Effect of Four Surface Treatment Methods on the Shear Bond Strength of Resin Cement to Zirconia Ceramics- A Comparative in Vitro Study
Varsha Murthy1, Manoharan2, Balaji3, David Livingstone4
1 Assosiate Professor, Department of Prosthodontics, Indira Gandhi Institute of Dental Sciences, Pillayarkuppam, Pondicherry, India.
2 Professor, Department of Prosthodontics, Indira Gandhi Institute of Dental Sciences, Pillayarkuppam, Pondicherry, India.
3 Postgraduate Student, Department of Prosthodontics, Indira Gandhi Institute of Dental Sciences, Pillayarkuppam Pondicherry, India.
4 Assosiate Professor, Department of Prosthodontics, Indira Gandhi Institute of Dental Sciences, Pillayarkuppam, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Varsha Murthy, Assosiate Professor, Department of Prosthodontics, Indira Gandhi Institute of Dental Sciences, Pillayarkuppam,Pondicherry-607402, India. Phone : +91 7708364959, E-mail : drvarshamurthy@gmail.com
Background: Improving the retention of zirconia-based ceramics is desirable in order to avoid the failure of crowns and fixed partial dentures .This can be achieved by creating micromechanical retention using surface treatments. Therefore, it becomes necessary to constantly compare and re-evaluate the influence of different surface treatment methods on the bond strength .
Aim: To evaluate the effect of four different surface treatments on shear bond strength between zirconia surface and resin cements.
Settings and Design: Observational study.
Materials and Methods: Twenty five zirconia plate samples were prepared based on ISO standards and were divided into five groups and each group was subjected to following five different surface treatments : no treatment, sandblasting with 110 μm alumina, sandblasting with 250 μm alumina, acid etching with 9.6% hydrofluoric acid and laser radiation on the surface. All the samples were surface disinfected and were embedded in blocks of autopolymerising resin to check shear bond strength on the universal testing machine. Statistical analysis used-data was analyzed using one-way ANOVA and a Post Hoc Bonferroni test.
Results: Analysis of the data showed that the highest shear bond strength values were obtained with laser treatment (18.120 ± 0.8159 Mpa). The lowest values were obtained with control group (9.166 ± 0.569 Mpa). Laser treatment increased the shear bond strength values significantly (p<0.05).
Conclusion: Surface treatments increased the bond strength between zirconia and resin cement and carbon dioxide laser could be an effective surface treatment for increasing bond strength.
Airborne particle abrasion, Carbon dioxide laser, Hf acid etching, Laser etching, Shear bond strength, Surface treatment
Introduction
Success of an all ceramic restorations is highly dependent on achieving a bond of the resin with the underlying tooth structure as well as with the restoration. Bonding is required for improving the retention, marginal adaptation, fracture resistance and bond strength of restorations [1]. Bonding also increases surface energy, surface area for bonding, and wettability [2]. During the fabrication or milling of the ceramic, sufficient bond strength values are not generated, therefore it requires surface pretreatment [3]. Bond strength can be improved by the presence of micromechanical retention, as the creation of roughened ceramic surfaces may allow resin cement to penetrate and flow into such microretentions, thereby creating a stronger micromechanical interlock [4]. There are several tests for assessment of bond strength of resin-based materials to dental ceramics namely shear, tensile, and microtensile tests. These test methods are based on the application of a load in order to generate stress at the adhesive joints until failure occurs [5].
There are various surface treatment methods namely grinding, abrasion with diamond rotary instruments, airborne particle abrasion, silicate coating, acid etching, coupling with silane and combinations of any of these methods [4,5]. Airborne particle abrasion with aluminium oxide abrasive particles has been identified as an effective means of achieving a stable, durable bond for zirconia ceramics [6]. Acid etching on a zirconia ceramic surface has been found to produce a significant difference in the surface roughness [4]. A few studies have also been performed on the carbon dioxide laser treatment of zirconium oxide ceramics [5,7] .
Considering the various materials and techniques available, influence of surface treatment on bond strength with commonly available modalities like sandblasting, acid etching, and laser treatment was planned. So the first NULL hypothesis for the present study was that the type of surface treatment does not significantly affect the shear bond strength of zirconia to tooth structure .The second NULL hypothesis was that the carbon di oxide laser does not have a determinant effect and could not be an effective surface treatment modality to increase bond strength.
Materials and Methods
Twenty five samples of zirconia, CEREC (Cortis-YZ, Sirona Dental GmbH Bensheim, Germany) were sliced off from the blocks using the diamond disc under running water and assorted into groups and sintered for 8 hours [Table/Fig-1] following manufacturer’s instructions(www.sirona.com/en/products/digital-dentistry/newproducts/information). Then the samples were trimmed and prepared to size of 16 x 11 mm uniformly following ISO -682, 2008 guidelines [8] for sample preparation. All the samples were then surface disinfected with isopropyl alcohol (Surfacept, Minntech Corporation Minneapolis, USA), smoothened with emery paper under running water and then cleaned in ultrasonic cleanser.

Subsequently the samples are divided into five Groups, Group A samples were left untreated and served as control group for the study. Group B samples were sandblasted with 110 μm alumina (KoroxR110 microns Bego, Bremen, Germany) at 35 psi from a distance of approximately 10mm for 15 secs. Group C samples were sandblasted with 250 μm alumina (KoroxR110 microns Bego, Bremen, Germany) at 35 psi from a distance of approximately 10mm for 15 seconds. Group D samples were acid etched with 9.6% hydrofluoric acid (Ultradent porcelain etch 9.6%, Ultradent Products, South Jordan) for 30 sec and then air dried. Group E samples were treated with surgical carbon dioxide laser radiation (Smart US 20D, Carbon Dioxide laser, Deka Floresence, Italy) on the surface. Laser energy was delivered in a pulse mode with wavelength of 10.6 mm, a pulse repetition rate of 1000 Hertz and pulse duration of 160 ms at an average power setting of 3 w, delivered perpendicular to the surface in non-contact mode 1mm away from the surface.
All the samples were once again surface disinfected with isopropyl alcohol to remove off debris and were embedded in blocks of autopolymerising resin to facilitate clamping on the universal testing machine (Mechanical Krystal Elmec, Ichkalkaranji, Maharashtra, India) [Table/Fig-2]. Resin cement blocks of 0.5 mm were embedded over treated surface using LEDition (LED lamp LUX-V Guilin woodpecker medical instrumentation co.Guangxi, China) with Intensity of 600- 800W/cm2 for 20 sec following manufacturer’s instructions. The samples were loaded in the universal testing machine and pulled apart after clamping in the opposite jaws [Table/Fig-2,3] to find the shear bond strength. A thin wire of 0.2 mm diameter was looped around and a shear force was applied at cross head speed of 1mm/minute. The shear bond strength was calculated in Megapascal by dividing Failure load (N) by area of composite resin (πr2). Results obtained were tabulated and subjected for statistical analysis. Means and standard deviations of the bond strength were calculated and mean values were compared by one-way ANOVA using Statistical software program, Statistical Package for the Social Sciences (SPSS, Version 19; IBM SPSS Inc., Chicago, Illinois). Multiple comparisons test were done using Bonferroni post hoc test.
Universal testing machine

Samples clamped in the UTM

Results
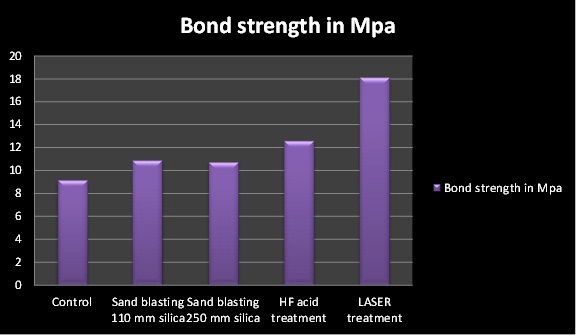
[Table/Fig-4] yielded the highest shear bond strength values for lasers(18.120 ± 0.8159 Mpa) and lowest values were obtained for control group (9.166 ± 0.569 Mpa) [Table/Fig-4].One-way ANNOVA [Table/Fig-5] yielded p-value <0.05 which shows that the results were significant [Table/Fig-5]. There were no significant differences in p-value between control, sandblasting with 110 μm and sandblasting with 250 μm. Laser showed significant differences from all other groups (p < 0.05). On analysis of Bonferroni post hoc test results [Table/Fig-6], it was found that on comparing other groups with control, both HF and laser groups had better bond strength. When both air abrasion group was compared with other groups only laser treatment group had statistically significant values. HF group when compared with other groups was found to be better similar to control group. Finally, when laser group was compared with the rest it was found to have statistically significant values than any other group.
Mean and Standard Deviation of shear bond strength of Control and Experimental Groups
| Group | Treatment | Mean | SD |
|---|
| A | Control | 9.1660 | .56968 |
| B | Sand blasting 110 mm silica | 10.890 | .85591 |
| C | Sand blasting 250 mm silica | 10.732 | 1.17238 |
| D | HF acid treatment | 12.6060 | .53069 |
| E | LASER treatment | 18.120 | .8159 |
| SD – Standard Deviation |
Results of one- way ANOVA test
| Sum of squres | Df | Mean square | F | P |
|---|
| Groups | | 4 | | | |
| Within groups | 13.68 | 20 | 69.238 | 101.18 | .000 |
| Total | 290.63 | 24 | .684 | | |
P<0.05 indicates statistically significant differences, Df – degrees of freedom, F- F statistic, p- statistical significance
Results of Post Hoc Bonferroni test
| (I) Distribution of Group | (J) Distribution of Group | Mean Difference (I-J) | Std. Error | P |
|---|
| Control | Sand blasting with 110 mm silica | -1.72800* | .52318 | .036 |
| Sand blasting with 250 mm silica | -1.56600 | .52318 | .072 |
| Hydrofluoric acid | -3.44000* | .52318 | <0.001 |
| CO2 laser treatment | -9.54600* | .52318 | <0.001 |
| Sand blasting with 110 mm silica | Control | 1.72800* | .52318 | .036 |
| Sand blasting with 250 mm silica | .16200 | .52318 | 1.000 |
| Hydrofluoric acid | -1.71200* | .52318 | .038 |
| CO2 laser treatment | -7.81800* | .52318 | <0.001 |
| Sand blasting with 250 mm silica | Control | 1.56600 | .52318 | .072 |
| Sand blasting with 110 mm silica | -.16200 | .52318 | 1.000 |
| Hydrofluoric acid | -1.87400* | .52318 | .019 |
| CO2 laser treatment | -7.98000* | .52318 | <0.001 |
| Hydrofluoric acid | Control | 3.44000* | .52318 | .000 |
| Sand blasting with 110 mm silica | 1.71200* | .52318 | .038 |
| Sand blasting with 250 mm silica | 1.87400* | .52318 | .019 |
| CO2 laser treatment | -6.10600* | .52318 | <0.001 |
| CO2 laser treatment | Control | 9.54600* | .52318 | <0.001 |
| Sand blasting with 110 mm silica | 7.81800* | .52318 | <0.001 |
| Sand blasting with 250 mm silica | 7.98000* | .52318 | <0.001 |
| Hydrofluoric acid | 6.10600* | .52318 | <0.001 |
*. The mean difference is significant at the 0.05 level., P- statistical significance
Bar diagram showing shear bond strength of different groups
Discussion
The data in the present study rejected the first null hypothesis, as the bond strength between zirconia and resin cement was affected by the type of surface treatment similar to some previous studies [9]. The present study also rejected the second null hypothesis and carbon di oxide laser was found to improve the shear bond strength between zirconia and tooth structure. Several tests can be used for assessing bond strength namely, shear, tensile and microtensile tests. Tension tests are more appropriate for assessing adhesive characteristics of the resin cements to the ceramics which is not applicable in the present situation since our study aimed to determine the effect of surface pretreatments on bond strength. Microtensile test was not appropriate for the present study because multiple specimens from the same block leads to difficulties in statistical interpretation of the results. In the present study, shear bond has been used for comparison, as it is commonly used, is fast, easy to perform and also reflects the clinical situation [3]. There was no significant difference in the shear bond strength between the control, sandblasting and acid etching groups except in the laser group [Table/Fig-7].
Some studies have shown that some conventional and self-adhesive resin cements presented low bond strength when applied to intact surfaces of Zirconium oxide ceramics [10]. Improving the retention of zirconia-based ceramics is desirable in order to avoid the decementation phenomena [11,12]. Loss of crown retention was found to be the second leading cause of failure of crowns and fixed partial dentures [13]. Uncemented restorations have been listed as the third leading cause of prosthetic replacement with failures occurring in varying periods of 1 to 38 month [11,12] and 5.8 y of service [14]. Failures are usually reported as being within the substrate(cohesive),between the adhesive and substrate(adhesive),within the restorative material (cohesive),or mixed.
Air abrasion was proposed in order to increase the resin bond strength to zirconia [15] and the cement to ceramic bonding [16]. However it was found that particle abrasion alone, slightly roughens the zirconia surface [17] but does not always provide reliable resin bond strength [2,15]. Different sizes of aluminium oxide particles, between 50 and 110 mm, are generally used for sandblasting [15]. However, it was found that different size of particles and the application time may induce discrepancies in the achieved results, as excessively high pressure during blasting may initiate phase transition, and expedite the formation of micro-cracks, thus reducing the mechanical properties of zirconia [18]. In the present study particle size of alumina did not show any difference (p>0.05).
Acid etching on a zirconia ceramic surface produced a significant difference in the surface roughness [4]. Contrary to it was also found that etching with hydrofluoric acid has no influence on zirconia ceramics, as no micro-grooves are created, due to the low amount of glass phase [19,20] , and its susceptibility to hydrolytic degradation [15,21]. However, the present study showed better effectiveness of HF group similar to Ural et al., [22].
Carbon dioxide lasers have been previously used to etch zirconia bioceramic implants to enhance their osseointegration [23] and improve adhesion of orthodontic metal brackets to feldspathic porcelain. It has been reported that carbon di oxide laser etching produces a lower bond strength when compared with chemical etching [24] and is less effective for improving Zirconia bonding as compared to other lasers [25–27]. Although, there have been negative results for lasers, but in some studies [22] carbon di oxide laser enhanced micromechanical retention and improved the bond strength of resin cement on zirconia ceramic when compared with other surface treatments similar to our study.
An effective bonding between the tooth structure and zirconia would prevent the removal of more tooth structure to create retention and resistance form for the restoration. In addition, it would aid in retention of teeth with short or reduced clinical crowns [28]. However, clinically there are many other factors which lead to the dislodgement of crown. In the present study surface analysis tests using scanning electron microscopy, or x-ray diffraction method were not done which may be considered as a limitation of the study. Our aim however was to determine the bond strength in this study and not to assess the surface characteristics.
Conclusion
Within the limitations of the present study, it was possible to conclude that the surface treatments increased the bond strength and the type of surface treatment significantly affected the shear bond strength of zirconia to tooth structure. Carbon dioxide laser proved to increase bond strength. A chairside system of carbon di oxide laser may be effective in improving the shear bond strength between a zirconia ceramic and tooth structure.
P<0.05 indicates statistically significant differences, Df – degrees of freedom, F- F statistic, p- statistical significance
*. The mean difference is significant at the 0.05 level., P- statistical significance
[1]. Burke FJ, Fleming GJ, Nathanson D, Marquis PM, Are adhesive technologies needed to support ceramics? An assessment of the current evidenceJ Adhes Dent 2002 4:7-22. [Google Scholar]
[2]. Kim BK, Bae HE, Shim JS, Lee KW, The influence of ceramic surface treatments on the tensile bond strength of composite resin to all-ceramic coping materialsJ Prosthet Dent 2005 94:357-62. [Google Scholar]
[3]. Ozcan M, Vallittu PK, Effect of surface conditioning methods on the bond strength of luting cement to ceramicsDent Mater 2003 19:725-31. [Google Scholar]
[4]. Chaiyabutr Y, McGowan S, Phillips KM, Kois JC, Giordano RA, The effect of hydrofluoric acid surface treatment and bond strength of a zirconia veneering ceramicJ Prosthet Dent 2008 100:194-202. [Google Scholar]
[5]. Ersu B, Yuzugullu B, Ruya Yazici A, Canay S, Surface roughness and bond strengths of glass-infiltrated alumina ceramics prepared using various surface treatmentsJ Dent 2009 37:848-56. [Google Scholar]
[6]. Phark JH, Duarte S, Blatz M, Sadan A, An in vitro evaluation of the long-term resin bond to a new densely sintered high-purity zirconium-oxide ceramic surfaceJ Prosthet Dent 2009 101:29-38. [Google Scholar]
[7]. Convissar RA, Goldstein EE, A combined carbon dioxide/erbium laser for soft and hard tissue proceduresDent Today 2001 20:66-71. [Google Scholar]
[8]. Triwatana P, Srinuan P, Mongkol K, Comparison of two fracture toughness methods using a glass infiltrated and a zirconia dental ceramicJ Adv Prosthodont 2013 5:36-43. [Google Scholar]
[9]. Miragayaa L, Maia LC, Sabrosac CE, Goes MF, Da Silva EM, Evaluation of Self-adhesive Resin Cement Bond Strength to Yttria-stabilized Zirconia Ceramic (Y-TZP) Using Four Surface TreatmentsJ Adhes Dent 2011 13:473-80. [Google Scholar]
[10]. Aboushelib MN, Matinlinna JP, Salameh Z, Ounsi H, Innovations in bonding to zirconia-based materials: Part IDent Mater 2008 24:1268-72. [Google Scholar]
[11]. Schley JS, Heussen N, Reich S, Fischer J, Haselhuhn K, Wolfart S, Survival probability of zirconia-based fixed dental prostheses up to 5 year: a systematic review of the literatureEur J Oral Sci 2010 118:443-50. [Google Scholar]
[12]. Beuer F, Stimmelmayr M, Gernet W, Edelhoff D, Guh JF, Naumann M, Prospective study of zirconia-based restorations: 3-year clinical resultsQuintessence Int 2010 41:631-36. [Google Scholar]
[13]. Schwartz NL, Whitsett LD, Berry TG, Stewart JL, Unserviceable crowns and fixed partia l dentures: life-span and causes for loss of serviceabilityJ Am Dent Assoc 1970 81:1395-401. [Google Scholar]
[14]. Walton JN, Gardner FM, Agar JR, A survey of crown and fixed partial denture failures: length of service and reasons for replacementJ Prosthet Dent 1986 56:416-21. [Google Scholar]
[15]. Kern M, Wegner SM, Bonding to zirconia ceramic: Adhesion methods and their durabilityDent Mater 1998 14:64-71. [Google Scholar]
[16]. Dino Re, Augusti D, Augusti G, Giovannetti A, Early Bond Strength to Low-pressure Sandblasted Zirconia: Evaluation of Self-adhesive CementThe Eur Jrnl of Esthetic Dent 2012 7:164-75. [Google Scholar]
[17]. Borges GA, Spohr AM, de Goes MF, Sobrinho LC, Chan DC, Effect of etching and airborne particle abrasion on the microstructure of different dental ceramicsJ Prosthet Dent 2003 89:479-88. [Google Scholar]
[18]. Zhang Y, Lawn BR, Malament KA, Van Thompson P, Rekow ED, Damage accumulation and fatigue life of particle-abraded ceramicsInt J Prosthodont 2006 19:442-48. [Google Scholar]
[19]. Ozcan M, Alkumru HN, Gemalmaz D, The effect of surface treatment on the shear bond strength of luting cement to a glass-infiltrated alumina ceramicInt J Prosthodont 2001 14:335-39. [Google Scholar]
[20]. Blatz MB, Chiche G, Holst S, Sadan A, Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconiaQuintessence Int 2007 38:745-53. [Google Scholar]
[21]. Valandro LF, Ozcan M, Amaral R, Leite FP, Bottino MA, Microtensile bond strength of a resin cement to silica-coated and silanized In-Ceram Zirconia before and after agingInt J Prosthodont 2007 20:70-72. [Google Scholar]
[22]. Ural C, kulunk T, Kulunk S, Kurt M, The Effect of Laser Treatment on Bonding Between Zirconia Ceramic Surface and Resin CementActa Odontologica Scandinavica 2010 68:354-59. [Google Scholar]
[23]. Hao L, Lawrence J, Chian KS, Effects of Carbon dioxide laser irradiation on the surface properties of magnesia partially stabilized zirconia (MgO-PSZ) bioceramic and the subsequent improvements in human osteoblast cell adhesionJ Biomater Appl 2004 19:81-105. [Google Scholar]
[24]. Obata A, Tsumura T, Niwa K, Ashizawa Y, Deguchi T, Ito M, Super pulse Carbon dioxide laser for bracket bonding and debondingEur J Orthod 1999 21:193-98. [Google Scholar]
[25]. Akin H, Ozkurt Z, Kirmali O, Kazazoglu E, Ozdemir AK, Shear bond strength of resin cement to Zirconia ceramic after aluminium oxide sandblasting and various laser treatmentsPhotomed Laser Surg 2011 29:797-802. [Google Scholar]
[26]. Akin H, Tugut F, Akin GE, Guney U, Mutaf B, Effect of Er: YAG laser application on the shear bond strength and microleakage between resin cements and Y-TZP ceramicsLasers Med Sci 2012 27:333-38. [Google Scholar]
[27]. Paranhos MPG, Burnett LH, Magne P, Effect of Nd: YAG laser and Carbon dioxide laser treatment on the resin bond strength to zirconia ceramicQuintessence Int 2011 42:79-89. [Google Scholar]
[28]. Foxton RM, Cavalcanti AN, Nakajima M, Pilecki P, Sherriff M, Melo L, Watson T, Durability of Resin Cement Bond to Aluminium Oxide and Zirconia Ceramics after Air Abrasion and Laser TreatmentJrnl of Prosthod 2011 20:84-92. [Google Scholar]