Synchronous Presentation of Chronic Myeloid Leukemia with Carcinoma Penis: A Rare Presentation
Abhijeet P. Ganapule1, Vivi Srivasvas Tavaavaava2, Ramani Manoj Kumar3, Nirmal T.J4, Auro Viswabandya5
1Assistant Professor, Department of Haematology, Chrisitan Medical College, Vellore, India.
2Professor, Head Cytogenetics, Department of Pathology, Chrisitan Medical College, Vellore, India.
3Associate Professor, Department of Pathology, Chrisitan Medical College, Vellore, India.
4Associate Professor, Department of Urology, Chrisitan Medical College, Vellore, India.
5Professor, Department of Haematology, Chrisitan Medical College, Vellore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Auro Viswabandya, Christian Medical College and Hospital, Ida Scudder Road, Vellore, Tamil Nadu-632004, India. Phone : 9486455605,
E-mail: aurov@cmcvellore.ac.in
We report here a case of 52-year-old male presenting with penile ulcer. On evaluation, he was diagnosed to have Carcinoma penis with concurrent CML in chronic phase. Clinical examination showed pallor, bilateral inguinal lymphadenopathy, bilateral pitting pedal oedema and hepatosplenomegaly. He was diagnosed to have chronic myeloid leukemia based on peripheral smear examination showing raised counts with shift to left and fluorescence in situ hydridisation (FISH) showing t (9:22). The ilio-inguinal block dissection specimen showed inguinal metastasis of squamous cell carcinoma (SCC). This case is being presented here in view of the rarity in combination of CML with another malignancy.
Chronic myeloid leukemia- chronic phase (CML-CP), Fluorescence in situ hybridization (FISH), Squamous cell carcinoma (SCC)
Case Report
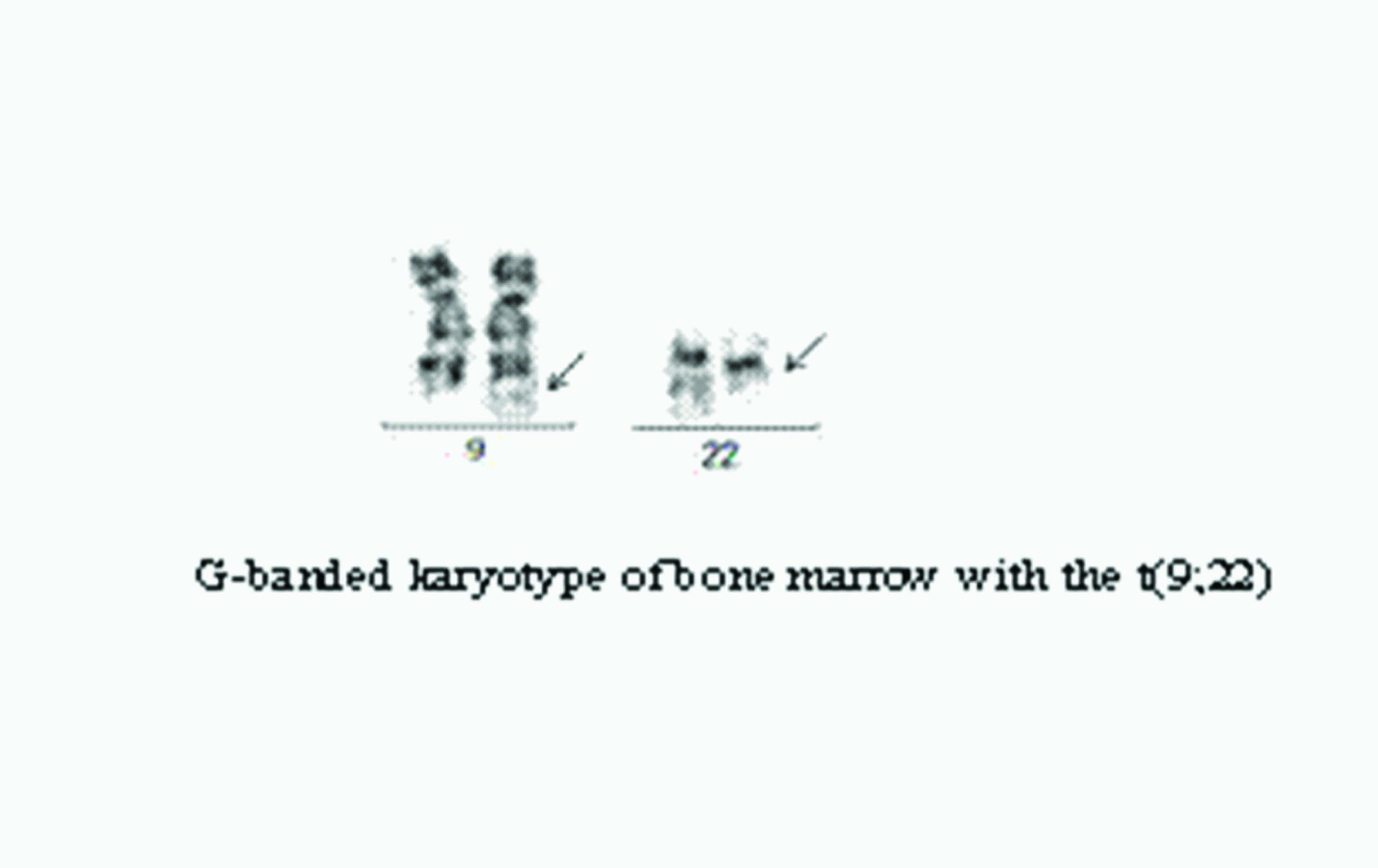
A 52-year-old gentleman presented with an ulcer on the foreskin of penis, with occasional blood stained discharge for last one year. He also gave history of swelling of both the legs extending to groin for last two weeks. There was no history of multiple sexual contacts. There was no history of smoking or alcohol consumption. He was circumcised during the evaluation of penile ulcer in native place. The penile skin biopsy was reported as squamous cell carcinoma, hence was referred to our centre for further management. General examination revealed pallor, bilateral multiple matted inguinal lymph nodes (largest measuring 2cm in diameter) and bilateral pitting pedal oedema extending upto the groin [Table/Fig-1]. Abdominal examination revealed hepatomegaly of 5cm and splenomegaly of 7cm. External genitalia examination showed partially circumcised, redundant foreskin overlying glands with no obvious ulcer or swelling. Rest of clinical examination was unremarkable. The routine blood counts done revealed -Haemoglobin- 6.9 grams%, Total leucocyte counts- 249000/mm3, Platelet counts - 7, 38,000/ mm3. Differential counts were as follows- Blasts- 2%, Promyelocytes- 3%, Myelocytes-20%, Metamyelocytes-9 %, Band forms-9 %, Neutrophils-51%, Eosinophils-3 %, Basophils- 2 %, Lymphocytes- 1 %, Nucleated red blood cells - 1/100 mm3. Peripheral smear was suggestive of CML in chronic phase [Table/Fig-2]. Florescence in situ hybridization (FISH) as well as karyotyping analysis on peripheral Sectionblood and bone marrow respectively showed translocation (9:22) [Table/Fig-3] . He underwent bilateral ilio-inguinal block dissection for suspected carcinoma penis with inguinal metastasis. The biopsy from inguinal lymph node showed nests of malignant epithelial cells with vesicular nuclei and visible nucleoli [Table/Fig-4&5] . A diagnosis of squamous cell carcinoma with metastasis to lymph nodes was made. Carcinoma penis was staged as TxN3M0. He was started on Imatinib mesylate as treatment for chronic myeloid leukemia, which was complicated by prolonged cytopenia. The patient could not receive any specific aggressive chemotherapy for carcinoma penis due to persistent, prolonged cytopenia secondary to Imatinib.
Discussion
CML is probably the most studied human malignancy [1]. The classic textbook description of the natural history of chronic myeloid leukemia is a stereotypical progression from relatively benign chronic phase through accelerated phase, finally into blast crisis [2]. Squamous cell carcinoma (SCC) post treatment with hydroxyurea and imatinib has been seen in patients with CML [3,4]. There are few case reports of SCC preceding or following (metachronous) CML, however only one case has been reported in literature of CML occurring simultaneously (synchronous) with SCC [5-7]. CML preceding or following second primary tumour has been reported in literature [5-7]. Budrukkar et al., reported seven patients of CML who had metachronous squamous cell carcinoma of head and neck [5]. The median interval in this study was 6y between diagnosis of CML and second primary tumours [5]. All seven patients were on either Imatinib or hydroxyurea as treatment for treatment of CML prior to detection of second primary tumour [5]. In this case series at median follow up of 14 months, three were alive free of second primary tumours [5].
Ugur Ural et al., reported a case of carcinoma cervix treated with radiation, four years later presented with CML [6]. Gola et al., reported a series of 200 CML patients on treatment, among which 6(3%) patients had synchronic or metachronic second primary tumour. One patient had synchronic neoplasm, the remaining five had metachronous neoplasm’s [7].
One of the postulated hypothesis for associated neoplasm in patients with CML who are on Imatinib may be related to decreased NK cell function following Imatinib, making them prone to develop other malignancies [8]. High incidence of non specific mutation in tumour suppressor gene p53, have been seen with concurrent use of tobacco and alcohol [9]. For CML, he was started on Imatinib Mesylate at dose of 400 mg once a day, however, after one week of treatment it was complicated by prolonged cytopenia which required growth factor treatment. Though not common, pancytopenia post imatinib treatment has been reported in literature [10]. He had carcinoma penis, which was staged as TxN3M0. He needed adjuvant Cisplatin and 5 Flurouracil based chemotherapy [11].
Ideally this patient should have been treated for carcinoma penis with aggressive chemotherapy. However, in view of his prolonged cytopenia secondary to Imatinib, he opted against aggressive chemotherapy and went on palliative chemotherapy, with concurrent continuation of imatinib for his CML.
Penile ulcer and bilateral inguinal lymphnodes

Peripheral smear showing CML in CP

G-banded karyotype of bone marrow with the t(9;22)
Lymp node involvement by Squamous cell carcinoma 40X

Histopathology picture of skin biopsy

Conclusion
We report here a rare case of CML, which presented synchronously with carcinoma penis. To the best of our knowledge, this case report is second in literature of CML presenting synchronously with SCC.
[1]. WN Michael Deininger, Goldman V Junia, Melo. The molecular biology of chronic myeloid leukemia.Blood 2000 96:3343-56. [Google Scholar]
[2]. JP Radich, The Biology of CML blast crisis.Hematology Am Soc Hematol Educ Program. 2007 :384-91. [Google Scholar]
[3]. GE Panuk, B Turget, O Vural, M Demer, M Tek, S Altaner, Metastatic Squamous cell carcinoma of skin in CML-complication of hydroxyurea treatment.Clin Lab Hematol. 2003 25:324-31. [Google Scholar]
[4]. G Baskaynak, K Krazer, M Schwarz, Squamous cutaneous epithelial cell carcinoma in 2 CML patient with progressive disease with CML.Eur J haematol. 2003 70:231-34. [Google Scholar]
[5]. A Budrukkar, S Muttagi, T Shahid, P Chatturvedi, S Banavali, SG Laskar, V Murthy, Second primary head and neck squamous cell cancer with aggressive behavior in patients with chronic myeloid leukaemia.British Journal Oral Maxllofacial Surgery. 2012 50(6):504-07. [Google Scholar]
[6]. Ural A Ugur, Chronic myeloid leukemia Following Radiotherapy for carcinoma of cervix: Report of case and brief Review of literature.American journal of Haematology. 2007 82:41-8. [Google Scholar]
[7]. A Gola, A Reszko, Chronic granulocytic leukemia and an organ neoplasm in the same person.Pol Tyg Lek. 1996 15(19-22):289-90. [Google Scholar]
[8]. N Rajaram, RJ Tatake, SH Advani, SL Nail, SG Gangai, Natural killer and lymphokine activated killer cell function in CML. Cancer Immunol Immunother. 1990 31:44-48. [Google Scholar]
[9]. JA Bresnnan, JO Boyle, WM Koch, Association between cigarette smoking and mutation of the p53 gene in squamous cell carcinoma of head and neck.NEJM 1995 332:712-17. [Google Scholar]
[10]. Khan Kurshid Ahmed, Junaid Ayesha, Siddique Nauman Saleen, Imatinib related bone marrow aplasia after complete cytogenetics response in CML. Journal of college of Physician and Surgeons Pakistan. 2008 18(3):176-78. [Google Scholar]
[11]. Pizzacaro G. , Algaba F, Horenblas S, Solsona E, Tana S, Poel H .Van Der, Wathin N., Guidelines on penile cancer.Eur Urol. 2010 57(6):1002-12. [Google Scholar]