Modern concept of osseous surgery considers the importance of conserving the alveolar bone and emphasizes more on the significance of reconstructive osseous surgery. In 1970’s Schallhorn [1] stated that, when attempting new attachment by flap procedure, bone graft should be inserted into infrabony defects in order to attain bone regeneration.
The quest for an ideal graft material led to the development of alloplastic graft materials which act as a scaffold over which new bone forms. The current scientific interest in alloplastic replacement is focused primarily on hydroxyapatite, because of its close chemical and structural resemblance to the bone mineral.
As a part of the development of bioceramics for hard tissue applications, the Biomedical technology wing of Sri Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, has developed hydroxyapatite in powder and granule forms. The hydroxyapatite powder (Chitra powder) is synthetic and non-porous having a particle size in the range of 100 to 300 microns. The Chitra granules is porous hydroxyapatite ceramic granule material derived from Chitra powder have a particle size of 0.5 to 1 mm with a pore size of 100-200 microns. Chitra granule resulted a better regeneration of alveolar bone and periodontal fibers as compared to Chitra powder and OsteoGenR (HA Resorb)TM in experimental osseous defects on Newzealand dwarf rabbits [4].
Human histologic analysis is the gold standard for determining the true potential of any graft material to regenerate the periodontium. The histological evaluation is not possible in man because of the need to retrieve teeth and their surrounding periodontium in large blocks for histological analysis. Advantage of experimentation in animal system is the possibility of creating paired defects of equal size.
The periodontal defects were produced by acute defect model. Advantages of the acute defect model include cost effectiveness, reduced experimental time and ensure standardization of defect size. According to Selvig KA [5] once detoxification has been successfully accomplished, the conditions of postsurgical healing will be the same regardless of past history of the root surface. This establishes a justification for studying the regenerative potential in the acute defect model.
The present study was to evaluate histologically and histometrically the efficacy of Chitra granules in the regeneration of alveolar bone and to compare it with that of OsteoGenR (HA Resorb)TM in iatrogenically created alveolar bone defects in dogs.
Materials and Methods
Study Design: Four healthy young adult mongrel dogs consisting of two females and two males were used for the study. The ethical committee clearance for the study was obtained. They were under quarantine for a period of 21 days after procurement, during which period they were dewormed and vaccinated against diseases. The animals were divided randomly into two groups of two animals: Group One and Group Two depending on the observation period of three months and six months duration respectively. Same animals were used as control and test. Each dog had four implantation sites; two on the right side (mesial aspect of right 3rd and 4th premolars) and two on the left side (mesial aspect of the 3rd and 4th premolars on the lower jaw). On the right side, Chitra granules was implanted and on the left side, OsteoGenR (HA Resorb)TM was implanted. The mongrel dogs selected for the study were small, easy to handle and extremely cooperative during experimentation. Since, it has an extensive rima oris which provides adequate site exposure during surgery.
Animal care and maintenance: Pre anaesthetic medication was carried out using Atrophine sulphate 0.5 to 1mg administered intramuscularly to reduce the excessive salivary flow during the course of the procedure. Diazepam 10mg was administered intramuscularly to exert potent tranquilising, muscle relaxant and anticonvulsant effects.
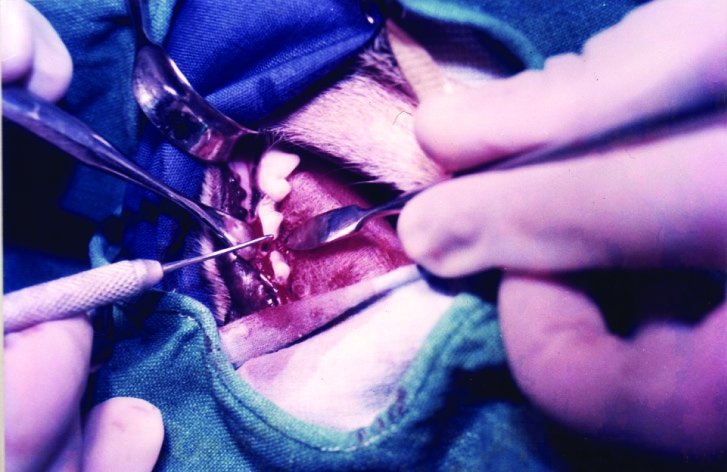
Presurgical Preparation: The dog was covered with sterile drapes only to expose the oral cavity. Any bacterial contamination of iatrogenic origin was avoided by using autoclaved instruments, wearing clean sterile face mask, cap, gown and gloves. Mouth of the animal was opened wide with a mouth gag placed on the canines.
Incisions and Elevation of Flap: A crevicular incision was placed around the 2nd, 3rd, 4th premolars and the first molar. Then a mucoperiosteal flap was elevated to expose the alveolar bone.
Preparation of Surgical Defect: Three walled intrabony defects of 2 to 3mm in dimension buccolingually and mesiodistally of about 4.5 to 5mm cervicoapically were created on the mesial aspect of 3rd and 4th premolars using a No.801 straight fissure bur in a slow speed contra angled hand piece with continuous saline irrigation. The root surface was curetted using a Gracey’s curette to remove the remaining periodontal ligament fibers. A notch, serving as landmark for measurements in histological sections, was prepared in mesial root surface at the level of the surgically reduced bone crest. The surgical defect was thoroughly irrigated with saline to remove the loose osseous fragments. The size of the defect was then confirmed using a graduated periodontal probe [Table/Fig-1]. Complete haemostasis was obtained before placing the graft material.
Williams periodontal probe showing the depth of osseous defect.
Placement of the Bone Graft Materials: The autoclaved bone graft material was dispensed into a sterile dapendish. It was moistened with 1 to 2 drops of saline to obtain a putty consistency and excess moisture was removed using a sterile filter paper. The material was then carried to the defect using an amalgam carrier and packed into the defect using a plastic filling instrument. Then, the mucoperiosteal flap was returned to the preoperative position and secured using 4-0 braided silk sutures. Direct loop sutures were placed so as to attain complete defect closure.
Post-Surgical Care: The animals were put under antibiotic coverage with ampicillin cloxacillin 250mg, twice daily by intramuscular injection for five days. For alleviating inflammation and pain, diclofenac sodium 25mg was given twice daily. The sutures were removed on the seventh postoperative day under sedation, and the surgical area was irrigated with 0.2% chlorhexidine gluconate solution.
Post-Surgical Procedures: Two dogs of Group One were sacrificed at the end of three months and the other two (Group Two) at the end of six months by euthanasia using intravenous injection of an overdose of thiopentone sodium, an ultra-short acting barbiturate. It resulted in marked cardiac and respiratory depression with cardiac arrest in 1 to 2 min. After confirming euthanasia, the mandible was dissected with soft tissues.
Fixation: The specimen was immersed in 10% buffered formalin soon after retrieval and allowed to be fixed for 48 h. The jaw was sectioned using diamond cutter into blocks corresponding to the bone graft sites. Block of each bone graft site included the bone graft with part of tooth on either side. All the blocks from Group One (three months) animals were subjected to decalcification. Whereas in Group Two (six months) animals, the blocks corresponding to third premolar teeth were decalcified and blocks corresponding to fourth premolar were processed by undecalcification.
Demineralization Tissue Processing: For decalcification, the blocks were placed in separate beakers containing decalcifying solution{10% formic acid (100m) and formalin (5ml)}. This was continuously agitated using a magnetic stirrer. The decalcifying solution was changed at least every 2 to 3 d. It took about 15-20 d for the complete decalcification to occur. The completion of decalcification was determined by adding a chemical ammonium oxalate, to the decalcifying solution. The decalcified block was subjected to dehydration in ascending grades of alcohol 50% (1 h), 70% (1 h), 80% (1 h), 90% (1 h), 100% (2 h) each with two changes. The dehydrated tissue was immersed in a clearing agent - chloroform (2 h) in a series of 3 changes. The cleared tissue was immersed in paraffin wax at 56°c for 2 h with 2 changes. This infiltrated tissue was positioned in a mould filled with embedding medium-paraffin to make a block. Multiple serial sections of 5μm thickness were cut in the mesio-distal plane using a leica microtome. These sections were placed on a microscopic slide and stained by standard haematoxylin and eosin technique and observed under light microscope.
Non Demineralized Tissue Processing: The specimen was subjected to dehydration in ascending grades of alcohol 70%, 80%, 90% and 100% each for 4 h with 2 changes. It was infiltrated in alcohol and acetone mixture at 1:1 concentration for 2 h and then in 100% alcohol for 4 d. This was treated with polymethylmethacrylate I for 4 d and polymethymethacrylate II for 2 d and polymerized with accelerator benzyl peroxide in vacuum to make a block. Isomet diamond cutter was used to make sections of 150 μm thick in a mesio-distal plane. These sections were ground and polished to 100 μm thickness and stained with steventhal’s blue.
Statistical Analysis
The data was analysed using statistical package Graph pad Software. Comparison of the hard and soft tissue parameters in the two groups was done using the Wilcoxan (Man Whitney), two tailed t-test. A p-value less than 0.05 were considered significant.
Results
The postoperative healing was clinically uneventful in all the four dogs with no local or systemic reactions. The gingiva appeared healthy and showed no clinical features of redness, ulceration or abscess formation.
Histologic evaluation at 3 mnth - in OsteoGenR (HA Resorb)TM sites
Maturing bone was present over the site implanted with bone graft, fibroblastic connective tissue as well as new woven osteogenic bone with osteocytes and osteoblasts was observed between the bone graft particles [Table/Fig-2]. Woven bone was in direct contact with bone graft particles, as well as with the apical border of the cavity. Fibrovascular tissue was observed between the maturing bone and tooth [Table/Fig-3]. A narrow layer of acellular cementum was also observed. Amounts of bone formation in the two animals were almost similar.
OsteoGen® (HA Resorb) TM at 3 months: Photomicrograph showing the surgical defect on the mesial aspect of a premolar with A. Implant spaces B. New bone. In decalcified section (Magnification 18 X)
OsteoGen® (HA Resorb) TM at 3 months: Photomicrograph showing A. Implant spaces B. fibrous connective tissue C. New bone D. Osteocytes in decalcified sections (Magnification 180X)

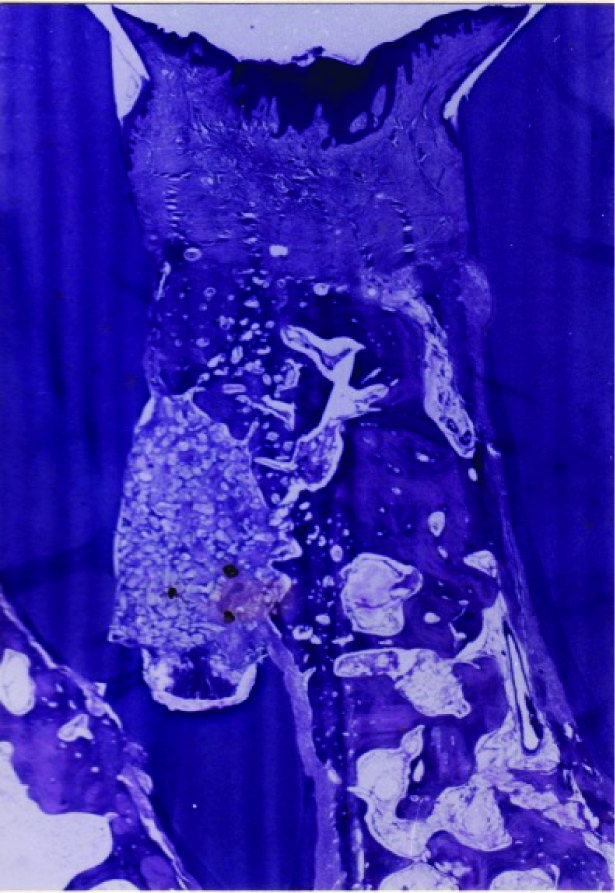
Histologic evaluation at 3 months – in Chitra granule sites: Bonegraft particles were identified as voids during decalcification. These appeared much larger in size than with OsteoGenR (HA Resorb)TM and were present in a well circumscribed area along the mesial aspect of the tooth. Fibroblastic connective tissue with numerous areas of osteogenic tissue was also observed. Woven bone was observed between these voids and bone was found mainly in the lower third of the cavity and areas of continuation with underlying alveolar bone were noted [Table/Fig-4]. New maturing bone was also seen over the bone graft area with immature periodontal ligamentous tissue adjacent to the tooth surface.
Chitra Granules at 3 months: Photomicrograph showing A. Implant spaces B. Fibrous connective tissue C. New bone D. Osteocytes in decalcified sections (Magnification 180 X)

Histologic evaluation of undecalcified sections of OsteoGenR (HA Resorb)TM sites at 6 month: Mature woven and lamellar bone with osteocytes and marrow spaces was observed to fill the cavity. Numerous bone graft granules of various sizes and shapes were present in the cavity, with mature bone enveloping some particles and fibroblastic connective tissue growing in between other particles [Table/Fig-5].
OsteoGen® (HA Resorb) TM at 6 months: Photomicrograph showing A. Implant spaces B. New bone C. Marrow D. Osteocytes in non decalcified sections. (Magnification 360X)

Histologic evaluation of undecalcified sections of Chitra Granules at 6 months: The cavity was completely filled by mature bone. Occasionally, Chitra granule particles were embedded in mature osteogenic tissue, whereas others were surrounded by fibrous connective tissue. Numerous chitra granules were present in the coronal portion of the cavity [Table/Fig-6]. Most of these granules were surrounded by fibrous connective tissue, though new bone appears to be in close contact with occasional Chitra granules.
Chitra Granules at 6 months: Photomicrograph showing A. Implant spaces B. New bone C. Marrow D. Osteocytes in non decalcified sections (Magnification 360X)

Decalcified Section: Over a period of six months, cavities filled with Chitra granules as well as those filled with OsteoGenR (HA Resorb)TM, were healed well with advanced osteogenesis. Mature woven and lamellar bone with osteocytes and marrow was also observed. There appeared to be a direct continuity between surrounding alveolar bone and bone formed in the cavity. The healing patterns appeared to be similar around both types of bone graft particles.
Histometric Evaluation
Histometric evaluation was planned by placing a notch on the root surface at the surgically reduced bone height. However, this notch could not be located in some histologic sections. Thus, in the 6 month sections an attempt was made to measure the height of new bone formed, by taking measurements from gingival margin to lower level of residual bone graft apically and gingival margin to coronal level of new bone. New bone formed was measured by subtracting the distance between gingival margin to coronal level of new bone, from the distance between gingival margin to lower level of residual bone graft.
In the control group treated with OsteoGenR (HA Resorb)TM, the mean amount of new bone formed was 6493.5 microns at 6 months, which was statistically significant (p=0.5000) [Table/Fig-7]. In the test group treated by Chitra granules, the amount of new bone formed was 6087.5 microns at six months postoperatively, and was statistically significant (p = 0.5000) [Table/Fig-8]. Although, there was no statistically significant difference in the bone formed between control and test groups, the mean values showed that amount of new bone formed with OsteoGenR (HA Resorb)TM was slightly more than that obtained by Chitra granules [Table/Fig-9].
Amount of new bone formation in control [ osteogenr (HA Resorb)TM] group by histometric evaluation in microns
| Animal No | Gingival margin to coronal level of new bone | Gingival margin to apical level of residual implants | Amount of new bone |
|---|
| 1 | 1838 | 6550 | 4712 |
| 2 | 1200 | 9475 | 8275 |
| Mean | 1519 | 8012.5 | 6493.5 |
Amount of new bone formation in test [Chitra Granules] group by histometric evaluation in microns
| Animal No | Gingival margin to coronal level of new bone | Gingival margin to apical level of residual implants | Amount of new bone |
|---|
| 1 | 2075 | 9100 | 7025 |
| 2 | 3400 | 8550 | 5150 |
| Mean | 2737.5 | 8825 | 6087.5 |
Comparison of new bone formation between the control [Osteogen(HA Resorb)TM] and test [Chitra Granules] groups by histometric evaluation in microns
| OsteoGenR (HA Resorb)TM | Chitra granules | p-value |
|---|
| Amount of new bone formed | 6493.5 ± 2519.42 | 6087.5 ± 1325.83 | 1.000 |
Discussion
In the present study, three walled intrabony defects were created surgically on the mesial aspects of third and fourth premolars. Similar three walled intrabony osseous defects were also carried out by Nery EB et al., [6,7] . All the treatment sites healed uneventfully with no clinical evidence of inflammatory response to the hydroxyapatite bone graft particles. Similar biocompatible nontoxic nature of hydroxyapatite has been reported by Kenney et al.,[8] (1985) and Krejci CB et al.,[9].
At three months, decalcified section showed no evidence of inflammation associated with both bone graft materials. Kenny et al., [10] also noted similar findings in three month specimens of human subjects. Whereas Stahl and Froum [11] noticed inflammation within the marginal gingival region, but there was no significant inflammatory infiltrate in the bone graft sites.
In the present study, healing in most specimens observed was by the formation of a connective tissue attachment. In a study by West and Brustein [12], noticed formation of long junctional epithelium in dog model treated by porous hydroxyapatite. Carranza et al., [13] noticed junctional epithelium extending below the level of porous hydroxyapatite. The present study showed advanced osteogenesis with both bone graft materials. Similar osteogenesis was also observed by West & Brustein [12] in dog model, Ettel et al., [14] in rhesus monkeys, and Kenney et al., [10], Carranza et al., [13] Stahl and Froum [11] in human subjects using porous hydroxyapatite.
Maturing bone was also present coronally over the bone graft area in the present study for both the bone graft materials at three months was similar to the study by Stahl and Froum [11]. Ettel et al., [14] also noted the bone apposition coronal to many of the implant particles in the 10 to 12 week specimens in rhesus monkeys. The bone guiding or osteoconductive properties of the calcium phosphate have been discussed by (Kenney et al., [10], Stahl and Froum [11], Ettel et al., [14]. Histologic evidence of bone deposition either in direct contact with the calcium phosphate implant Nery E et al., [15] or within the connective tissue adjacent to the implant Levin et al., [16], has been suggested to be due to the presence of the bone graft material.
In the present study, a narrow band of a cellular cementum was observed in association with OsteoGenR (HA Resorb)TM in one implanted site. No cementum formation was noted with Chitra granules. Formation of new cementum with porous implant materials was also reported by Carranza et al., [13] in human specimens and Ettel et al., [14] in rhesus monkeys. In the present study, the formation of immature, nonaligned periodontal ligament fibers were evident with both the bone graft materials at three months. In undecalcified sections at six months, some of the graft particles were present in the gingival connective tissue, above the coronal aspect of new bone. These particles were surrounded by fibrous connective tissue, few of them were in direct contact with new bone which was similar to the results of the study by Ettel et al., [14].
Histometric evaluation by using the notch placed at the surgically reduced bone height as a reference point was not possible in this study. Because in thicker sections, the difference in block orientation may produce greater variation. In the present study, the thicknesses of the sections were 150 μm, which were ground and polished to 100 μm thicknesses. Similarly, thicker sections were used in a study by Ettel et al., [14] on rhesus monkeys using porous hydroxyapatite. Since the reference notch was not identifiable in all sections in the present study, the amount of new bone formed was measured by subtracting the distance between gingival margin to coronal level of new bone from the distance between gingival margin to lower level of residual bone graft material seen apically. Thus the mean amount of new bone formed with OsteoGenR (HA Resorb)TM was 6493.5 microns, and with Chitra granules it was 6087.5 microns at 6 months. There was no statistically significant difference between these two groups. But the mean values showed a better mean amount of bone formed with OsteoGenR (HA Resorb)TM.
Conclusion
Histological study showed similar healing pattern with both the types of bone graft materials. Maturing bone was observed at three months with both OsteoGenR (HA Resorb)TM and Chitra granules. It also showed advanced osteogenesis at six months, and the number of bone graft granules were less when compared to three months for both the bone graft materials. However, histological evaluation for longer period is necessary to determine the time taken for complete replacement of the bone graft materials with new bone.