Diagnostic Utility of PET CT in Thymic Tumours with Emphasis on 68Ga-DOTATATE PET CT in Thymic Neuroendocrine Tumour - Experience at a Tertiary Level Hospital in India
Julie Hephzibah1, Nylla Shanthly2, Regi Oommen3
1 Associate Professor, Department of Nuclear Medicine, Christian Medical College, Christian Medical College, Vellore, Ida Scudder Road, Vellore, India.
2 Professor, Department of Nuclear Medicine, Christian Medical College, Christian Medical College, Vellore, Ida Scudder Road, Vellore, India.
3 Professor, Department of Nuclear Medicine, Christian Medical College, Christian Medical College, Vellore, Ida Scudder Road, Vellore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Julie Hephzibah, Associate Professor, Department of Nuclear Medicine, Christian Medical College, Vellore, Ida Scudder Road, Vellore-632004, India. Phone : 9994308782, E-mail : drjulsan@cmcvellore.ac.in
Introduction:18 Fluorine-fluoro-2-deoxyglucose positron emis–sion tomography/computed tomography (18F- FDG-PET/CT) is of importance in assessing high-risk thymoma and thymic carcinomas. Detection of advanced thymoma versus thymic carcinoma by routine cross sectional anatomical imaging such as computed tomography (CT), magnetic resonance imaging (MRI) often poses a diagnostic dilemma. In this case series we observed the utility of FDG uptake to predict advanced thymoma and distinguish thymoma from thymic cancer.
Materials and Methods: We reviewed 18F- FDG-PET/CT scans of 12 patients (8 males, 4 females); age 24-60yrs with thymic epithelial malignancy from January 2011 to May 2013. FDG activity in lesions was quantified using maximum standardised uptake value (SUVmax) and correlated with Masaoka staging and WHO classification. All patients fasted 4 hr prior to 18F-FDG PET/CT. Images from vertex to mid-thigh were acquired 60min post injection of 3.7 -4.7 MBq/kg (Mega Becquerel)/kilogram of18F-FDG and SUV max of each tumour was measured. One patient underwent DOTATATE scan, received 138MBq of 68Gallium (68Ga)-DOTATATE injection IV and imaging was done after 60 min.
Results: Higher FDG uptake of SUVmax 7.35 was seen in type B3 thymoma. FDG uptake was higher in thymic carcinoma (20.45 in primary and 17.46 in the node) or neuroendocrine differentiation (NED) than in patients with thymomas (ranged 7.35 - 3.02). No significant association was observed between higher focal FDG uptake and advanced-stage disease in thymoma. In NED 68Ga - DOTATATE imaging identified more lesions than in FDG.
Conclusion: PET CT is a valuable diagnostic tool in evaluation of thymic tumours, to assess in initial workup, for treatment response and for prognostication. 68Ga-DOTATATE PET/CT is beneficial in assessing neuroendocrine thymic tumours. Focal FDG uptake cannot predict advanced thymoma but is helpful in distinguishing thymoma from thymic carcinoma, or the more aggressive thymoma B3.
18F-FDG PET, 68Gallium-DOTATATE, Neuroendocrine differentiation, Thymoma, Thymic Carcinoma
Introduction
18Fluorine – fluoro-2-deoxyglucose Positron Emission Tomography/ computed tomography (18F-FDG-PET/CT) is an important functional imaging modality in assessing high-risk thymoma and thymic carcinomas. Tumours of the thymus are uncommon and are usually considered as being indolent, although this is often true of thymomas; thymic adenocarcinoma and thymic neuroendocrine cancer can be aggressive and have a poor prognosis. Physiologic uptake of FDG is seen in the thymus in 28% of normal people aged less than 40 yrs, with the incidence dependent on the age of the patient, being identified in up to 73% of children under 13 y, decreasing up to 8% of people in their fourth decade [1]. Our primary objective was to assess the usefulness of 18F-FDG-PET, if FDG uptake can predict advanced thymoma, distinguish thymoma from thymic cancer and if 68Ga- DOTATATE-PET was useful in thymic carcinoma with neuroendocrine differentiation (NED).
Materials and Methods
We reviewed 18F-FDG-PET/CT scans of 12 consecutive newly diagnosed patients with thymic epithelial malignancy from January 2011 to May 2013 and documented focal FDG activity using SUV max. All patients fasted for at least 4 hr before undergoing 18F-FDG PET examination. The patients received an intravenous injection of 3.7–40 MBq/kg of 18F-FDG. Image acquisition was performed after 60 minutes using a PET-CT scanner (Biograph 6; Siemens Medical Solutions, Erlangen, Germany). Three-dimensional emission scanning was performed from the vertex to the mid-thigh. The emission time per bed position was two minutes (12–16 min per whole-body scan), which is in accordance with standard clinical protocols. For the semi quantitative assessment, regions of interest (ROIs) were put over on FDG-avid mediastinal tumours, and the SUVmax {the maximum ROI activity (MBq/g)/injected dose (MBq)/body weight (g)) of each tumour was measured. This was correlated with Masaoka–Koga staging and WHO classification. Of the 12 patients one patient underwent 18F-FDG PET/CT at diagnosis and after a year underwent 68Ga-DOTATATE PET/CT as he had thymic carcinoma with NED.
Results
Of the 12 patients, nine were diagnosed to have thymoma, one thymic cyst, one thymic carcinoma and 1 thymic carcinoma with NED. Age ranged from 24-60 yrs; eight were males and four females.
The SUV max measured were as follows:
Low risk type thymoma 3-5
Type B3 thymoma 7.35
Thymic carcinoma 20.45
Thymic cyst was not 18F-FDG avid.
In NED 68Ga- DOTATATE imaging identified additional lesions and hence was superior to 18F-FDG PET/CT.
Discussion
18F-FDG-PET/CT in the diagnosis of mediastinal masses is not a routine investigation but is of significance in assessing high-risk thymoma and thymic carcinomas. CT and MRI are exceptional modalities for localization of mediastinal masses but has limited role in assessment of the aggressiveness of masses, identify viable tumour in residual masses after chemotherapy or radiotherapy.
Inoue and Luzzi et al., [2,3] reported that SUVmax of low-risk thymomas containing types A, AB and B1 tumours was significantly lower than those of high-risk thymic tumours consisting of types B2 & B3 thymomas and thymic carcinomas. So much so that Luzzi et al., [3] suggested that ‘any anterior mediastinal mass whose SUVmax is >5 not be resected without biopsy because of the possibility that it may be more aggressive than thymoma or even a nonsurgical disease such as lymphoma’. In our case series we found that patient with B3 had a higher SUVmax. Consistent with previous reports [4–8], our study found higher FDG uptake in thymic carcinoma than in thymoma although there were no significant differences in uptake among high and low risk groups of thymoma. Sharma et al., [9] studied the role of 18F-FDG PET/CT in thymic carcinoma diagnosis and reported that SUVmax of >/=7 in the presence of lobulated masses with areas of necrosis and calcification, encasement of mediastinal structures, pleural thickening, mediastinal lymphadenopathy and distant metastases was suggestive of thymic carcinoma.
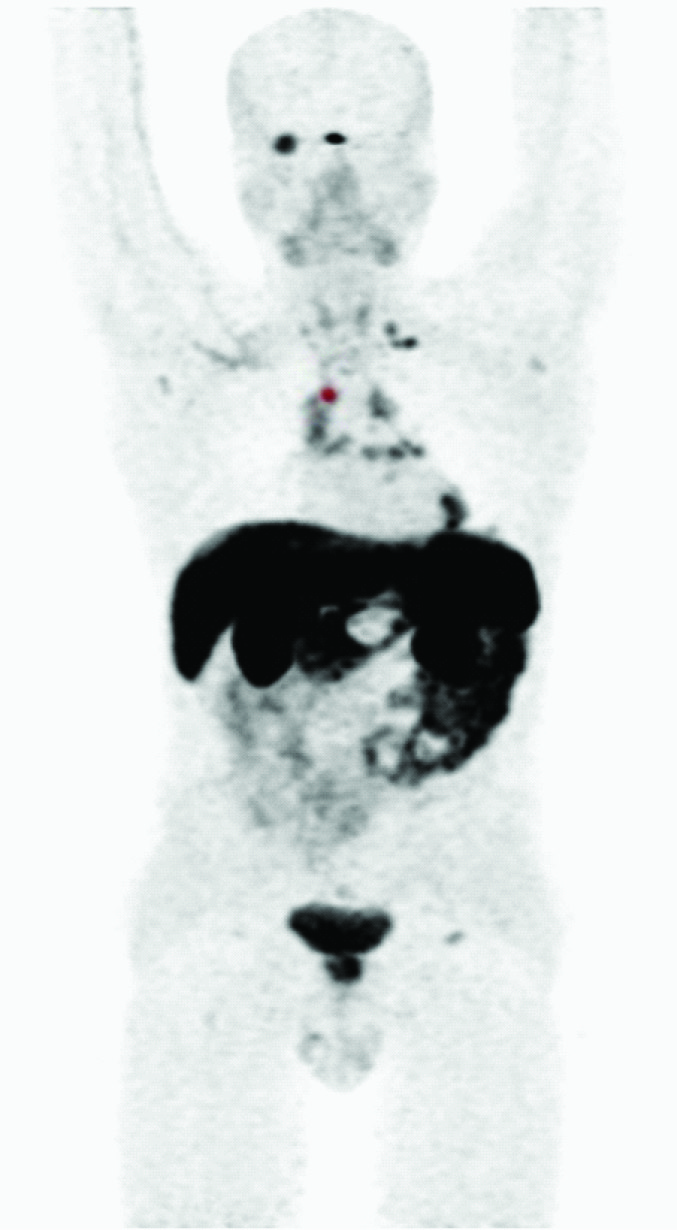
Thymomas and thymic carcinomas are diverse with respect to oncological behaviour. Surgical resection is the main modality of treatment for thymomas and multidisciplinary treatment with induction chemotherapy is recommended for patients with Stage III disease with great vessel invasion or Stage IV disease [10,11]. Thymic carcinomas are much more aggressive tumours, and the incidence of lymph node and distant metastasis is higher than that observed in thymomas.18F-FDG PET/CT is useful in the follow up and to assess response to therapy [Table/Fig-1] of patients diagnosed with thymic tumours. 68Ga-DOTATATE-PET/CT is a valuable imaging modality in the diagnosis of neuroendocrine tumours. One patient with thymic carcinoma and NED underwent this imaging modality [Table/Fig-2a,b,c] and additional lesions were picked up in comparison to FDG PET, thus indicating a useful role in NED. In 68Ga- DOTATATE avid tumours peptide receptor radiotherapy (PRRT) with 177Lutetium can be considered as the therapeutic option [12]. 18F-FDG PET imaging plays an important role in monitoring treatment response and predicting survival in advanced thymic epithelial tumours as shown by Thomas et al., [13] in a prospective study of 56 patients with Masaoka stage III and IV, metabolic responders had significantly longer progression-free survival of 11.5 vs 4.6 months suggesting that an early metabolic response closely correlates with therapy outcome.
32yr old lady with anterior mediastinal mass and lung lesion. Serial FDG PET CT imaging. 1a, b. Preop FDG PET – lesion in anterior mediastinum and left lung lower zone consistent with thymoma AB with Focal B3, stage 4a. 2 a,b. Postop imaging showing no lesion in the primary and the region of lung. 3 a,b. Follow up scan was unremarkable

30yr old gentleman with thymic carcinoma & NED. Maximum Intensity projection (MIP) of 18F-FDG PET showing lesion in anterior mediastinum & left lung

MIP of 68Ga-DOTATATE: Multiple lesions are seen in the right orbit, left supraclavicular, mediastinal & hilar nodes, pericardial deposits
Axial image showing right orbital lesion seen more prominently in 68Ga-DOTATATE PET/CT

Conclusion
PET/CT is a valuable diagnostic tool in evaluation of thymic tumours, in initial workup, to assess treatment response and for prognostication. 68Ga-DOTATATE-PET/CT is valuable in assessing neuroendocrine thymic tumours and to plan for therapy with 177Lutetium-DOTATATE if positive. Focal FDG uptake cannot predict advanced thymoma but is helpful in distinguishing thymoma from thymic carcinoma.
[1]. Jerushalmi J, Frenkel A, Bar-Shalom R, Khoury J, Israel O, Physiologic thymic uptake of 18F-FDG PET in children and young adults: a PET/CT evaluation of incidence, patterns, and relationship to treatmentJ Nucl Med 2009 50:849-53. [Google Scholar]
[2]. Inoue A, Tomiyama N, Tatsumi M, Ikeda N, Okumura M, Shiono H, F-18-FDG PET for the evaluation of thymic epithelial tumours: Correlation with the World Health Organization classification in addition to dual-time-point imagingEJNMMI 2009 36:1219-25. [Google Scholar]
[3]. Luzzi L, Role of fluorine-flurodeoxyglucose positron emission tomography/computed tomography in preoperative assessment of anterior mediastinal massesEur J Cardiothorac Surg 2009 36:475-79. [Google Scholar]
[4]. Igai H, Matsuura N, Tarumi S, Chang SS, Misaki N, Go T, Usefulness of [18F] fluoro-2-deoxy D-glucose positron emission tomography for predicting the WHO malignancy grade of thymic epithelial tumoursEur J Cardiothorac Surg 2011 40:143-5. [Google Scholar]
[5]. Kaira K, Endo M, Abe M, Nakagawa K, Ohde Y, Okumura T, Biologic correlation of 2-[18F]-fluoro-2-deoxy-D-glucose uptake on positron emission tomography in thymic epithelial tumoursJ Clin Oncol 2010 28:3746-53. [Google Scholar]
[6]. Sung YM, Lee KS, Kim BT, Choi JY, Shim YM, Yi CA, 18F-FDG PET/CT of thymic epithelial tumours: usefulness for distinguishing and staging tumour subgroupsJ Nucl Med 2006 47:1628-34. [Google Scholar]
[7]. Endo M, Nakagawa K, Ohde Y, Okumura T, Kondo H, Igawa S, Utility of 18FDG-PET for differentiating the grade of malignancy in thymic epithelial tumoursLung Cancer 2008 61:350-5. [Google Scholar]
[8]. Sasaki M, Kuwabara Y, Ichiya Y, Akashi Y, Yoshida T, Nakagawa M, Differential diagnosis of thymic tumours using a combination of11C-methionine PET and FDG PETJ Nucl Med 1999 40:1595-601. [Google Scholar]
[9]. Sharma P, Evaluation of thymic tumours with 18F-FDG PET–CT: a pictorial reviewActa Radiol 2013 54(1):14-21. [Google Scholar]
[10]. Falkson CB, Bezjak A, Darling G, Gregg R, Malthaner R, Maziak DE, The management of thymoma: a systematic review and practice guidelineJ Thorac Oncol 2009 4:911-19. [Google Scholar]
[11]. Yokoi K, Matsuguma H, Nakahara R, Kondo T, Kamiyama Y, Mori K, Multidisciplinary treatment for advanced invasive thymoma with cisplatin, doxorubicin, and methylprednisoloneJ Thorac Oncol 2007 2:73-78. [Google Scholar]
[12]. Baum RP, Wehrmann C, Zachert C, Long-term results of peptide receptor radionuclide therapy (PRRT): 5-year follow-up of 1,150 courses in 360 patients with progressive somatostatin receptor positive neuroendocrine tumours in one clinical centerJ Nucl Med 2007 48(Suppl 2):37P [Google Scholar]
[13]. Thomas Anish, Mena Esther, Kurdziel Karen, 18F-Fluorodeoxyglucose Positron Emission Tomography in the Management of Patients with Thymic Epithelial TumoursClin Cancer Res 2013 19:1487-93. [Google Scholar]