its societal cost are enormous, thereby epitomizing a public health problem. In the last decade heart failure has also emerged as a major health problem in developing countries, imposing an escalating burden on their health care systems.
As the population ages, the prevalence of heart failure is likely to increase and so also the expenditure related to care of patients with this debilitating disease, posing a serious burden on the individual as well as the State. In India, though the actual data is not available, it is postulated that due to increasing prevalence of cardiovascular diseases and improved longevity, burden of chronic heart failure is likely to increase in the coming years.
Therefore, it is of utmost importance to develop strategies to contain this staggering health and economic burden. Such strategies may include adopting approaches for preventing heart failure and implementing new treatment modalities into large-scale clinical practice. For successful implementation of these strategies, it is imperative to understand the pathophysiology of the disease, diagnose it early, and design preventive and curative methods.
Even though the comprehension of the pathophysiology of Congestive Heart Failure has evolved from that of a simple pump failure to that of a multi system disorder, there is paucity of robust criteria which identify heart failure early in its course. Signs and symptoms of heart failure remain non-specific (dyspnea, exercise intolerance, fatigue, weakness) and often can be attributed to other conditions, such as pulmonary disease, anaemia, hypothyroidism, depression, and obesity. Several criteria for establishing the diagnosis have been proposed including the Framingham criteria, [3] the Boston criteria, [4] the Gothenburg criteria, [5] and the European Society of Cardiology criteria [6]. All of them focus on similar indicators of symptoms and elevated filling pressures and combine data from the medical history, physical examination and chest X-ray. Utilizing echocardiographic criteria of ejection fraction for classifying heart failure may help in identifying only 20-40% cases. Moreover these criteria fail to identify the magnitude of the problem completely due to its utility being mainly late in the course of the disease missing the early and subtle presentations
Pathophysiology of heart failure has been extensively unravelled and this has led to the identification of many categories of potential biomarkers. Based on pathophysiological stages these comprise of biomarkers of inflammation, oxidative stress, extracellular-matrix remodelling, neurohormones, myocyte injury and stress, with an additional group of new biomarkers under characterization. Studies have tried to identify an ideal biomarker which can be used as an indicator for heart failure for early diagnosis and is helpful in risk stratification and monitoring therapy [7]. Methyl malonic acid(MMA) is one such metabolite implicated and this is supported by the presence of heart defects in large number of children with methyl malonic academia [8]. We therefore planned to evaluate the potential role of MMA as a biomarker in patients with IHF.
Materials and Methods
The study was an observational, non interventional study conducted in a tertiary care teaching hospital in the months of June and July, 2011. Subjects attending the Hypertension clinic, Preventive Cardiology Clinic, Emergency, General Medicine Wards and Coronary Care Unit were included in the study after obtaining a written informed consent. The study was approved by the ethical committee of the Institution. Since the current study was a pilot study, hence a sample size of convenience which included 20 patients with IHD, 20 with IHF and 20 normal age and sex matched controls were considered. The diagnosis of heart failure was based on Framingham criteria [3]. It was based on simultaneous presence of at least two of the following major criteria or one major criterion in conjunction with two of the following minor criteria. Major criteria considered were cardiomegaly on chest radiography, presence of a third heart sound, acute pulmonary oedema, paroxysmal nocturnal dyspnea, crackles on lung auscultation, central venous pressure of more than 16 cm water at the right atrium, jugular vein distension, positive abdominojugular test, and weight loss of more than 4.5 kg in 5 days in response to treatment. The minor criteria were tachycardia of more than 120 beats per minute, nocturnal cough, dyspnea on ordinary exertion, pleural effusion, decrease in vital capacity by one third from maximum recorded, hepatomegaly and bilateral ankle oedema.
The patients of IHF were classified using Killip Classification [9]. Patients who had no signs of cardiac decompensation were included in class One. Patients with heart failure-with rales, third heart sound and venous hypertension were included in Class two. Patients with severe heart failure with presence of pulmonary oedema were included in Class three. Patients with cardiogenic shock determined by presence of hypotension (systolic blood pressure <90 mm Hg) and evidence of peripheral vasoconstriction such as oliguria, cyanosis and diaphoresis were included in Class four. The diagnosis of ischaemic heart disease was based on ECG findings according to Minnesota criteria [10] based on the presence of pathological Q waves, ST elevation or depression. Along with this a positive cardiac troponins test was also considered in the diagnosis.
Patients with clinical evidences of Vit B12 deficiency hyperpigmentation of knuckles, glossitis, and stomatitis were excluded because deficiency of Vit B12 could be associated with increased amounts of methyl malonic acid, hence would act as a confounding factor
Sample Collection, Preparation, Extraction and Analysis
Ten ml of early morning urine sample was collected from the above stated participants in capped plastic containers as this is believed to yield the best results [11]. The samples were then stored at room temperature and transported for analysis within 24 hours of collection. The urinary creatinine level was determined by modified Jaffes method [12] and urine equivalent to 2.5 μmol of creatinine was used for analysis. If the calculated urine volume exceeded 2.0 ml, only one half of the volume was used (internal standard and final volume was also cut into half) for the assay. Organic acid-ethyl acetate (6ml) was added to the urine (2ml) sample in a 10 ml glass-stoppered tube and 200μl of internal standard was added. It was incubated for 30 min at 60oC with 0.5ml of a 50g/l aqueous hydroxylamine hydrochloride solution, the pH of the mixture being adjusted to 14 with 7.5 mol/l NaOH. After cooling, the mixture was adjusted to the pH 1 with 6 mol/l HCl , supplemented with 1 g of NaCl and extracted three times with ethyl acetate portions. The combined organic phase was dried on 0.5 g of anhydrous Na2SO4 and evaporated to dryness under nitrogen at 50oC in a 1 ml PTFE-capped glass vials. To convert the compounds into trimethylsilyl derivatives, 100μl of (BSTFA-TMCS) pyridine was added to the residue and the capped vial was left overnight at room temperature [13].
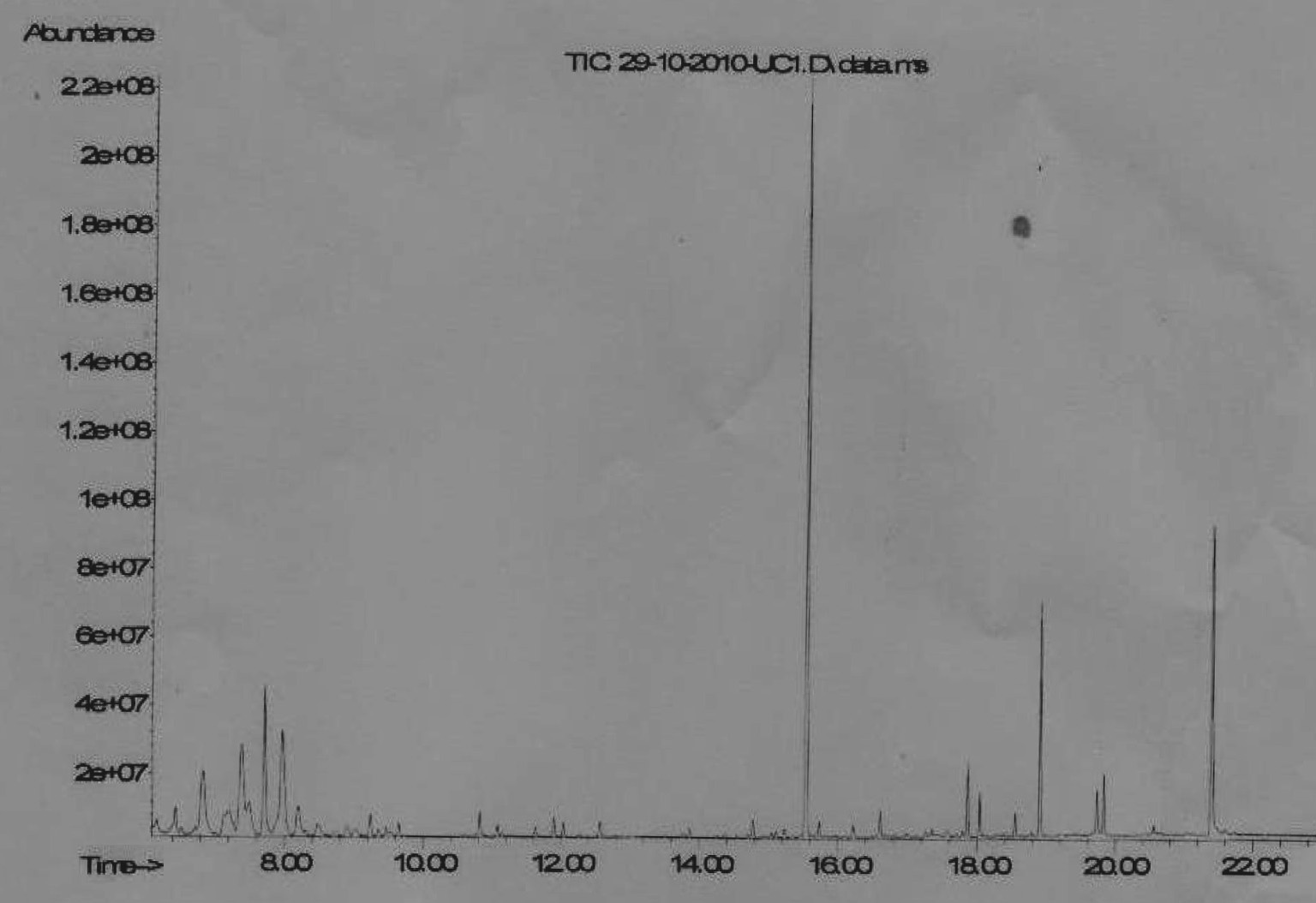
Analysis by GC-MS was done in total ion chromatogram (TIC) mode (GC-MS TIC) and SIM mode was used, one for the standard analysis of organic acids by GC-MS in total ion chromatogram (TIC) mode (GC-MS TIC) and another for the determination in selected ion monitoring (SIM) mode of a limited number of acylglycine and organic acid species (GC-MS SIM).
All analyses were done on Agilent GC-MS Chemstation System equipped with capillary gas chromatograph HP 6890 series using helium as carrier.
A derivatized standard mixture of the deutrated MMA was run prior to patient samples to determine the absolute and relative retention times. The 1μl sample was then injected and the product ion spectra monitored. Total ion current chromatograms (m/z 50-550 amu) was acquired and processed with MSD ChemStation software (Agilent Technologies).The identities of the peaks with reference spectra was confirmed by computerised comparison of the mass spectra underlying the peaks with the reference spectra of NIST mass spectra library. Quantification was done on integration of the peak area of the target ions, while the other ions as qualifying ions. The areas of the product ion peak were compared with the reference range from 20 normal urine specimens. The normal range of the upper limit was the average of ratios of the area of the analyte over the area of internal standard derived from 20 normal urines plus two standard deviations for each of the target compounds.
The MMA was identified by the qualifier and target ions and retention times [Table/Fig-1].
Statistical Analysis
The data was then analysed using SPSS 16.0 and results compared to find a correlation between levels of MMA in patients with ischemic heart failure using χ2 and Mann Whitney u tests. Comparison between variables was done by a one-way-ANOVA test.
Results
Twenty five samples were collected from patients with IHD and 20 were collected from patients with IHF. Three samples from patients with IHD and two samples from patients with IHF had to be discarded because the volume of sample was not adequate.
The demographic details as well as the results for levels of folic acid, Vit B12 and MMA in patients with IHD, IHF and control have been tabulated in [Table/Fig-2].
The values of MMA was significantly higher in patients with IHF as compared with controls (p<0.001), as well as that of patients with IHD with controls (p<0.001).
However no statistical significance was found between the levels of MMA in patients with IHF when related to severity of heart failure determined by Killip’s classification (p=0.135) Further, the duration of the disease did not have any statistical significance when compared to the level of MMA.
Discussion
Our study indicates that urinary MMA levels are significantly raised in patients with IHF as compared to IHD and normal individuals (p< 0.001). This was in accordance with the results of the study done by Seok-Min Kang et al., in Korea wherein the results showed that urinary metabolite levels of methyl malonate (p<0.001) were significantly higher in the heart failure patients along with other metabolites of Tri-carboxylic acid cycle [14]. The same is found to be true for Indian Population in our study. The mean value of MMA in patients with IHD was 126.71 (±66.3) pmol/L and those with IHF was 390.76 (±97.99) pmol/L with the difference being statistically significant (p<0.001).
It has been proposed that the failing heart and its associated state might be caused by energy starvation [15] and the failing heart is characterized by alterations in myocardial energy metabolism, including mitochondrial dysfunction and a reduction in fatty acid oxidation rate, which is partially compensated by an increase in glucose utilization. Recently much attention has been attributed to the dysfunction of mitochondrial energy metabolism, which has not only been associated with chronic failure, but acute events also. Since these involve energy pathways, it is likely that they would be deranged early in the course of the disease, may correspond with its degree and aid in monitoring and assessing prognosis. It has been shown that increased levels of organic acids, including MMA, can be cytotoxic, with effects on cells in the central nervous system, bone marrow, and kidneys [16]. It has also been shown that there is high prevalence of cardiac involvement in patients with MMA, possibly due to the inhibitory effect of methyl malonic acid on mitochondrial metabolism. Experimental studies indicate that complex II-of the mitochondrial respiratory chain is inhibited by MMA [17]. In addition MMA potently inhibits Lactate dehydrogenase (LDH) catalysed conversion of lactate to pyruvate in a purified bovine heart LDH preparation [18].
Hence, it has been suggested that patients with Heart Failure might have increased amounts of MMA due to disruption in energy metabolics, contributing to the pathophysiology and can be identified early in the disease.
However, there is paucity of data to indicate the co relation between increased levels of MMA in patients with Ischemic Heart Disease (IHD) and Ischemic Heart Failure (IHF) to support the above hypothesis. In addition, it has been recognized that a failing heart is characterized by alterations in myocardial energy metabolism, including mitochondrial dysfunction and a reduction in the fatty acid oxidation rate, which is partially compensated by an increase in glucose utilization. Alternatively, it has been postulated that a reduction in the expression of genes involved in fatty acid metabolism may be associated with cardiac hypertrophy and heart failure [19]. Indeed, several mitochondrial β-oxidative enzymes have reduced activity [18] in heart failure, and are partly responsible for the reduction in fatty acid metabolism.
MMA is the metabolite that is converted to the tricarboxylic cycle intermediate succinate with the help of the co-factor vitamin B12. It has been hypothesized that MMA induced inhibition of complex II of the mitochondrial respiratory chain leads to derangements in energy metabolism. MMA has also been reported to inhibit succinate-supported oxygen consumption by interfering with mitochondrial succinate uptake [10], Therefore it can be speculated that the accumulation of MMA would be associated with impaired tricarboxylic acid cycle flux. The results of our study are in accordance with these findings. However, since the standards used in the present study were only deutrated MMA we could not measure the variations in other metabolites of tricarboxylic acid cycle – urinary excretion of acetone, acetoacetate, acetate, citrate, succinate, 2-oxo-glutarate, and cis-aconitate. A measurement of these metabolites will further help in substantiating our hypothesis.
A significantly higher mean value of MMA in patients with IHF indicates that levels of MMA are altered early in the course of the disease. Since MMA alters pathways in the mitochondria and since these involve energy pathways, it is likely that they would be deranged early and hence MMA could serve as a potential marker in the early diagnosis of the condition.
The biggest limitation study is the small sample size; it cannot conclusively determine whether these observations are applicable in a large cohort. In the study, we could not compare the efficiency of MMA as a biomarker in comparison to the Brain Natriuretic peptide (BNP), which has been suggested to be of some value in diagnosing heart failure. However, it has been shown that BNP is more contentious in its role in helping to guide the management on of heart failure rather than the diagnosis [20]. BNP levels have been found to be measurable only after a few hours of development of clinical symptoms of heart failure like pulmonary oedema and dyspnea [21]. Hence, we suggest that it cannot be used until the disease has progressed to such a stage. In contrast, the results of the our study suggest that MMA levels are raised in IHD patients, long before the clinical signs of heart failure appear and therefore can be measured early in the disease.
A larger study comprising of cohorts with various grades of Heart failure and ischemic heart disease and a comparison of MMA with other biomarkers implicated in Heart Failure may be more suitable to answer these questions.
Chromarogram Having elevated MmaPeak.
Demographic details, levels of folic acid, Vit B12 and MMA in patients with IHD, IHF and normal individuals
| Ischemic Heart Disease | Ischemic Heart Failure | Controls |
| Age (years) | 56.10(±8.84) | 59.55(±9.06) | 58.65(±9.45) |
| Males | 13 | 11 | 11 |
| Females | 7 | 9 | 9 |
| Duration of Hospital stay (days) | 1.5 | 2.6 | 0 |
| Folic acid(ng/ml) | 3.63(±1.72) | 3.68(±1.36) | 4.03(±1.98) |
| Vit B12(pg/ml) | 392.9(±176.3) | 390.89(±190.07) | 408.13(±178.07) |
| MMA(pmol/L) | 126.71(±66.3) | 390.76 (±97.99) | 14.1pmol/L (±8.55) |
Conclusion
We measured the excretion of methyl malonic acid, in patients with ischemic heart disease and heart failure using gas chromatography mass spectrometry. It was observed that the levels of MMA were significantly higher in patients with heart failure as compared to those with Ischemic heart disease, which in turn were significantly raised in comparison to the healthy individuals. It is likely that the increased levels of MMA can be attributed to the causation or progression of the disease condition and can be used to objectively identify the disease during the early stages, before the appearance of florid signs and symptoms by which time it is the condition has progressed to an irreversible stage. MMA is likely to be deranged early during the course of failure and hence appears to be a sensitive marker for early identification
Declaration of Funding Source
There was funding received from Indian Council of Medical Research under the Short Term Studentship for this study.
[1]. VL Roger, AS Go, DM Lloyd-Jones, RJ Adams, JD Berry, TM Brown, Heart disease and stroke statistics--2011 update: a report from the American Heart Association.Circulation. 2011 123(4):e18-e209.Epub 2010/12/17 [Google Scholar]
[2]. C Berry, DR Murdoch, JJ McMurray, Economics of chronic heart failure.European journal of heart failure. 2001 3(3):283-91.Epub 2001/05/30 [Google Scholar]
[3]. PA McKee, WP Castelli, PM McNamara, WB Kannel, The natural history of congestive heart failure: the Framingham study.The New England journal of medicine. 1971 285(26):1441-46.Epub 1971/12/23 [Google Scholar]
[4]. KJ Carlson, DC Lee, AH Goroll, M Leahy, RA Johnson, An analysis of physicians’ reasons for prescribing long-term digitalis therapy in outpatients. Journal of chronic diseases. 1985 38(9):733-9.Epub 1985/01/01 [Google Scholar]
[5]. H Eriksson, K Caidahl, B Larsson, LO Ohlson, L Welin, L Wilhelmsen, Cardiac and pulmonary causes of dyspnoea--validation of a scoring test for clinical-epidemiological use: the Study of Men Born in 1913.European heart journal. 1987 8(9):1007-14.Epub 1987/09/01 [Google Scholar]
[6]. H Krum, The Task Force for the diagnosis and treatment of chronic heart failure of the European Society of Cardiology. Guidelines for the diagnosis and treatment of chronic heart failure: full text (update 2005).European heart journal. 2005 26(22):2472author reply 3-4. Epub 2005/10/06 [Google Scholar]
[7]. M Bohm, AA Voors, JM Ketelslegers, SH Schirmer, E Turgonyi, P Bramlage, Biomarkers: optimizing treatment guidance in heart failure. Clinical research in cardiology : official journal of the German Cardiac Society. 2011 100(11):973-81.Epub 2011/07/23. [Google Scholar]
[8]. LE Profitlich, B Kirmse, MP Wasserstein, GA Diaz, S Srivastava, High prevalence of structural heart disease in children with cblC-type methylmalonic aciduria and homocystinuria.Molecular genetics and metabolism. 2009 98(4):344-8.Epub2009/09/22. [Google Scholar]
[9]. T Killip, JT Kimball, Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients.The American journal of cardiology. 1967 20(4):457-64.Epub 1967/10/01 [Google Scholar]
[10]. H Blackburn, A Keys, E Simonson, P Rautaharju, S Punsar, The electrocardiogram in population studies. A classification system.Circulation. 1960 21:1160-75.Epub 1960/06/01 [Google Scholar]
[11]. S Araki, K Murata, K Yokoyama, S Yanagihara, Y Niinuma, R Yamamoto, Circadian rhythms in the urinary excretion of metals and organic substances in “healthy” men. Archives of environmental health. 1983 38(6):360-66.Epub 1983/11/01 [Google Scholar]
[12]. J Cocker, HJ Mason, ND Warren, RJ Cotton, Creatinine adjustment of biological monitoring results.Occup Med (Lond). 2011 61(5):349-53.Epub 2011/08/13 [Google Scholar]
[13]. GF Hoffmann, Selective screening for inborn errors of metabolism – past, present and future. European journal of pediatrics. 1994 153(7 Suppl 1):S2-8.Epub1994/01/01. [Google Scholar]
[14]. SM Kang, JC Park, MJ Shin, H Lee, J Oh, H Ryu do, H nuclear magnetic resonance based metabolic urinary profiling of patients with ischemic heart failure.Clin Biochem. 2011 44(4):293-9.Epub 2010/12/21 [Google Scholar]
[15]. HG DM, The chemical nature of heart failure.Ann Intern Med. 1939 12:1233-44. [Google Scholar]
[16]. ER Baumgarter, C Viardot, Long-term follow-up of 77 patients with isolated methylmalonic acidaemia.J Inherit Metab Dis. 1995 18(2):138-42. Epub 1995/01/01. [Google Scholar]
[17]. LF Pettenuzzo, C Ferreira Gda, AL Schmidt, CS Dutra-Filho, AT Wyse, M Wajner, Differential inhibitory effects of methylmalonic acid on respiratory chain complex activities in rat tissues. International journal of developmental neuroscience : the official journal of the International Society for Developmental Neuroscience. 2006 24(1):45-52.Epub 2005/12/06 [Google Scholar]
[18]. LO Saad, SR Mirandola, EN Maciel, RF Castilho, Lactate dehydrogenase activity is inhibited by methylmalonate in vitro. Neurochem Res. 2006 31(4):541-48.Epub 2006/06/08. [Google Scholar]
[19]. SD Anker, S von Haehling, Inflammatory mediators in chronic heart failure: an overview.Heart. 2004 90(4):464-70.Epub 2004/03/17. [Google Scholar]
[20]. KH Schlendorf, EK Kasper, Use of Novel and Conventional Biomarkers for Management of Patients With Heart Failure.Curr Treat Options Cardiovasc Med. 2011 Epub 2011/10/04 [Google Scholar]
[21]. GS Filippatos, SD Anker, F Kardaras, B-type natriuretic peptide serum levels in acute heart failure.Eur Heart J. 2004 25(12):1085author reply -6. Epub 2004/06/12 [Google Scholar]