Non Puerperal Uterine Inversion in A Young Female- A Case Report
Setu Rathod1, Sunil Kumar Samal2, P Pallavee3, Seetesh Ghose4
1 Assistant Professor, Department of Obstetrics and Gynaecology, Mahatma Gandhi Medical College & Research Institute, Puducherry, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, Mahatma Gandhi Medical College & Research Institute, Puducherry, India.
3 Associate Professor, Department of Obstetrics and Gynaecology, Mahatma Gandhi Medical College & Research Institute, Puducherry, India.
4 Professor and Head, Department of Obstetrics and Gynaecology, Mahatma Gandhi Medical College & Research Institute, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Setu Rathod, 4-D, Type II Staff Quarters, Mahatma Gandhi Medical College, Pillaiyarkuppam, Pondicherry-607402, India. Phone : 917598191660, E-mail : seturathod@gmail.com
We report a case of 28-year-old, primipara who presented with complaints of mass descending per vaginum along with excessive bleeding and foul smelling vaginal discharge for the past six months. Clinical examination revealed an inverted uterus, cervix and vagina with a large submucosal fundal fibroid. A diagnosis of non-puerperal uterine inversion was made. Surgical management included vaginal myomectomy with repositioning of the uterus using an abdomino-vaginal approach and a successful outcome. Histopathology confirmed the diagnosis of leiomyoma. Hence, we conclude that uterus-sparing surgery should be considered in young females desirous for future pregnancy until the final pathology is known.
Myomectomy, Non-puerperal, Uterine inversion
Case Report
A 28-year-old P1L1 woman presented to our outpatient department with the complaints of mass descending per vaginum and foul smelling vaginal discharge for the past six months. She had an institutional normal vaginal delivery two and a half years back which was uneventful. She had history of irregular and excessive menstrual flow with intermittent abdominal pain for the last one year and was treated in local hospital medically.
General examination revealed pallor and haemoglobin estimation was reported as 7.4gm/dl. There was no other systemic abnormality. Gynaecological examination revealed a mass protruding through the vaginal introitus which was globular and the broadest leading part measured 25x10x6cm [Table/Fig-1]. The surface of the mass appeared hemorrhagic, edematous and had a shaggy look. No opening could be seen in the leading part of mass. Cervical os could not be identified. There was no active bleeding at that time. On palpation the mass felt firm and bled on touch. Vagina was completely inverted out, cervix could not be felt and the mass was found to be irreducible. Uterine sound could not be passed.Uterus could not be felt and a vacuum was felt anteriorly in the per rectal examination.
Uterine inversion with submucous leiomyoma

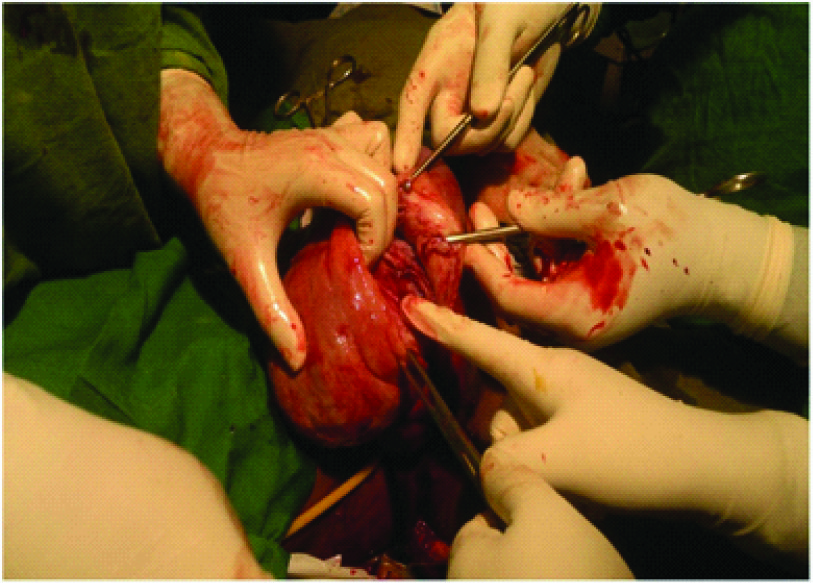
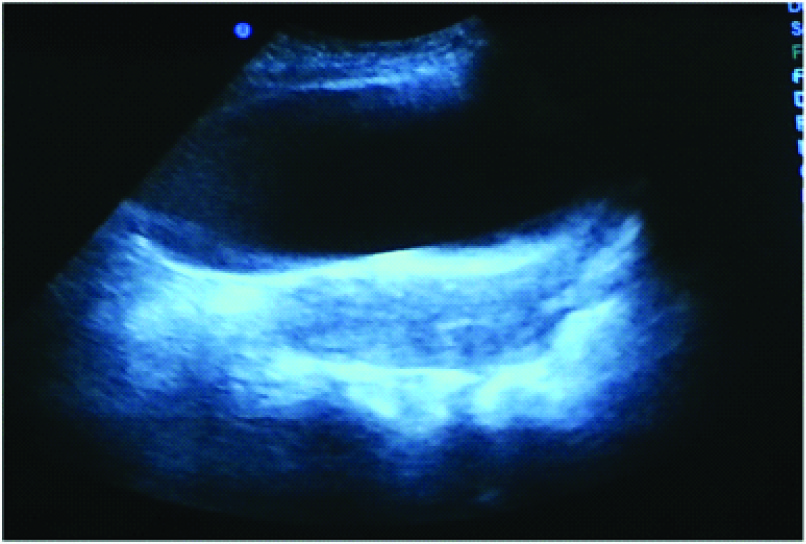
Transabdominal ultrasound could not identify uterus in its normal position in pelvis. A provisional diagnosis of chronic uterine inversion with submucosal fundal myoma was made and the patient was prepared for surgery. Continuous bladder drainage with Foleys catheter and broad spectrum intravenous antibiotics was started. Blood transfusion was done to improve her anaemic status preoperatively. Local dressing using the antiseptic solution of povidone iodine and hygroscopic action of magnesium sulphate was done daily. Intravenous pyelography was done preoperatively to trace the course of ureter. As the patient was young and desirous of future pregnancy, a combined abdomino-vaginal approach using Kustner’s method was undertaken to reposition the uterus into the pelvic cavity. Vaginal myomectomy [Table/Fig-2] was done by giving a longitudinal incision on the most dependent part of mass with posterior extension followed by enucleation of the fibroid. Redundant wall was excised and the uterus was reposed into the pelvic cavity [Table/Fig-3]. Abdominal part of the operation entailed accessing the abdominal cavity through a transverse incision which revealed normal appearing bilateral ovaries, visible distal parts of fallopian tube and an absent uterine corpus along with the medial ends of fallopian tube. Through the abdominal approach, the uterine incision was repaired in layers. Postoperative period was uneventful. The patient was asymptomatic and doing well at six weeks and six months of postoperative follow-up [Table/Fig-4]. Histopathology confirmed the diagnosis of leiomyoma.
Abdominal view after correcting inversion

Post operative USG picture showing uterus after reposition
Discussion
Chronic non-puerperal uterine inversion affects mostly women with intrauterine tumour like submucosal leiomyoma while other causes are leiomyosarcoma, endometrial carcinoma, rhabdomyosarcoma, malignant mixed mullerian tumour and endometrial stromal carcinoma [1]. This condition is very rare, accounting for only one sixth of all cases of uterine inversion [2]. Usually, the cases of non-puerperal uterine inversion present after 45y; are mostly related to benign myomas and rarely associated with malignancies [3]. Only few cases of non-puerperal inversions have been reported in young women and in most cases the aetiology is attributed to malignancy [1,4]. Uterine leiomyoma are known to cause inversion in 78-85% of cases [4,5].
Clinical presentations of non-puerperal inversion include vaginal bleeding, mass descending through the introitus, lower abdominal pain, and urinary problems. Definitive diagnosis is made by Ultrasound and Magnetic Resonance Imaging (MRI). In T2 weighted MRI scan, a U-shaped uterine cavity with a thickened, inverted uterine fundus on a sagittal image and a “bull’s eye” configuration on an axial image are signs indicative of uterine inversion [6].
Different surgical approaches are followed for treatment of chronic non-puerperal uterine inversion. Abdominal approaches include Huntington’s and Haultain whereas vaginal approaches include Kustner and Spinelle. Kustner procedure includes entering the pouch of Douglas vaginally and splitting the posterior aspect of the uterus and cervix and finally re-inverting the uterus where as in Spinelli’s method incision is given in anterior aspect of cervix and uterus is reinverted [7]. Where fertility is wished, the uterine incision is repaired through abdominal approach otherwise routine vaginal hysterectomy can be proceeded. Malignant tumours may be present in case of non-puerperal uterine inversion as reported by Takano et al., showing 92% association with tumours out of which 71.6% were leiomyomas and 20% malignant tumours [8]. Thus, a high index of suspicion should be maintained.
Conclusion
The cases of non-puerperal uterine inversion are uncommon and are difficult to manage even for an experienced gynaecologist. In selected cases, where fertility preservation is needed, uterine reposition with repair of uterine incision can be done.
[1]. de Vries M, Perquin DAM, Non-puerperal uterine inversion due to submucous myoma in a young woman: a case reportJournal of Medical Case Reports 2010 4:21 [Google Scholar]
[2]. Krenning RA, Nonpuerperal uterine inversion. Review of literatureClin Exp Obstet Gynecol 1982 9:12-15. [Google Scholar]
[3]. Gomez-Lobo V, Burch W, Khanna PC, Non-puerperal uterine inversion associated with an immature teratoma of the uterus in an adolescentObstet Gynecol 2007 110:491-93. [Google Scholar]
[4]. Lupovitch A, England ER, Chen R, Non-puerperal uterine inversion in association with uterine sarcoma; case report in a 26-year-old and review of the literatureGynecol Oncol 2005 97(3):938-41. [Google Scholar]
[5]. Simms-Stewart D, Frederick S, Fletcher H, Char G, Mitchell S, Postmenopausal uterine inversion treated by subtotal hysterectomyJ Obstet Gynaecol 2008 28(1):116-17. [Google Scholar]
[6]. Lewin JS, Bryan PJ, MR imaging of uterine inversionJ comput Assist Tomogr 1989 13:357-59. [Google Scholar]
[7]. Fofie C, Baffoe P, Non puerperal uterine inversion: A case reportGhana Med J 2010 44:79-81. [Google Scholar]
[8]. Takano K, Ichikawa Y, Tsunoda H, Nishida M, Uterine inversion caused by Uterine Sarcoma: A Case ReportJpn J Clin Oncol 2001 31(1):39-42. [Google Scholar]