Clinicopathological Study of Prostatic Biopsies
A. Josephine1
1Assistant Professor, Department of Pathology, Sree Balaji Medical College & Hospital, No: 7, Works Road Chromepet, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. A. Josephine, Assistant Professor, Department of Pathology, Sree Balaji Medical College & Hospital, No: 7, Works Road Chromepet, Chennai - 600044, India.
Introduction: Prostatism is a common malady in the geriatric age group. Benign prostatic hyperplasia and Carcinoma of the prostate are increasingly frequent with advancing age. The aim of the present study is to study the spectrum of prostatic lesions among the biopsies received in a rural hospital.
Materials and Methods: One hundred and six cases of prostatic biopsies received in the Department of Pathology, Rajah Muthiah Medical College and Hospital – Annamalai University were included in the present study. There were 44 needle biopsies and 62 TURP specimens. All the specimens were fixed in 10% neutral buffered formalin and 5μ sections were stained with Hematoxylin and Eosin stain (H & E stain). Relevant clinical data including age, the presenting complaints and S.PSA values in suspected cases of carcinoma prostate were recorded.
Results: Among the 106 biopsies received, 79 (74.52%) cases were of Benign prostatic hyperplasia, two cases (1.89%) were Prostatic intraepithelial neoplasia and 25 cases (23.58%) were Carcinoma of Prostate. Prostatitis was the most common associated lesion in cases of benign prostatic hyperplasia presenting in 25.31% patients. Among the Carcinoma patients, 20 cases (80%) were of Adenocarcinoma of prostate and 5 cases (20%) were Small cell carcinoma of prostate. Both Benign prostatic hyperplasia and Carcinoma prostate were common in the seventh decade. Most common clinical presentation was difficulty in micturition. Most common histological type of Carcinoma prostate was Adenocarcinoma. Serum PSA estimation was done in 49 cases of prostate biopsies. Elevations of serum PSA levels were noted in both BPH and Carcinoma prostate patients.Eight cases of BPH, had serum PSA values in the range of 0-4ng/ml. Six cases of Carcinoma prostate ,had serum PSA values in the range of >80 ng/ml.
Conclusion: Benign prostatic hyperplasia is the most commonly encountered prostatic lesion. Although, investigations like transrectal ultrasonogram and serum PSA estimation aids in diagnosis, a definitive diagnosis of benign and malignant lesions of prostate can be made by histopathological study of prostatic biopsies.
Benign prostatic hyperplasia, Prostatic intraepithelial neoplasia
Introduction
Benign Prostatic hyperplasia (BPH) and carcinoma prostate are increasingly frequent with advancing age. BPH is the most common urological problem of ageing men and is a complex disease from the etiological and pathogenisis point of view [1]. Both BPH & Carcinoma of prostate display a parallel increase in prevalance with patient’s age. Both require androgens for growth and both respond to anti-androgen treatment regimen. Both present with obstructive urinary symptoms. The combination of Digital rectal examination [DRE], Trans Rectal Ultrasonogram which is an indispensable tool to guide a needle biopsy and to estimate the volume of prostate gland for calculating PSA density [2] and Serum PSA estimation, supplemented with biopsy procedures represents a powerful diagnostic tool in the diagnosis of both benign and malignant prostatic lesions. Moreover very few studies have been done in India regarding prostatic lesions. This prompted us to investigate the clinicopathological correlation of prostatic biopsies with special reference to serum Prostate specific antigen(PSA) levels.
Materials and Methods
One hundred and six prostatic biopsies received during the period between May 2008 and April 2011 in the Department of Pathology, Raja Muthiah Medical College and Hospital were included in the present study.
The biopsy material included transuretheral resection of prostate (TURP) specimens, needle biopsies, both trucut and core needle biopsies. There were 44 needle biopsies and 62 TURP specimens. All the specimens were fixed in 10% neutral buffered formalin and 5μ sections were stained with hematoxylin and eosin stain (H & E stain).
Relevant clinical data including age, the presenting complaints and S.PSA values in selected biopsy cases were recorded.
Results and Observation
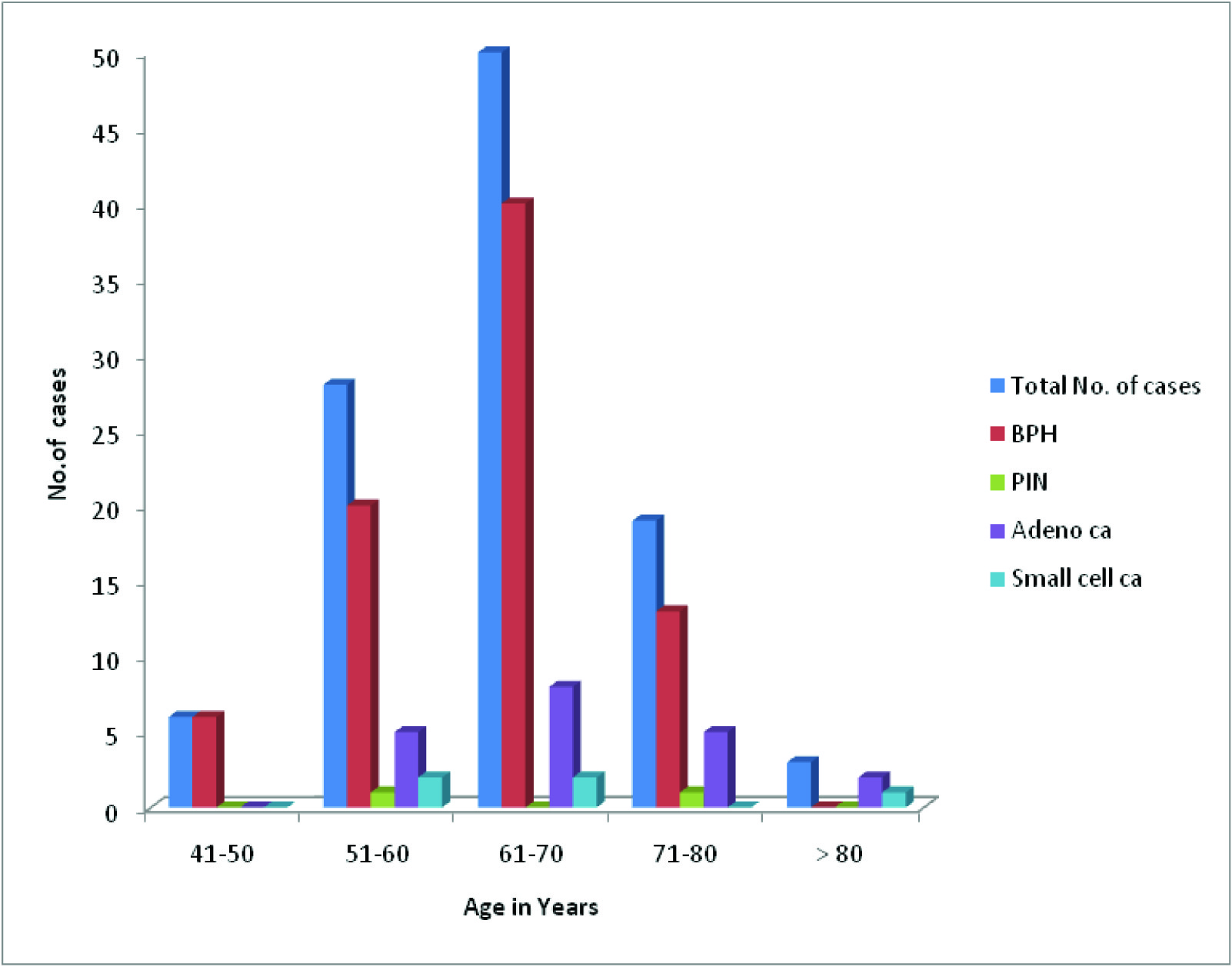
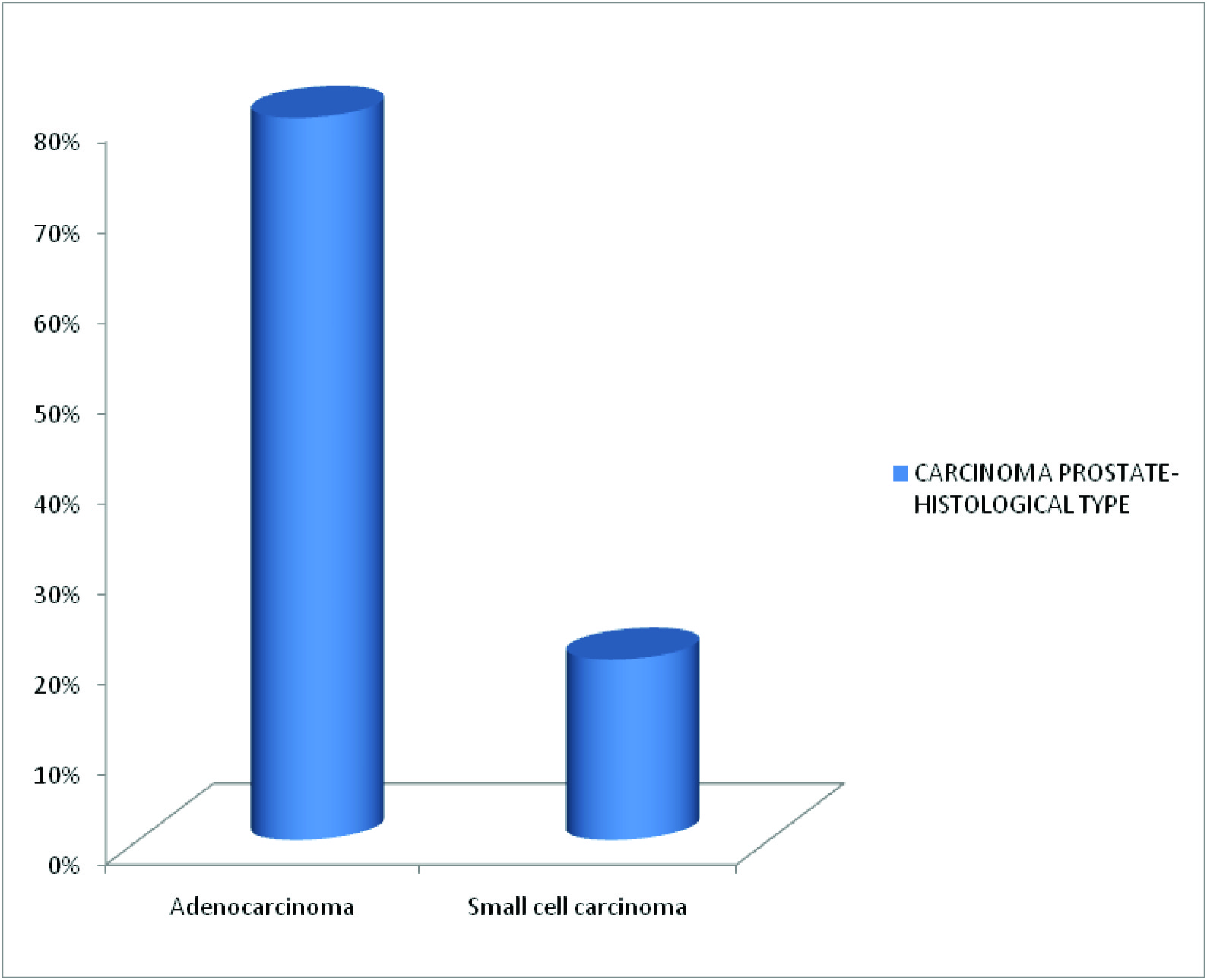
BPH was the most common histological lesion encountered (79 cases–74.52%) with maximum incidence in VII decade [Table/Fig-1] .The mean age of patients with prostatic disorders was 65.5y and the median age noted was 65y. In the present study both BPH and carcinoma of prostate were most common in the seventh decade of life [Table/Fig-2] and difficulty in micturition was the most common presentation(85 cases) followed by frequency of micturition (27 cases) [Table/Fig-3] . BPH was the most common prostatic disorder encountered presenting in 79 cases (74.52%). Majority of them Showed glandulostromal proliferation 61(77.21%). 20(25.31%) cases of BPH showed featuters of associated chronic prostatitis. Two cases (1.89%) of prostatic intraepithelial neoplasia were encountered in the study. Adenocarcinoma of prostate was the most common histological type of carcinoma encountered (20 cases –80%) followed by Small cell carcinoma (5 cases –20%).[Table/Fig-4] .Among the BPH patients, S.PSA levels were available in 29 cases, out of which 16 cases had S.PSA levels in the range of 4-20 ng/ml. The highest value of serum.PSA noted among the BPH patients was 32.33 ng/ml.Among the carcinoma patients, S.PSA levels were available in 16 cases of Adenocarcinoma and 4 cases of small cell carcinoma. Six cases of adenocarcinoma showed very high levels of S.PSA (>80 ng/ml) [Table/Fig-5] . In the present series there were 7 (35%) cases of Adenocarcinoma of prostate with Gleason score 7 and the least score noted was Gleason score 2 presenting in a single case. The most common primary grade noted was grade 3 presenting in nine cases and the least common Primary grade noted was grade 2.
Incidence of Prostatic Disorders

Prostatic Disorders : Age Incidence

Carcinoma Prostate-Histological Pattern
Prostatic disorders & S.PSA Levels

Discussion
Prostatism is a common malady in the geriatric age group. Benign prostatic hyperplasia and Carcinoma of the prostate are increasingly frequent with advancing age and are uncommon before the age of 40 yrs. A careful examination of the prostate in an unselected series of autopsies disclosed nodular hyperplasia in approximately 20% of the men in 40y of age, a figure that increases to 70% by age 60 and to 90% by eighth decade of life. In India the incidence of benign prostatic hyperplasia is estimated to be 92.97% [3] . In patients with clinically detected nodules, raised PSA, needle biopsy/trucut needle biopsy is an established tool to confirm the diagnosis. It is currently estimated that in United States of America approximately 200,000 new cases are detected every year,of which approximately one fifth prove to be lethal [4] . In India the incidence of carcinoma of prostate is estimated at 8/100,000 persons[3] . The incidence of prostatic disorders increases with increasing age in male population. Mittal et al., in their study comprising of 185 biopsies, reported BPH in 172 (92.97%) cases and carcinoma prostate in 13(7.02%) cases [5] . As men age there is increased incidence of Lower Urinary Tract Symptoms. Both BPH and carcinoma of prostate presents with obstructive urinary symptoms. Benign prostatic hyperplasia is characterised pathologically by a cellular proliferation of the epithelial and stromal elements in the prostate gland. These changes begin histologically in the third decade of life and clinically in the fifth decade of life, resulting in increased resistance to urinary flow during micturition. Chute, Panesar and Girman [6] in their study of benign prostatic hyperplasia patients reported obstructive voiding in 36.45% of the patients as the chief complaint followed by frequent urination in 34.75% of the patients. Dysuria, slow stream, increased urinary frequency and complete retention of urine have been historically mentioned as the most common symptoms in patients with carcinoma prostate.
Both BPH and Carcinoma prostate presents with obstructive Urinary Symptoms [7] . In the present study also difficulty in micturition was the most common complaint among the carcinoma prostate patients (22 cases), followed by increased frequency of micturition in seven cases. The incidence of prostate cancer increases with ageing peaks somewhere in the seventh decade of life. Ibrahim et al., in their study reported mean age for benign prostatic lesions as 64.3y and for carcinoma prostate the mean age was 66.8y (7). Lokuhetty et al., in their study reported that maximum incidence of prostatic lesions both benign and malignant prostatic lesions were in the seventh decade of life. The mean age for BPH patients in their series was 68.1y and mean age for carcinoma prostate patients was 71.3y [8] .
In the present study the mean age for prostatic lesions was 65.5y with a mean age of 63.8 y for benign prostatic lesions and a mean age of 68.8 y for carcinoma patients.
In the present study, the maximum incidence of both benign and malignant prostatic lesions was in the seventh decade of life. The mean age of patients with prostatic disorders in the present study was 65.5y (Mean age for BPH was 63.8y & for CA Prostate was 68.8y) which was similar to that of the study by Ibrahim [9] .
Serum PSA and Prostatic Disordes
PSA is the most important tumour marker in the detection of prostate cancer. PSA when used alone cannot be used as an effective screening tool for carcinoma of prostate due to its’ low sensitivity and specificity, especially in the low and intermediate range. Elevations of serum PSA values can be caused by any process that disrupts the normal architecture of prostate allowing the diffusion of PSA into the stroma, leading to its’ entry into the blood through the microvasculature. In case of BPH, the main reason for elevated levels of S. PSA is due to increase in glandular volume. Thus elevated serum PSA levels are observed in conditions such as prostatitis, prostatic infarcts and BPH, though the most clinically important elevations are seen in adenocarcinoma of prostate. Murthy et al., in their study of 261 cases reported maximum number of cases (111) with serum PSA in the range of <4 ng/ml [9] . El imam et al., in their study of serum PSA assay in 194 cases estimated that maximum number of cases (140) was having serum PSA in the range of 4 to 10 ng/ml [10] . Rishi et al., in their series of serum PSA assay in 177 cases also had maximum number of patients (63) presenting with serum PSA values in the range of 4 to 10 ng/ml [11] . In the present study serum PSA estimation was done in 49 cases. Elevations of serum PSA values were observed in our study in both carcinoma of prostate and benign prostatic hyperplasia. The lowest value of serum PSA noted among BPH cases in our study was 0.87 ng/ml and the highest value was 32.33 ng/ml. The lowest value of serum PSA among the carcinoma prostate patients was 7.5 ng/ml and the highest value of serum PSA among the carcinoma patients in the present study was 229.5 ng/ml. In the present study, six cases of carcinoma patients had serum PSA values > 100 ng/ml and was similar to the study done by Murthy and Ray [9] .
Age Specific Serum PSA Values in Prostatic Disorders
Age specific ranges for PSA are important. They increase with advancing age. A single reference range of 0 – 4 ng/ml is not appropriate for men of all ages [12] . In the present study also, a similar trend of elevation of serum PSA values with increasing age was observed. There were only two cases with serum PSA < 4 ng/ ml in fifth decade of life. In the seventh decade, maximum number of cases (10) presented with serum PSA values in the range of 20 to >100 ng/ml.
Carcinoma Prostate and Gleason’s Score
Numerous grading systems have been designed for the histopathological grading of prostate cancer. The prostate biopsy Gleason score correlates with tumour aggressiveness, tumour volume, serum PSA levels, prognosis and influence of the treatment policy. The Gleason score is also often used to determine eligibility of clinical trials including those for watchful waiting [13].
In the study done by Surveillance, Epidemiology, and End Results (SEER) Prostate cancer trends 1973-1995 (1998) 41% of patients had Gleason’s score GS 5-7, 23% had GS 2-4 and 21% with GS 8-10 [4]. In the study done by Bing – Yirshen et al., there were 46% of carcinoma prostate patients presenting with GS 5-7 and 33.3% with GS 2-4 [8]. In the present study 60% of carcinoma cases presented with GS 5-7, 25% with GS 8-10 and 15% with GS 2-4.
Conclusion
Thus, in conclusion benign prostatic hyperplasia was the commonest lesion encountered followed by carcinoma of prostate. CA prostate is associated with elevated levels of serum prostate specific antigen (PSA). But definitive diagnosis can be made out by histopathological examination of prostatic biopsies.
[1]. R Konwar, N Chattopadhyay, HK Bid, Genetic polymorphism and pathogenisis of benign prostatic hyperplasia.BJU Int. 2008 102:536-44. [Google Scholar]
[2]. Aarnik Rene G, P Harrie, Beerlarge J Jean, MJ Frans, Transrectal ultrasound of the prostate: Innovations and future applications.Journal of Urology. 1997 159(5):1568-79. [Google Scholar]
[3]. HK Bid, R Konwar, V Singh, Benign prostatic Hyperplasia; Is it a growing public health concern for India?Indian J Med Sci. 2008 62:373-74. [Google Scholar]
[4]. JL Stanford, RA Stephenson, LM Coyle, Prostate Cancer Trends 1973- 1995.Bethesda, Md:National Cancer Institute: NIH Pub. 1999 pp:99-4543. [Google Scholar]
[5]. BV Mittal, MB Amin, SG Kinare, Spectrum of histological lesions in 185 consecutive prostatic specimens.J Postgrad Med. 1989 35(3):157 [Google Scholar]
[6]. CG Chute, LA Panser, CJ Girman, JE Oesterling, The prevalence of Prostatism; a population based survey of urinary symptoms.Journal of Urology. 1993 150(1):85-89. [Google Scholar]
[7]. I Mansoor, Pattern of prostatic diseases in Saudi Arabia. The Internet journal of Pathology.TMISSN. 2003 2(2):1528-8307. [Google Scholar]
[8]. MD Lokuhetty, HD Wijsinghe, DT Abeysuriya, UC Samarasinghe, Transrectal ultrasound guided prostate biopsies: a single centre experience in Srilanka.Ceylon Medical journal. 2009 54(1):6-9. [Google Scholar]
[9]. DP Murthy, U Ray, J Morewaya, SK Sengupta, A study of the correlation of prostatic pathology and serum prostate specific antigen levels; A perspective from Papua New Guinea.PNG Med J. 1998 41(2):59-64. [Google Scholar]
[10]. M El imam, NZ Higazi, DO Abuidris, Prostate specific antigen versus Digital rectal examination as screening for Ca Prostate in Sudanese patients.Sudanese J of Public health. 2009 4(2):278-81. [Google Scholar]
[11]. R Nayyar, P Singh, NP Gupta, A Seth, R Kumar, Upgrading of Gleason Score on radical prostatectomy specimen compared to preoperative needle core biopsy ; An Indian experience.Indian J of Urology. 2010 26(1):56-59. [Google Scholar]
[12]. JE Oesterling, WH Cooner, SJ Jacobsen, HA Guess, MM Leiber, Influence of patient age on serum PSA concentration. An important clinical observation.Urol Clin North Am. 1993 20:671-80. [Google Scholar]
[13]. R Montironi, R Mazzuccheli, M Scarpelli, Gleason grading prostate cancer in needle biopsies or radical prostactectomy specimens: Contemporary approach, current clinical significance and sources of pathology discrepancies.BJU International. 2005 95:1146-45. [Google Scholar]