Koch’s Disease Presenting as an Isolated Testicular Mass- An Unusual Occurance
Rachna Lamichaney1, Deepak Das2, Mingma Sherpa3
1Assistant Professor, Department of Pathology, Sikkim Manipal Institue of medical Sciences, Tadong, Sikkim, India.
2Assistant Professor, Department of Pathology, Sikkim Manipal Institue of medical Sciences, Tadong, Sikkim, India.
3Assistant Professor, Department of Pathology, Sikkim Manipal Institue of medical Sciences, Tadong, Sikkim, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rachna Lamichaney, Assistant Professor, Department of Pathology, Central Referral hospital, Tadong, Sikkim, India. Phone : 9002446517,
E-mail: creation_rl@hotmail.com
Isolated testicular tuberculosis (TB) is rarely seen. A 72-year-old, farmer presented with complaints of discharging sinus from scrotum along with pain and swelling. The patient had no sign of tuberculosis. On examination a hard mass arising from the left testis was noted along with a discharging fistula on the overlying scrotal skin. Chest x-ray and ultrasound examination of the abdomen were within normal limits. After assessing the testicular mass, an informed consent was taken thereafter left orchiectomy and fistulectomy performed. Histopathological examination revealed caseating granulomas along with numerous Langhan’s giant cells consistent with tuberculous orchitis. The patient received anti-TB treatment for six months. The rare involvement of testis by tuberculosis needs to be mentioned.
Caseous necrosis, Caseating granulomas, Discharging sinus, Orchitis
Case Presentation
A 72-year-old, farmer presented with complaints of discharging sinus from scrotum along with pain and swelling for the past one year. There were no history of systemic symptoms, pulmonary tuberculosis, hernia repair, epididymitis, lower urinary tract symptoms, trauma, medical treatment or infertility. Except for mild anaemia all other parameters were within normal limits. Local examination revealed a hard mass arising from the left testis with a discharging fistula on the overlying scrotal skin. Trans-illumination test of the left scrotal contents was negative. The right testis, both epididymis and the cord structures were clinically normal. Routine hematological examination showed low hemoglobin (Hb) level of 9.7 g/dl and erythrocyte sedimentation rate (ESR) of 80mm in one hour. Chest x-ray, spinal x-ray, urea, electrolyte, creatinine and liver function tests were found to be normal. Retroviral screening and venereal Disease Research Laboratory (VDRL) tests were non-reactive. After assessing the testicular mass, an informed consent was taken. Thereafter left orchiectomy and fistulectomy was performed and specimen sent for histopathological examination. We received a specimen of testis with attached skin measuring 7 x 4 x 3 cms in size. A fistulous tract measuring 1.5 x 1 cms was noted on the skin. Cut section of the specimen showed testicular parenchyma replaced by areas of chalky white areas [Table/Fig-1] .
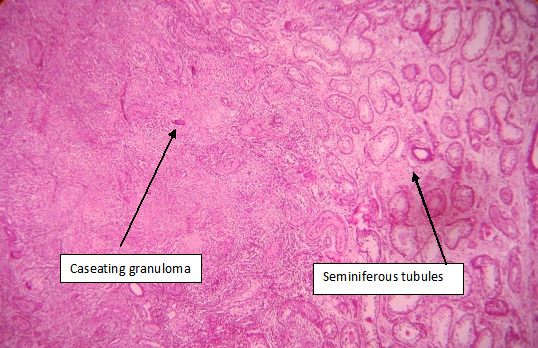
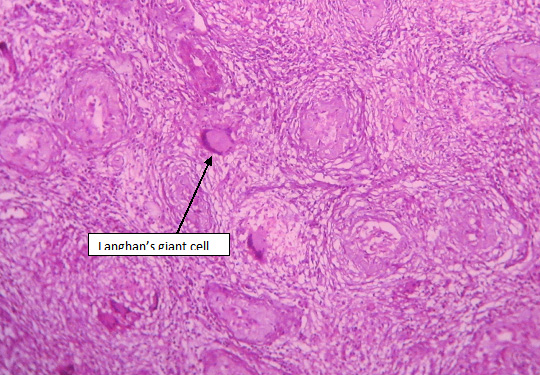
Histopathological examination showed testicular tissue, most of which were replaced by caseating granulomas composed of epithelioid histiocytes, lymphocytes, and Langhan’s multinucleated giant cells, surrounded by lymphocytes and plasma cells. The tubules were degenerated and atrophied and few showed normal spermatogenesis [Table/Fig-2a,2b].
Sections from the fistulous tract showed stratified squamous epithelium with the underlying tissue composed of caseating granulomas and Langhan’s giant cells. Ziehl Neelsen stain did not reveal any acid fast bacilli. Urine examination was negative for acid-fast bacilli. The patient was started on anti-TB therapy for six months and the response was excellent.
Discussion
Genitourinary TB is the second most common site of involvement among extra-pulmonary TB [1]. About 28% of these patients will have isolated genital involvement [2]. The most common site of genital TB is the epididymis, however isolated testicular tuberculosis is rare [3,4]. The epididymis is the commonest structure to be involved, followed by the seminal vesicles, prostate, testis, and the vas deferens. Genital TB occurs through hematogenic spread to the epididymis and prostate or through the urinary system to the prostate and canalicular spread to the seminal vesicles, deferent ducts, and epididymides[3,4]. Testicular involment is mostly due to local spread from the epididymis, retrograde seeding from the epididymis and rarely by haematogenous spread [4]. Though the exact incidence of isolated testicular tuberculosis is not known but isolated involvement of testes is rare and an unusual presentation of tuberculosis [5,6].
TB of the lower genitourinary tract can present with irritative voiding symptoms, hematuria, epididymo-orchitis, prostatitis, and fistulas [3,4,7]. The result is great thickening and the formation of a caseous mass. Caseous masses are very dense, but after a certain amount of time they generally breakdown and burst externally, resulting in tedious fistulae. Drug treatment is the first line therapy in genitourinary TB. Treatment regimens of 6 months are effective in most of the patients [7]. Isolated TB orchitis is a rare manifestation of tuberculosis [5,6]. It is difficult to diagnose TB orchitis in the absence of pulmonary or renal involvement. The most important step in diagnosing genitourinary TB is patient history. A positive culture or histological analysis of biopsy specimens possibly combined with PCR is still required in most patients for a definite diagnosis [7] . Garbyal RS et al., from India and Shugaba A.I et al., from Nigeria reported cases of isolated TB orchitis presenting with scrotal ulceration [8] .
Cut section of the gross specimen showing the testicular parenchyma replaced by chalky white areas

Photomicrograph shows caseating granulomas and testicular tissue( H&E,X100)
Photmicrograph shows testicular parenchyma replaced by caseating granuloma and atrophied seminiferous tubules (H&E, ×400)
Conclusion
Isolated testicular tuberculosis is a rare presentation and in the absence of a histologic finding, the diagnosis of TB testis may be impossible. The rarity of the disease should be taken into consideration to avoid diagnostic dilemma and help in timely diagnosis.
[1]. GJ Wise, VK Marella, Genitourinary manifestation of tuberculosis.Urol Clin North Am. 2003 30:111-21. [Google Scholar]
[2]. JS Wolf, JW McAninch, Tubercular epididymo-orchitis: Diagnosis by fine needle aspiration.J Urol. 1991 145:836-38. [Google Scholar]
[3]. GJ Wise, A Shteynshlyuger, An update on lower urinary tract tuberculosis.Curr Urol Rep. 2008 9:305-13. [Google Scholar]
[4]. BS Viswaroop, N Kekre, G Gopalakrishnan, Isolated tuberculous epididymitis: A review of forty cases. J Postgrad Med. 2005 51:109-11. [Google Scholar]
[5]. A Joual, R Rabii, H Guessous, M Benjelloun, M el Mrini, S Benjelloun, Isolated testicular tuberculosis: report of a case. Ann Urol. 2000 34:192-94. [Google Scholar]
[6]. RA Riehle, K Jayaraman, Tuberculosis of testis. Urology. 1982 20:43-46. [Google Scholar]
[7]. M Cek, S Lenk, KG Naber, MC Bishop, TE Johansen, H Botto, EAU Guidelines for the Management of Genitourinary Tuberculosis. European Urology. 2005 48:353-62. [Google Scholar]
[8]. RS Garbyal, K Sunil, Diagnosis of isolated tuberculous orchitis by fine-needle aspiration cytology.Diagn Cytopathol. 2006 34:698-700. [Google Scholar]