Tracheobronchial Amyloidosis-A Series of Two Cases
Kavita V1, Palak D Raiyani2, Sunil S Vyas3
1 Assistant Professor, Department of General Pathology, Christian Medical College, Vellore, India.
2 Assistant Professor, Department of General Pathology, Christian Medical College, Vellore, India.
3 Assistant Professor, Department of Pulmonary Medicine, Christian Medical College, Vellore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kavita V, Assistant Professor, Department of General Pathology, 3rd Floor, ASHA building, Christian Medical College, Vellore, India. Phone : 9176009166, E-mail : drkavitav@gmail.com
Amyloidosis is a rare disorder characterised by accumulation of insoluble fibrillar proteins in extracellular space. Respiratory amyloidosis presents as two tracheobronchial forms (local and diffuse) and two parenchymal forms (nodular and diffuse), of which diffuse tracheobronchial amyloidosis is the least common. We herein present two cases of tracheobronchial amyloidosis.
Amyloidosis, Diagnosis, Tracheobronchial
Case Report
Case -1
A 67-year-old gentleman presented to the outpatient clinic with a five month history of progressive pain in the right hip and difficulty in weight bearing on the right leg. He also complained of progressive shortness of breath.
Investigations- Urine Bence Jones proteins- positive, serum and immunofixation electrophoresis were normal.
MRI pelvis revealed a lytic expansile lesion involving the right ilium, acetabulum with trabeculations within it. No matrix mineralization. Cortical breech with soft tissue extension was present.
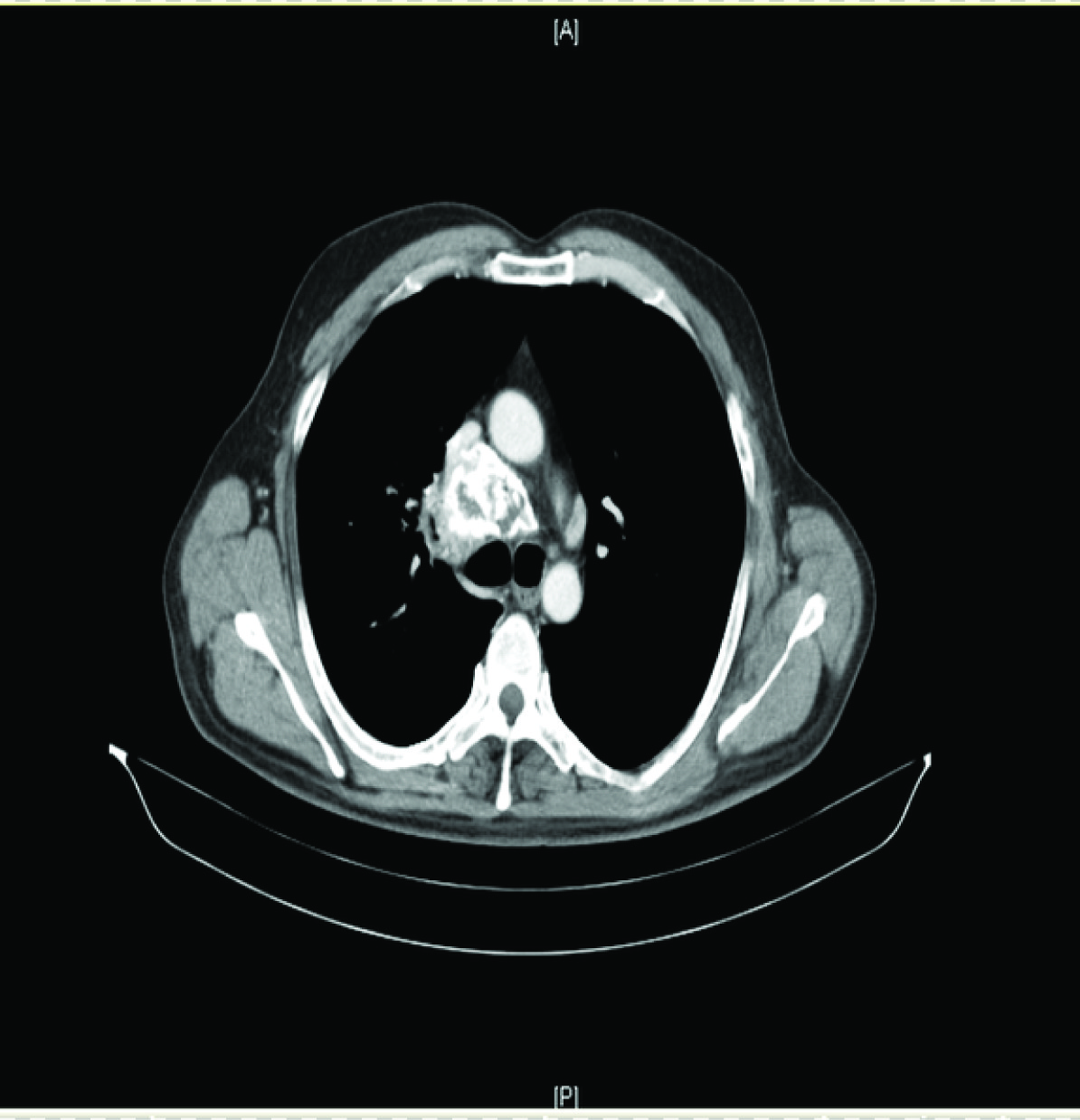
CT Thorax- Diffuse interlobular septal thickening/branching nodular opacity at upper lobe of right lung [Table/Fig-1].
CT Thorax- Diffuse interlobular septal thickening / branching nodular opacity at upper lobe of right lung
Biopsy of the acetabular mass showed a tumour composed of sheets of plasma cells including few immature forms. The plasma cells were positive for CD138 in keeping with a diagnosis of plasmacytoma.
Bronchoscopy was done and revealed a mass lesion in the upper lobe of right lung [Table/Fig-2].
Bronchoscopy showing mass lesion in the upper lobe of right lung

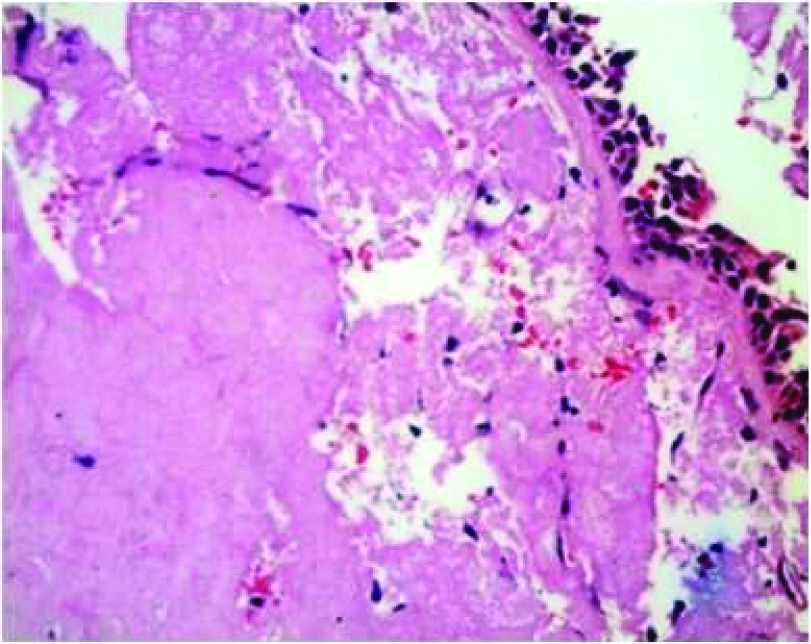
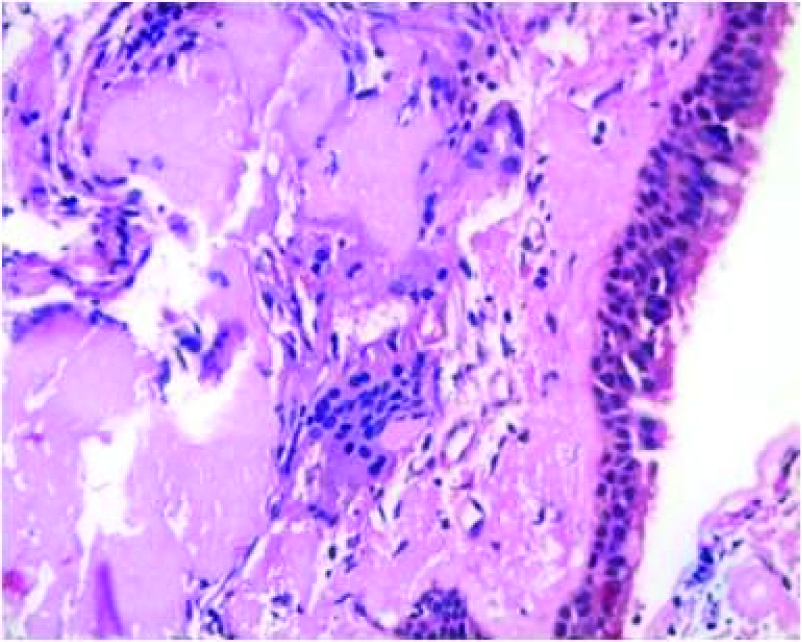
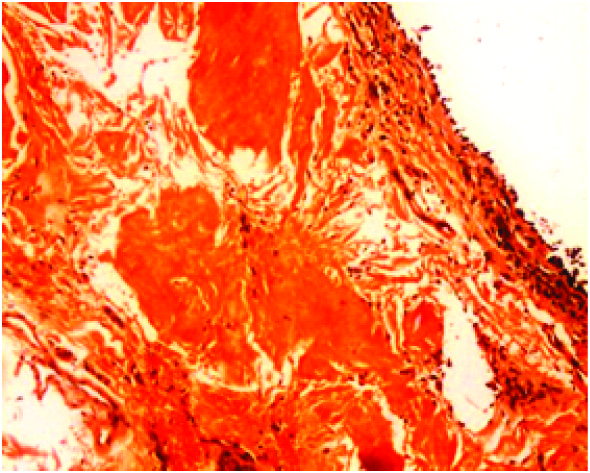
Transbronchial lung biopsy was done and showed subepithelial deposits of acellular eosinophilic homogenous material resembling amyloid [Table/Fig-3]. Some of these deposits formed casts surrounded by inflammatory cells composed of lymphocytes, histiocytes and multinucleate giant cells [Table/Fig-4].These deposits showed apple green birefringent under polarising microscopy using Congo red stain [Table/Fig-5]. Thioflavine T stained the deposits. On immunohistochemistry Lambda light chain antibody intensely stained the deposits [Table/Fig-6]. Kappa light chain antibody was negative.
Subepithelial deposits acellular eosinophilic homogenous material resembling amyloid, H&E 400x magnification
Some of these deposits formed casts surrounded by inflammatory cells and multinucleate giant cells,H&E 400x magnification

Lambda light chain antibody stains the deposits 200X

This patient was treated for the hip lesion with radiotherapy. Bronchoscopy guided therapeutic excision of the lung lesion has been planned. Currently the patient is on symptomatic treatment and under follow-up.
Bronchoscopy showing mass lesion in the upper lobe of right lung.
Case-2
History: A 31-year-old female came with history of cough, breathlessness and haemoptysis since two years.
CT thorax- Left lower lobe broncholithiasis resulting in collapse of left lower lobe with mucus filled, dilated bronchi. The bronchus intermedius was dilated with beaded appearance [Table/Fig-7] .
CT thorax- left lower lobe broncholithiasis resulting in collapse of left lower lobe with mucus filled, dilated bronchi

Bronchoscopy showed localized nodules in the left main bronchus and lower lobe of left lung [Table/Fig-8].
Bronchoscopy showing localized nodules in left main bronchus

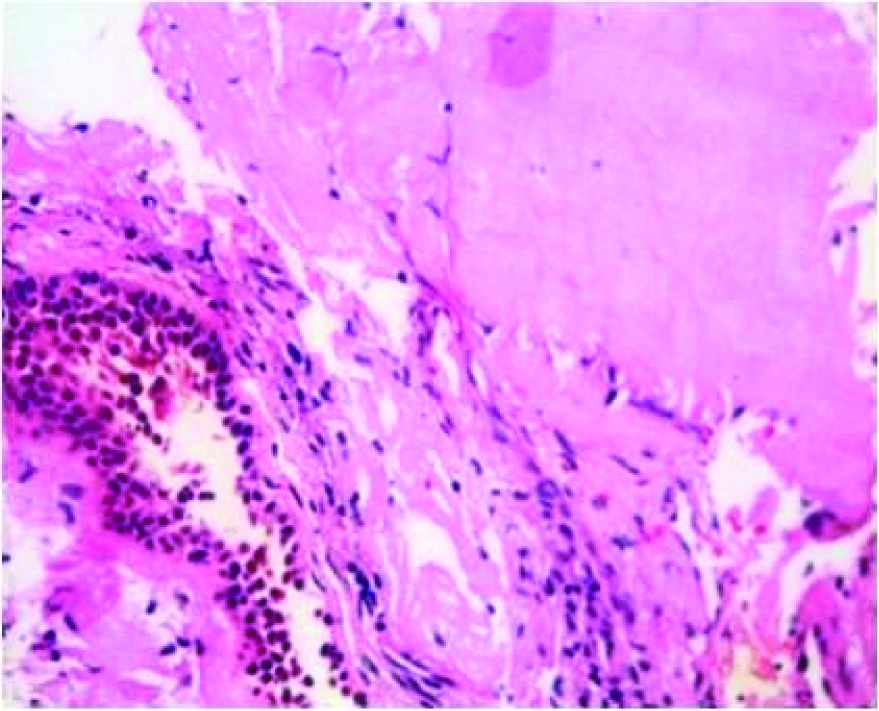
Transbronchial lung biopsy was done and showed subepithelial deposits of acellular eosinophilic homogenous material resembling amyloid [Table/Fig-9]. These deposits showed apple green birefringent under polarising microscopy using Congo red stain [Table/Fig-10]. Thioflavine T stained the deposits. On immunohistochemistry Lambda and kappa light chain antibodies were negative. In addition there were foci of calcification.
Subepithelial deposits of acellular eosinophilic homogenous material resembling amyloid, H&E 400x magnification
Treatment : Bronchoscopy guided Nd-YAG laser excision has been planned for the lung lesion.
Discussion
Amyloidosis is a rare disorder characterised by accumulation of insoluble fibrillar proteins in extracellular space. Amyloid is a complex protein which has the ability to form a beta pleated sheet. Amyloidosis can involve the lung as a local manifestation or as a part of systemic amyloidosis. Respiratory amyloidosis was first described in 1877 by Lesser [1]. Respiratory impairment is uncommon and there are four types of involvement: two tracheobronchial forms (local and diffuse) and two parenchymal forms (nodular and alveolar septal), of which diffuse tracheobronchial amyloidosis is the least common [2].
Piard et al., described a case in which the patient had a solitary pulmonary plasmacytoma associated with deposits of nonamyloid immunoglobulin light chain located within and away from the tumour. There was no associated paraprotein or evidence of systemic disease [3]. Morinaga et al., have described deposits of nonamyloid light chain in a patient with an extramedullary plasmacytoma involving the left lower lobe of the lung associated with multiple lymph node and pleural nodules. Bone marrow biopsies and skeletal surveys revealed no evidence of extrathoracic disease [4]. In contrast, our first case showed deposition of amyloid with lambda light chain restriction in a patient with solitary plasmacytoma of right acetabulum.
Our second patient was a young lady presenting with cough, hemoptysis and breathlessness. She had been visiting the OPD for asthma like illness, Hence, there was no clinical suspicion of amyloidosis. However, due to symptoms refractory to treatment, a CT thorax was done which revealed broncholithiasis with collapse of lower lobe of left lung. Based on CT thorax, the clinical diagnosis was of tracheopathica osteoplastica. However, her biopsy revealed amyloid deposits with foci of calcific deposits which differentiates this condition from tracheopathica osteoplastica which also has calcific deposits and metaplastic bone [5], but no amyloid deposition. Serraj et al., have reported a case of idiopathic tracheobronchial amyloidosis mimicking asthma, but unlike our case there was no widespread distribution and associated calcific deposits [6].
Bronchial debulking or surgical excision remains the mainstay of treatment in amyloidosis. Use of carbon dioxide laser or yttrium aluminum garnet laser has also been reported [6].
Conclusion
Tracheobronchial amyloidosis clinically presents with symptoms of airway disorders. Hence, early diagnosis and therapeutic intervention is important to prevent respiratory failure. Histopathology remains the gold standard for diagnosis of tracheobronchial amyloidosis. With therapeutic modalities and supportive care, the morbidity and mortality can be reduced.
[1]. Gillmore JD, Hawkins PN, Amyloidosis and the respiratory tractThorax 1999 54:444-51. [Google Scholar]
[2]. Ozer C, Nass DM, Yildz A, Apaydin FD, Egilmez H, Arpaci T, Primary diffuse tracheobronchial amyloidosis: case reportEur J Radiol 2002 44:37-9. [Google Scholar]
[3]. Piard F, Yaziji N, Jarry O, Solitary plasmacytoma of the lung with light chain extracellular deposits: a case report and review of the literatureHistopathology 1998 32:356-61. [Google Scholar]
[4]. Morinaga S, Watanabe H, Gemma A, Plasmacytoma of the lung associated with nodular deposits of immunoglobulinAm J Surg Pathol 1987 11:989-95. [Google Scholar]
[5]. Meyer C.N, Døssing M, Broholm H, Pseodotomoral Tracheobronchopathia osteochondroplasticaRespiratory medicine 1997 91(8):499-502. [Google Scholar]
[6]. Serraj Journal of Medical Case Reports 2012 6:40 [Google Scholar]