Background: Cardiac adversity is by far the commonest cause of mortality in patients with diabetes. Cardiac involvement in diabetes commonly manifest as coronary artery disease (CAD). Definitive diagnosis,precise assessment and anatomic severity of CAD requires invasive diagnostic modality like coronary angiography.
Aims and Objectives: To study angiographic extents, type of vessels, number of vessels, severity involving coronary artery and its branches in patients with acute coronary syndrome(ACS).Compare the same in diabetics and non diabetics with ACS.
Materials and Methods: Hundred patients with ACS,50 diabetics and 50 nondiabetics admitted in Bapuji Hospital ICCU attached to J.J.M. Medical College were selected randomly during a period of approximately one and half years formed the study group. RBS, FBS was done in all 100 pateints, HbA1c in all diabetics. All subjects with ACS were taken up for coronary angiography.
Statistical Analysis: Chi-square test was used to determine any significant difference between two groups. p-value of less than 0.05 was considered significant.
Results: In our study 22 (44%) out of 50 diabetic patients had triple or multi-vessel disease compared to 8 (16%) out of 50 non diabetics. Hundred patients with ACS, number of vessels involved were 199, of which 61.3% in diabetics and 38.6% in non diabetics, 23(46%) of 50 diabetic patients required CABG as treatment outcome. HbA1c levels of >8.5%, 69.2% had triple / multi vessel disease and 19 (73.1%) of 23 patients who had to undergo CABG had HbA1c levels >8.5%, 24% of diabetics were in third decade, 40% were in fourth decade as compared to 10% and 26% of non-diabetics of similar age group.
Interpretation and Conclusion: This study showed that ACS in diabetic patients presented much earlier in life, the severity and extent of CAD and incidence of triple/multi vessel disease was significantly high in diabetics when compared to nondiabetics with ACS. Diabetics with high HbA1c had more number of coronary vessel involvement and the mode of treatment required in them was CABG.
Introduction
Diabetes mellitus is one of the commonest disease worldwide ranking next to cardiovascular disorder. It is estimated that, around 100 million populations is affected with diabetes worldwide [1]. Diabetes is a disease of complications, both acute and chronic. Cardiac affliction is by far the commonest cause of mortality in patients with diabetes [2]. Dyslipidemia is observed in practically all patients of type-2 diabetes mellitus and every high level of cholesterol in diabetics has 2-3 times higher CAD risk than non-diabetic individuals.
Cardiac involvement in diabetes commonly manifest as coronary artery disease (CAD) and less commonly as diabetic cardiomyopathy and cardiac autonomic neuropathy [3]. CAD alone accounts for the major chunk of mortality in diabetes. Accelerated and greater frequency of CAD has been widely documented in hospital, autopsy, and epidemiological as well as longitudinal studies in several populations.
Diabetes has become predominantly a disease of the cardiovascular system and hence cardio-daibetology [4] is fast emerging as subspecialty throughout the world to tackle the menace of cardiac related mortality and morbidity in diabetes particularly in NIDDM.
Although, CAD and diabetes mellitus have been recognized as distinct entities for many decades, but their correlation was established only in 1870 after the work of Seegen J, Der. who emphasized higher incidence and mortality of CAD among diabetics [1].
Although the patients history, physical examination and non-invasive techniques like resting ECG, holter monitoring, stress test (TMT), stress echocardiography, stress thallium imaging are valuable in establishing the diagnosis of myocardial ischemia in diabetes, the definitive diagnosis of CAHD, its precise assessment and anatomic severity requires invasive diagnostic modality like coronary angiography.
A breakthrough in the field of cardiology came with the introduction of “interventional cardiology” which serves as a diagnostic as well as therapeutic aid in the management of coronary artery disease [5].
Coronary angiography or arteriography remains the ‘Gold-standard’ technique for diagnosing and evaluating coronary artery disease.
Hence, this study titled comparitive angiographic profile in diabetics and non-diabetic patients with acute coronary syndrome, was undertaken and an attempt was made to find, how ACS in diabetics differ from that of non-diabetics, with special interest on their angiographic profile.
Materials and Methods
The present study is a cross-sectional study. This study was conducted on 100 patients with ACS among which 50 patients who are diabetics and other 50 patients who are non-diabetics admitted in Bapuji Hospital ICCU, attached to JJM Medical College and in S.S. Institute Of Medical Sciences, Davangere, India.
Patients who matched the inclusion and exclusion criteria were selected randomly during period of approximately one and a half years formed the study group.
Inclusion Criteria
• Group 1(Diabetic): Previously known diabetic or first time detected diabetic by American Diabetes Association (ADA) criteria presenting with ACS.
• Group 2(Non-Diabetic): Cases presenting with acute coronary syndrome that is non-diabetic or not fulfilling ADA criteria.
Exclusion Criteria
Patients having impaired fasting glucose presenting with ACS.
Following investigations were done after selection: Fasting blood glucose levels by collection method, Random blood glucose levels, HbA1c in diabetic and newly detected diabetes mellitus patients, Complete haemogram, Blood urea, Serum creatinine, Lipid profile, Cardiac enzymes-CPK-MB/LDH/SGOT, ECG, 2D ECHO, Treadmill Test (TMT) and Coronary Angiogram. Patients coming with complaints of acute chest pain, breathlessness were diagnosed to have ACS based on ECG and cardiac enzymes.
RBS, FBS were done for all the patients. HbA1c was sent in patients whose RBS or FBS was in higher range to confirm newly detected diabetes and in all diabetic patients to know the glycemic control. Patients with ACS, both diabetics and non diabetics were treated and once they were stabilized were taken up for coronary angiography which was performed by the standard Judkin’s technique after adequate preparation.
The indication for performing coronary angiography was unstable angina NSTEMI and STEMI and post infarct angina.
Severity of lesions as noted in angiography were graded as follows:
Grade 0: No disease
Grade 1: Intimal disease <50% stenosis
Grade 2: 50-69% stenosis
Grade 3: 70-95% stenosis
Grade 4: 96-99% stenosis
Grade 5: Total occlusion
Coronary artery narrowing of more than or equal to 70% was considered as significant stenosis.
HbA1c was done in all the diabetics’ patients and in newly detected T2DM patients. We classified the diabetic patients with their HbA1c control as <7 is good control, 7 – 8.5 is fair control and >8.5 poor control.
Depending on the angiographic findings, further treatment was planned whether the patient requires medical line of management, PTCA or CABG. Angiographic parameters and further treatment required were compared between diabetic patients and non diabetic patients with ACS.
Statistical Analysis
Categorical data was expressed as number and percentages. Chi-square test was used to determine any significant difference between two groups. A p-value of less than 0.05 was considered for statistical significance.
Chi-square test:
O: Observed frequency
E: Expected frequency
Fisher’s exact probability test.
F = PA or PB
PA = Probability A
PB = Probability B
Results
Distribution of Diabetics and Non Diabetics with ACS in Various Age Groups
Peak incidence of ACS in diabetics was in the third and fourth decade as compared to fifth and sixth decade in non-diabetics.
Diabetic patients presented much earlier with ACS as early as third decade of life compared to non-diabetics.
Among diabetics 24% of the cases were in their third decade and 40% of the cases were in the fourth decade as compared to 10% and 26% of non-diabetics of similar age group.
Sex Incidence
In our study the incidence of ACS in males was 68% in diabetics and 80% in non-diabetics. In females the incidence of ACS was 32% in diabetics and 20% in non-diabetics.
So the risk of developing ACS in females was more in diabetics compared to non-diabetics.
Duration of Diabetes
In our study the majority of patients (48%) had a relatively shorter duration of diabetes between 5-10 years.
18% of the patients were newly detected and diagnosed as T2DM and 34% had longer duration of diabetes of >10 years.
The incidence of Triple /multi vessel disease in diabetics was much higher (44%) compared to non-diabetics (16%).
The incidence of double vessel disease in diabetics was slightly higher (26%) compared to non-diabetics (20%).
Single vessel disease was much higher in non-diabetics (64%) [Table/Fig-1].
Out of 100 patients of both diabetics and non diabetics with ACS, total number of vessels involved are 199, out of which 61.3% are involved in diabetics where as 38.6% in non-diabetics which is significant suggesting patients with diabetes having more number of vessels involved.
Significant difference present in the involvement of LMCA in diabetics (7.5%) compared to non diabetics (1%). The commonest vessel involved in both the groups was LAD, 23.1% in diabetes and 21.1% in non diabetic [Table/Fig-2].
Severity of stenosis ranging from grade 4-5 was noticed in 52% of the diabetics compared to 18% in non-diabetics[Table/Fig-3].
Total occlusion or grade 5 stenosis was significantly high in diabetics as compared to non-diabetics.
The incidence of SVD and DVD was much higher in diabetic patients whose duration of disease as 5-10 years.
Incidence of triple / multi vessel disease was significantly higher with the duration of diabetes >10 years (94.1%) [Table/Fig-4]
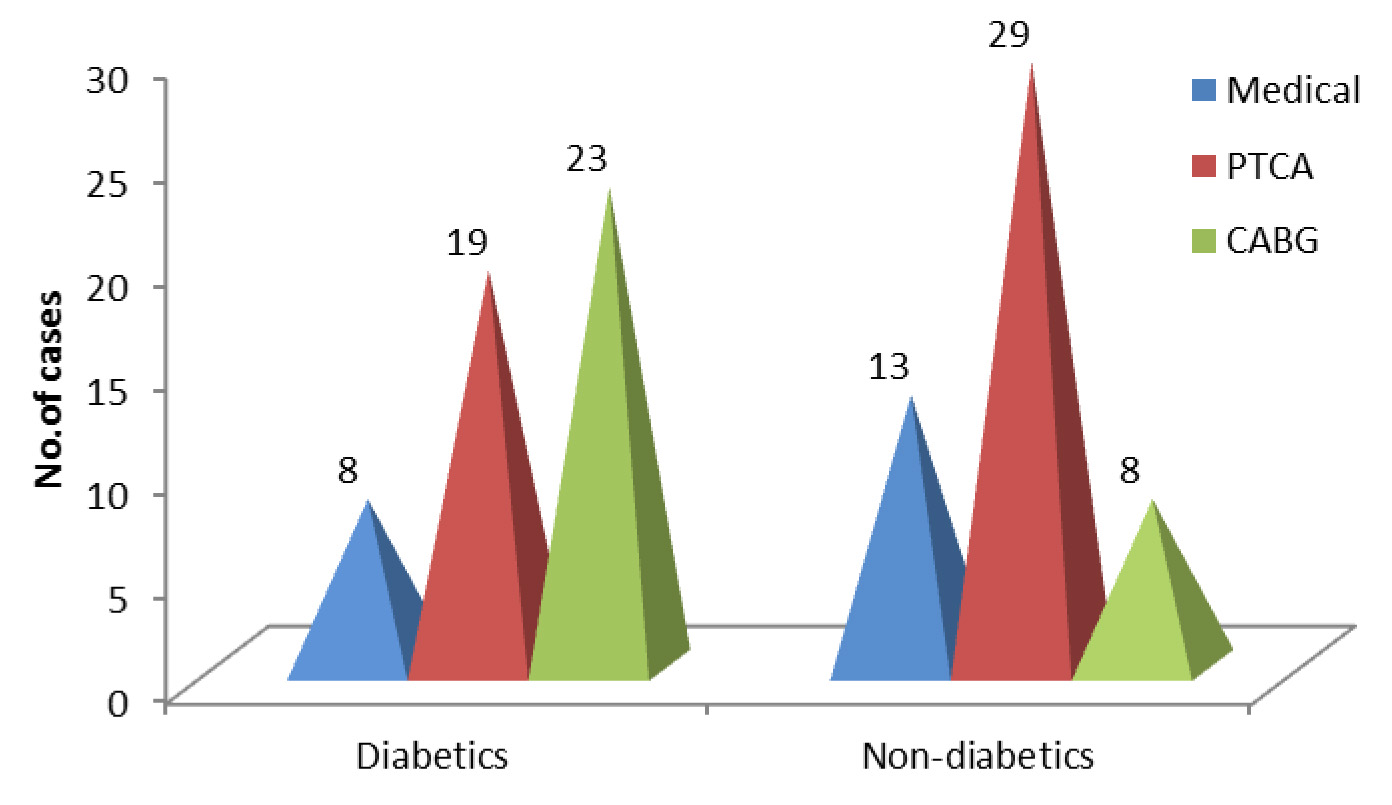
Majority of diabetic patients (46%) require CABG as treatment option compared to 16% of non-diabetics.
PTCA is preferred in 58% of non-diabetics compared to 38% of diabetics.
Medical line of management was required in 26% of non diabetics where as 16% in diabetics [Table/Fig-5] .
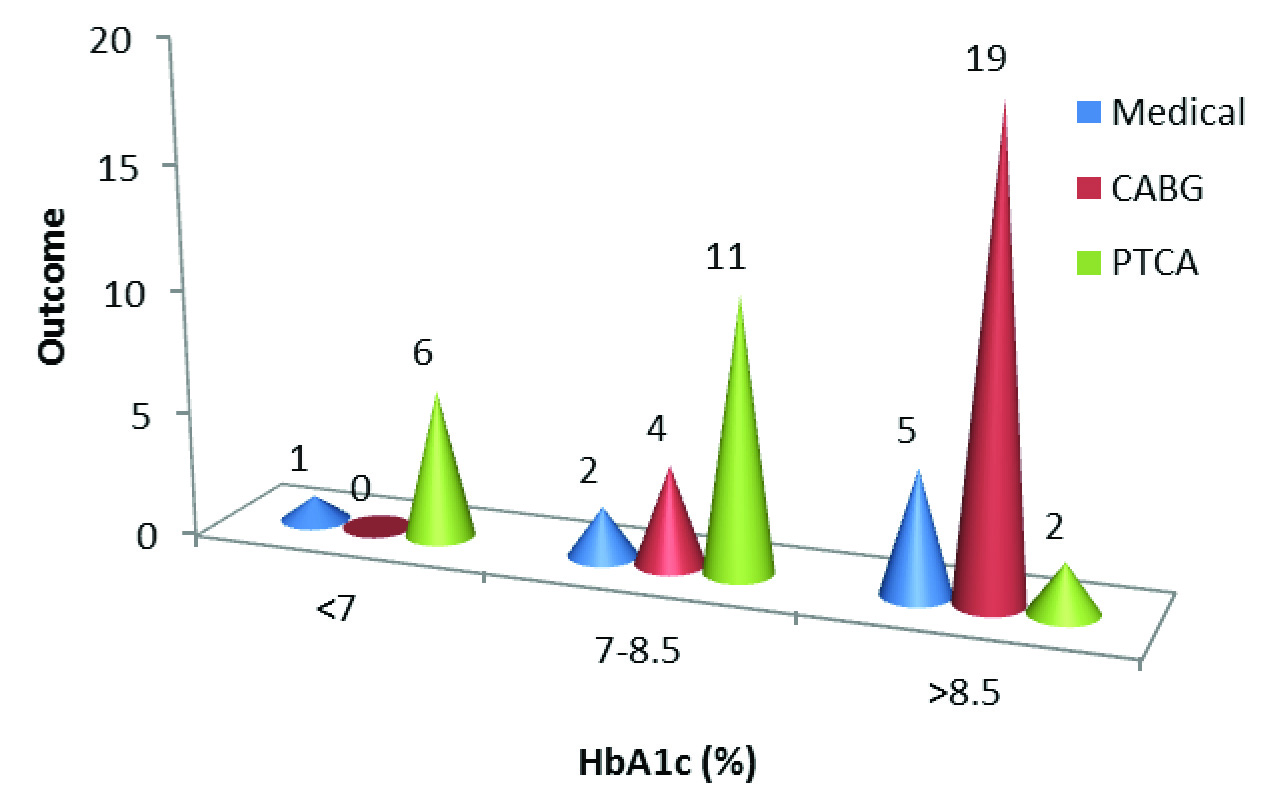
In patients with HbA1c of <7 (good control), 85.7% had single vessel involvement and no triple vessel disease. Whereas patients with HbA1c >8.5 (poor control) had 69.2% of triple/ multiple vessel disease and 7.7% of single vessel involvement [Table/Fig-6].
Suggesting with good control of HbA1c there is reduction in number of vessels involved.
In our study patients with poor control of HbA1c > 8.5, 73.1% of them had to undergo CABG where as with good control of HbA1c <7, 85.7% of them underwent PTCA [Table/Fig-7] .
Discussion
The present study of 50 diabetic patients and 50 non-diabetic patients with CAD were analysed with special emphasis laid on the coronary angiographic findings in acute coronary syndrome (ACS). Our results were compared with similar studies done earlier
Age Incidence
In the present study it was seen that the peak incidence of ACS in diabetics with poor glycemic control was in the third and fourth decade as compared to fifth and sixth decade in non-diabetics. This finding correlated with DiabCare Asia--India Study: diabetes care in India–current status [6].
Sex Incidence
In our study the incidence of ACS in males was 68% in diabetics and 80% in non-diabetics. In females the incidence of ACS was 32% in diabetics and 20% in non-diabetics. The risk of developing ACS in females was more in diabetics compared to non diabetics [7]. This risk was doubled when the female patients had features of syndrome X.
Severity of Cad with Duration of Diabetes
In our study, 48% of diabetic patient had a relatively shorter duration of diabetes between 5-10 years and 34% had longer duration of diabetes of >10 years. Incidence of triple / multi vessel disease was significantly higher with the duration of diabetes >10 years (94.1%). This findings correlates with the other study by Fox CS et al., [8], showing the risk of CHD was 1.38 times higher for each 10 year increase in the duration of diabetes (95% CI, 0.99 – 1.92).
Significance HbA1c Levels
In our study, diabetic patients with poor glycemic control, i.e. HbA1c >8.5%, 69.2% of them had triple vessel disease and 23.1% had double vessel disease suggesting poor glycemic control with higher HbA1c levels having more number of coronary vessels and more the severity of the stenosis. This finding correlates with other study conducted by Tahir Saleem et al., showed HbA1C (r=0.427, p=0.001) and duration of DM (r=0.362, p=0.004) had a positive linear correlation with the Gensini score. Multiple regression analysis showed HbA1C to be an independent factor that influenced the Gensini score (p=0.021) [9]. In our study, diabetic patients with higher HbA1c levels, 73.1% of them had CABG as treatment outcome. Suggesting prevalence of elevated glycosylated haemoglobin levels in patients undergoing coronary artery bypass surgery. This findings correlates with other study conducted by Milo Engoren et al., showed prevalence of elevated haemoglobin levels in patients undergoing coronary artery bypass surgery is high and routine measurement should be done to permit institution of lifestyle modifications and medication changes that decrease complications and death from diabetes mellitus [10].
Angiographic Profile
In our study, coronary angiography revealed that the incidence of multivessel disease in diabetics was much higher (50%) compared to non-diabetics which was only 16%. This finding correlates with the other study by Singh RB,Niaz MA., [11], showed higher incidence of MVD in diabetics (57.3%) compared to 41.3% in non-diabetics. In another study conducted at CMC Vellore also showed that MVD was more common in diabetics (87.5% Vs 79.6%) in two separate groups of 516 diabetic and non-diabetic patients [12]. In a study by Henry et al., showed patients with diabetes had moderate (50% to75% narrowing) stenosis much more frequently than patients without diabetes (50.6 versus 30.3%, p < 0.001). Moreover, diabetes mellitus was an independent risk factor for moderate stenosis. The lesions were more frequently located on distal arteries, more frequently had a pattern of three-vessel disease, and had a trend toward more diffuse disease [13]. Sousa JM et al., showed severe three-vessel disease was significantly more frequent in diabetic patients (28% x 10%), as well as totally occluded vessels: 51 (23%) x 54 (14.3%), p < 0.005. Additionally, ejection fraction <50% was more common in diabetic patients confirming the diffuse pattern of atherosclerotic disease in diabetic patients [14].
The commonest vessel involved in our study was LAD in both the groups followed by Lcx and RCA. This finding is similar to other various studies. In our study, the number of patients having total occlusion was 20% in diabetics and 6% in non diabetics. This finding is statistically significant (p<0.01). Hence the extent and severity of coronary artery disease was significantly high in diabetic patients with acute coronary syndrome when compared to non diabetic with acute coronary syndrome.
This finding were similar in other studies like Mahdi Mossavi et al., [15], Uddin SN et al., [16], Nichoils et al., [17], Jamal S. Rana et al., [18], where they found the angiographic extent and severity of coronary artery disease was high in diabetic patients with acute coronary syndromes.
No.of vessels involved by angiography,
| Diabetics | Non-Diabetics |
| Single vessel disease | 15 (30%) | 32 (64%) |
| Double vessel disease | 13 (26%) | 10 (20%) |
| Triple /Multi vessel disease | 22 (44%) | 8 (16%) |
| Total | 50 | 50 |
X2 = 13.07, P=0.014, Significant
| Diabetics (n=50) | Non-diabetics (n=50) | X2 | P-value |
| LMCA | 15 (7.5%) | 3 (1%) | 4.05 | 0.044 Sig |
| LAD | 46(23.1%) | 42 (21.1%) | 5.43 | 0.0197Sig |
| LCx | 33 (27.04%) | 14 (7.03%) | 2.06 | 0.151, NS |
| RCA | 28 (14.07%) | 18 (9.04%) | 0 | 1,NS |
| Total | 122 (61.3%) | 77 (38.6%) | X2=8.28 | P=0.0405, Sig |
| Diabetics | Non-diabetics |
| Grade 1 | 8 (16%) | 18 (36%) |
| Grade 2 | 8 (16%) | 16 (32%) |
| Grade 3 | 8 (16%) | 7 (14%) |
| Grade 4 | 16 (32%) | 6 (12%) |
| Grade 5 | 10 (20%) | 3 (6%) |
| Total | 50 | 50 |
X2 = 14.89, p=0.0049 Significant
Duration of diabetes with no. of vessels involvedfisher’s exact probability test p=0.00001, HS
| 5-10 years | >10 years |
| Single vessel disease | 10 (41.6%) | 0 |
| Double vessel disease | 9 (37.5%) | 1 (5.8%) |
| Triple / Multi vessel disease | 5 (20.8%) | 16 (94.1%) |
| Total | 24 | 17 |
Significance of Hba1c Control with Number of Vessels Involved
| HbA1c (%) | SVD | DVD | TVD/MVD |
| <7 | 6 (85.7%) | 1 (14.3%) | 0 |
| 7-8.5 | 7 (41.2%) | 6 (35.3%) | 4 (23.5%) |
| >8.5 | 2 (7.7%) | 6 (23.1%) | 18 (69.2%) |
| Total | X2=17.519 p<0.0001df=2HS | X2=1.372 p=0.502df=2NS | X2=15.108p=0.001df=2Sig |
Significance of Hba1c Control with Treatment Outcome
Conclusion
The severity and extent of CAD in diabetics was more compared to non-diabetics. Involvement of LMCA was significantly high and severity of stenosis and total occlusion of vessels were more commonly seen in diabetic patients. The incidence of triple vessel or multivessel disease was significantly higher with the duration of diabetes more than 10 years. Majority of the diabetic patients with ACS require CABG as the main mode of treatment. Patients with poor glycemic control with elevated levels of HbA1c had diffuse pattern of atherosclerotic disease and high levels of HbA1c correlated with patients undergoing CABG. Hence, routine HbA1c levels to be measured and adoption of lifestyle changes and medications that decrease cardiovascular complications and morbidity from diabetes mellitus.
X
2 = 13.07, P=0.014, Significant
X
2 = 14.89, p=0.0049 Significant
[1]. DM Nathan, J Meigs, De Singer, The epidemiology of cardiovascular disease in type-2 diabetes mellitus: How Sweat it is…. Or is it.The Lancet 1997 350(S1):S14-8. [Google Scholar]
[2]. BB Thripaty, Complications of diabetes :API text book of medicineBr Dent J 2001 6th EditionAssociation of Physicians of India:1005-07pp. [Google Scholar]
[3]. Rlos Maerrano, Cardiac complications in diabetes:World book of diabetes in practice2:169pp [Google Scholar]
[4]. PC Manoria, The concpet of cardio-diabetology.: post-graduate medicine APIJ Am Dent Assoc 1998 :363-68. [Google Scholar]
[5]. Baim Donald S., Grossman William, Coronary angiography : Grossman’s cardiac catheterization, angiography and interventions: 2000 6PhiladelphiaLippincott Williams & Wilkins:211-12pp. [Google Scholar]
[6]. BS Raheja, A Kapur, Diabetes care Asia-India Study: diabetes care in India- Current status. J.Assoc Physicians India. 2001 49(7):717-22. [Google Scholar]
[7]. MJ Garcia, PM McNamara, Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow-up study.Diabetes 1974 23(2):105-11. [Google Scholar]
[8]. CS Fox, L Sullivan, Sr D’Agostino RB, PW Wilson, Framingham heart study. The significant effect of diabetes duration on coronaryheart disease mortality : the Framingham Heart study.Diabetes Care. 2004 2793:704-08. [Google Scholar]
[9]. T Saleem, KH Mohammad, Association of glycosylated haemoglobin level and diabetes mellitus duration with the severity of coronary artery disease.Diabetes and Vascular Disease Research. 2008 5(3):184-89. [Google Scholar]
[10]. MilloEngoren Habbi Robert H., Zacharias Anvar, Schwann Thomas A, Riordan Christopher J., The prevalence of elevated haemoglobin A1c in patients undergoing coronary artery bypass surgery.J Cardiothoracic Surgery. 2008 3:63 [Google Scholar]
[11]. RB Singh, MA Niaz, Coronary risk factors in Indians.The Lancet 1995 346:778-79. [Google Scholar]
[12]. S Krishnaswami, G Joseph, E Punnoose, ST Chandy, Coronary angiographic findings in patients with diabetes: an exercise in cardiovascular epidemiology. The Journal of the Association of Physicians of India 1996 44(3):169-71. [Google Scholar]
[13]. P Henry, S Makowski, P Richard, F Beverelli, Increased incidence of moderate stenosis among patients with diabetes: substrate for myocardial infarction?Am Heart J. 1997 134(6):1037-43. [Google Scholar]
[14]. JM Sousa, JL Herrman, M Teodoro, Comparison of coronary angiography findings in diabetic and non-diabetic women with non-ST-segment-elevation acute coronary syndrome.Arq Bras Cardiol. 2006 86(2):150-55. [Google Scholar]
[15]. Mossavi Mahdi, Nematipour Ebrahim, Mehrpooya Maryam, Comparison of extent of coronary artery disease in angiography of diabetics and non-diabetics.Iranian Heart Journal. 2006 7(4)PhiladelphiaLippincott Williams & Wilkins:37-42. [Google Scholar]
[16]. SN Uddin, F Malik, MA Bari, NI Siddiqui, GK Khan, S Rahman, Angiographic severity and extent of coronary artery disease in patients with type 2 diabetes mellitus. MMJ 2005 14(1):32-37. [Google Scholar]
[17]. SJ Nichoils, EM Tuzev, S Kalidindi, Effect of diabetes on progression of coronary atherosclerosis and arterial remodeling; a pooled analysis of intravascular ultrasound trials. J Am Coll Cardiol. 2008 52:255-62. [Google Scholar]
[18]. Rana Jamal S., Dunning Allison, Achenbach Stephen, Mallah Mouaz-Al, Budoff Mathew J., Cademartiri Filippo, Difference in prevalence, extent, severity and prognosis of coronary artery disease among patients with and without diabetes undergoing coronary computed tomography angiography. Care.diabetes_ Journals.Org / content/ early 2012/06. [Google Scholar]