Pneumocystis Pneumonia – A Novel Complication in a Non-HIV Dengue Patient
Swapndeep Singh Atwal1, Swapnil Puranik2, Shibani Mehra3, Umesh Chandra Garga4
1 Senior Resident, Department of Radiology, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
2 Junior Resident, Department of Radiology, Govt. Medical CollegeKota, Rajasthan, India.
3 Associate Professor, Department of Radiology, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
4 Professor and Head of Department, Department of Radiology, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Swapndeep Singh Atwal, 8/4, 3rd Floor, Old Rajinder Nagar, New Delhi-110060, India. Phone : 9013837423, E-mail :swapndeepsinghatwal@gmail.com
Dengue, Pneumocystis pneumonia
Dengue fever is a rapidly emerging arboviral infection in human beings spredominantly in tropical and subtropical countries. It is transmitted by the bite of Aedes mosquitoes [1]. It is a self-limiting viral illness with varying symptomatology ranging from completely asymptomatic infection to fulminant form of dengue known as dengue haemorrhagic fever. The common symptoms include fever, joints and body pain. Fever usually lasts for 5-7 days. Recovery is complete but gradual. Some patients may progress to Dengue haemorrhagic fever and Dengue shock syndrome. Dengue haemorrhagic fever is having more dramatic course with persistently falling platelet counts and plasma leak. There is a higher chance of bleeding in such patients. Complications after dengue are rare but can occur depending upon the severity of infection, host immune status and presence and absence of comorbidities. These include mild hepatic dysfunction, iritis, retobulbar and bulbar haemorrhage, orchitis, oophritis and pneumonia. Pneumocystis pneumonia has not been described in association with dengue. We report a case of dengue fever that developed pneumocystis pneumonia during the course of his illness.
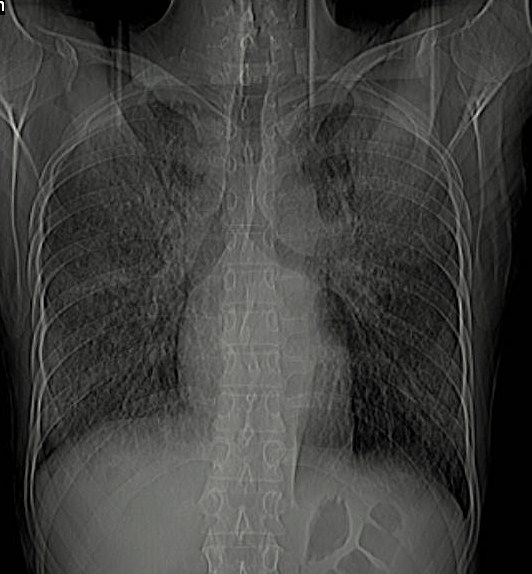
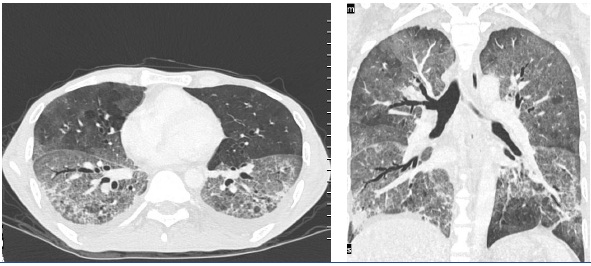
A 33-year old male presented with two days history of high grade fever with chills, headache, generalized body ache and vomiting. His haematological investigations on the day of admission revealed haemoglobin 9.5 mg%, white blood cells count of 4,500/cu.mm, platelets 1,20,000/ cu.mm with mildly elevated alanine aminotransferase and aspartate aminotransferase. Peripheral blood smear was negative for malarial parasite.His PaO2 was 96%.He was seronegative for HIV with normal CD4 count. His ELISA test for was positive for dengue. Chest radiograph was unremarkable, [Table/Fig-1] and ultrasound abdomen suggested mild hepatomegaly and mild ascites. Patient was stared with conservative management including antipyretic for fever. Since fourth day of treatment patient became progressively dyspnoeic with dry cough. His PaO2 was 76% with alveolar-arterial gradient of 38 mm Hg. Repeat chest radiograph show bilateral fine reticulo-nodular and ground glass opacity predominantly in upper and mid-zones. Subsequently CECT chest was done, which revealed patchy ground glass and crazy paving areas in both lungs [Table/Fig-2a & 2b]. Few lung cysts and patchy infiltrates were also seen. There was no lymphadenopathy. Mild pleural effusion was present on the right side. CT findings suggested a possibility of pneumocystis pneumonia though possibility of viral pneumonia was not ruled out. Patient was started with trimethoprim-sulphamethoxazole at a dose of 100 mg/kg/day intravenous and prednisolone at a dose of 50 mg/day for five days and then tapered for next two weeks. Meanwhile, bronchoalveolar lavage was performed which confirmed pneumocystis infection. Patient started responding from day 4th of the start of antibiotics and significantly recovered in 10 days, however the antibiotics were continued for 21 days. The patient was discharged after complete recovery.
Frontal chest radiograph showing reticulonodular shadows with underlying haziness involving both the lung predominantly in parahilar and upper zones
Computed tomography chest (a) axial and (b) coronal image in lung window setting showing bilateral patchy ground glass and crazy-paving pattern
Pneumocystis pneumonia is a common fungal respiratory infection in HIV positive patient particularly with CD4 counts <200/cu.mm, but can be seen in non-HIV patients like patients on drug therapy for rheumatoid arthritis, immunosuppressive therapy and transplant recipients [2,3]. It presents with non-productive cough, fever, breathlessness with reduced PaO2 and increased alveolar-arterial gradient [4].
To the best of our knowledge, this is probably the first case in which pneumocystis pneumonia is seen associated with dengue infection in a non-HIV patient. This case draws attention to the rare complication in dengue illness and emphasizes the importance of considering pneumocystis pneumonia as a possibility in patients with dengue fever with appropriate symptoms and imaging findings, so that timely management can be done.
[1]. Engelthaler DM, Fink TM, Levy CE, Leslie MJ, The reemergence of Aedes aegypti in ArizonaEmergInfect Dis Apr-Jun 1997 3(2):241-42. [Google Scholar]
[2]. Mori S, Sugimoto S, Pneumocystis jirovecii infection: an emerging threat to patients with rheumatoid arthritisRheumatology 2012 :1-11. [Google Scholar]
[3]. Sing A, Roggenkamp A, Autenrieth IB, Heesemann J, Pneumocystis carinii carriage in immunocompetent patients with primary pulmonary disorders as detected by single or nested PCRJ. Clin. Microbiol 1999 37(10):3409 [Google Scholar]
[4]. Fujii T, Nakamura T, Iwamoto A, Pneumocystis pneumonia in patients with HIV infection: clinical manifestations, laboratory findings, and radiological featuresJ Infect Chemother 2007 13(1):1-7. [Google Scholar]