Acute Abdomen Due to Penicillium marneffei: An Indicator of HIV Infection in Manipur State
Hemanth Sureshwara Ghalige1, Biswajeet Sahoo2, Sanjeeb Sharma3, Khuraijam Ranjana Devi4, Sudhir Chandra Singh TH5
1 Junior Resident, Department of Surgery, RIMS, Imphal, India.
2 Junior Resident, Department of Microbiology, RIMS, Imphal, India.
3 Junior Resident, Department of Microbiology, RIMS, Imphal, India.
4 Associate Professor, Department of Microbiology, RIMS, Imphal, India.
5 Professor, Department of Surgery, RIMS, Imphal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kh Ranjana Devi, Associate Professor, Department of Microbiology, RIMS, Imphal-795004, India. Phone : 9862780378, E-mail : ranjanakhu@rediffmail.com
Opportunistic infection in HIV disease often present to clinicians in an atypical manner testing clinical acumen. Here, we report a case of Penicilliosis marneffei (PM) infection presenting to surgical emergency as acute abdomen with undiagnosed HIV status in advanced AIDS, chief complaints being prolonged fever and diffuse abdominal pain. Radiologic imaging showed non-specific mesenteric and retroperitoneal lymphadenopathy. Fine needle aspiration cytology (FNAC) of the lymph node was done and subjected to direct microscopy, gram staining and culture on Sabouraud’s dextrose agar (SDA) which showed Penicillium marneffei. He was then treated with intravenous amphotericin. This case is reported for its rarity and unusual presentation to sensitise clinicians and microbiologists to consider PM as an aetiology in acute abdomen in high risk individuals, more so, in patients from north-east India.
Acute abdomen, HIV, Mesenteric lymphadenopathy, Penicillium marneffei
Case Report
A-28-year-old male military personnel presented with a four day history of right sided non-colicky abdominal pain radiating to the back, and associated with fever and rigor for two weeks, at Regional Institute of Medical Sciences (RIMS), Imphal, Manipur, India. The fever used to subside only on medication. He had no other gastrointestinal or urinary symptoms. He was not an intravenous drug abuser but consumed alcohol in moderate amounts regularly. There was history of significant weight loss in the recent past.
On general examination, he was pyrexic with associated tachycardia. Other than pallor and non tender non matted multiple lymphadenopathy no other significant finding was present.
Abdomen was diffusely tender with mild guarding and could be palpated properly only after administering analgesics (Inj. Diclofenac 75 mg i.m.). Multiple lumps were palpated in all the quadrants. The lumps were firm in consistency, tender and mobile. Liver was just palpable.
Chest radiograph looked normal. His blood test showed neutrophilia (20×109/l), a raised ESR of 120 and a raised C-reactive protein of 200 mg/l. The rest of the blood tests including serum amylase were in the normal range.
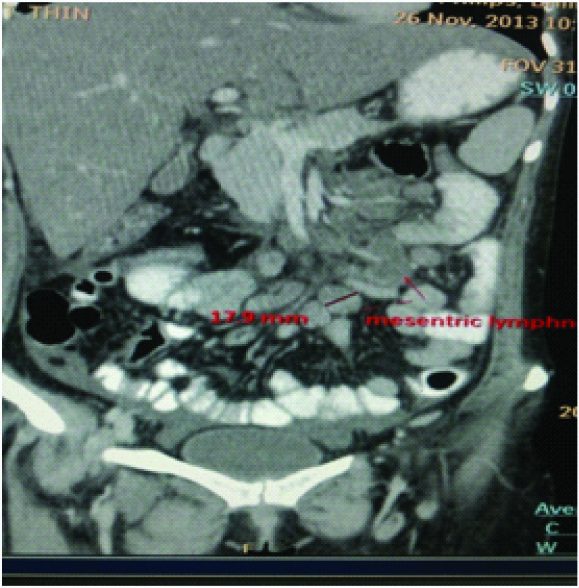
An abdominal radiograph was non-contributory and computed tomography of the abdomen multiple enlarged mesentric lymph nodes [Table/Fig-1]. Patient was treated conservatively and started on broad spectrum intravenous antibiotics (ceftriaxone and ofloxacin) but his condition did not improve.
CECT abdomen showing multiple mesenteric lymph nodes
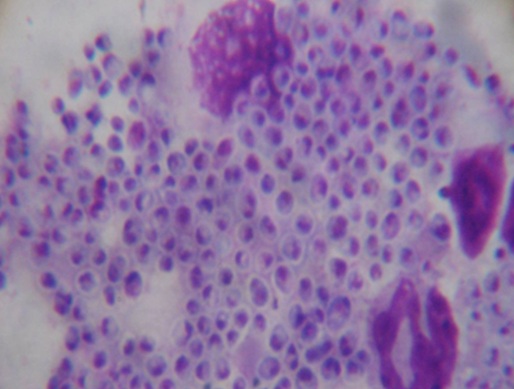
Fine needle aspiration cytology (FNAC) of neck nodes and retroperitoneal lymph nodes showed Penicillium marneffei like organisms which were present both intra and extra cellularly [Table/Fig-2] following which we counselled the patient to get HIV test done, which was positive and CD4+ count was 8 cells/mm3.
Giemsa stained lymph node aspirate showing intracellular and extracellular yeast
Cultures of blood and lymph node aspirate showed growth on 3rd day itself which were consistent with culture characteristics of Penicilliummarneffei [Table/Fig-3].
Granular yellow colour growth with a characteristic red diffusible pigmentation on SDA at 250C

Peri oral umbilicated lesions [Table/Fig-4] appeared in the 4th day during the course of antifungal treatment which further described the Penicillium dissemination. Treatment was started with Amphotericin B at the dose of 0.6 mg/kg/day intravenously for two weeks followed by Anti Retroviral Therapy and itraconazole as per recommendation. The patient showed marked improvement on follow up after six months and was symptom free with CD4 cell count of 350/mm3.
Peri oral umbilicated lesions

Discussion
Penicilliosis marneffei (PM) is a disseminated and progressive fungal infection caused by Penicillium marneffei, a facultative intracellular pathogen and the only dimorphic species of the genus Penicillium [1,2].
Human beings and bamboo rats are the only known animal hosts of P. marneffei. Ranjana et al., [3] has clearly indicated the local epidemiology of infection citing plenty of bamboo grooves in immediate vicinity of human dwelling in Manipur and consumption of raw and fermented bamboo shoots on regular basis by the people.
Most patients have constitutional symptoms like fever, weight loss and malaise. Skin manifestations such as subcutaneous abscesses and papule-like ulcers may be present [2]. It is common to have signs and symptoms reflecting involvement of reticulo-endothelial system including anaemia, hepatosplenomegaly and lymphadenopathy. In our case at presentation though fever, weight loss, lymphadenopathy were present, there was no apparent history suggestive of HIV infection, prevalence of tuberculosis in India makes other diagnosis a rarity in clinical practice often overlooking other opportunistic infections.
Respiratory involvement is often present, with productive cough, dyspnoea and haemoptysis. Chest X-ray may show diffuse reticular infiltration, localized alveolar infiltrates or cavitatory lesion [4]. Our patient didn’t have any findings of pulmonary involvement.
The infection may rarely present as acute abdomen [5]. In patients with advanced HIV/AIDS who present with acute abdomen, opportunistic fungal infections of the bowel especially penicilliosis needs to be considered as aetiology, more so in patients from a distinct geographic region such as South-East Asia [6]. Authors have previously isolated four cases of disseminated P. marneffei in patients who were already suffering from HIV infection from the state of Manipur [1]. In this case also acute abdomen was the presenting feature making a strong point for clinicians in the north-east India to be aware of such presentation in emergency services making PM as an indicator disease of HIV. This case is justified being a rare, for the fact that after diagnosis of P. Marneffei, HIV positivity was tested.
Penicilliosis is mostly seen in late HIV infection with CD4+ count less than 100/mm3 [7]. Up to 80% or more of the cases have CD4+ count below 50/mm3 [8–10]. In our patient CD4+ was only 8/mm3 at presentation.
In Southeast Asia, it is the third most common opportunistic infection in human immunodeficiency virus (HIV)-infected patients, following tuberculosis and cryptococcosis, in its prevalence and incidence [5,11]. Human penicilliosis was uncommon until the development of HIV Pandemic and now it has become one of the AIDS defining illnesses of HIV positive patients in endemic areas. Ranjana et al., [3] reported 25% incidence of PM in HIV patients in Manipur state.
P. marneffei is the only dimorphic fungus in the genus Penicillium. It exists in mycelial form at 250C but in yeast form at 370C. It shows a rapid growth rate and matures within three days at 25–300C. Its growth is enhanced in Sabouraud dextrose agar (SDA) but is inhibited by cycloheximide. At 250C, the colonies of P. marneffei are granular with shade of greenish-yellow colour and a characteristic red diffusible pigment. Little or no red diffusible pigment is produced at 35°C to 37°C. Microscopically, the mould form is typical of other Penicillium species with hyaline septated hyphae and fruiting structures composed of branching metulae and phialides which produce spherical conidia in chains [7]. In our case, SDA was used with success in isolating the organism. Also, we insist that lymph node aspirates (cervical and retroperitoneal, mesenteric lymph nodes) perhaps has a better yield in such cases with constitutional symptoms in ruling out other aetiologies involving reticulo-endothelial system. Our suggestion is supported by case series from the author [3].
Conclusion
We stress upon considering Penicilliosis as one of the differential diagnosis for acute abdomen in immune suppressed individuals in the Manipur, north east part of India in this era of HIV pandemic. Multimodality approach (Clinicians, Radiologists, Pathologists and Microbiologists) increases diagnostic yield and cure of the patients.
[1]. Singh NP, Ranjana KH, Singh YI, Singh KP, Sharma SS, Kulachandra M, Indigenous Disseminated Penicillium marneffei Infection in the state of Manipur, India: Report of four Autochthonous CasesJ Clin Microbiol 1999 37(8):2699-702. [Google Scholar]
[2]. Cooper CR, McGinnis MR, Pathology of Penicillium marneffei: an emerging acquired immunodeficiency syndrome-related pathogenArch Pathol Lab Med 1997 121(8):798-804. [Google Scholar]
[3]. Ranjana KH, Priyokumar K, Singh TJ, Gupta ChC, Sharmila L, Singh PN, Disseminated Penicillium Marneffei infection among HIV-Infected Patients in Manipur StateIndia. J Infect 2002 45:268-71. [Google Scholar]
[4]. Deesomchok A, Tanprawate S, A 12-case series of Penicillium marneffei pneumoniaJ Med Assoc Thai 2006 89(4):441-47. [Google Scholar]
[5]. Ko CI, Hung CC, Chen MY, Hsueh PR, Hsiao CH, Wong JM, Endoscopic diagnosis of intestinal penicilliosis marneffei: report of three cases and review of the literatureGastrointest Endosc 1999 50(1):111-14. [Google Scholar]
[6]. George IA, Sudarsanam TD, Pulimood AB, Mathews MS, Acute abdomen: an unusual presentation of disseminated Penicillium marneffei infectionIndian J Med Microbiol 2008 26(2):180-82. [Google Scholar]
[7]. Viviani MA, Vanittanakom N, Topley & Wilson’s Microbiology and Microbial infections- Medical Mycology 2005 10th editionLondonHodder Arnold [Google Scholar]
[8]. Supparatpinyo K, Khamwan C, Baosoung V, Nelson KE, Sirisanthana T, Disseminated Penicillium marneffei infection in Southeast AsiaLancet 1994 344:110-13. [Google Scholar]
[9]. Wu TC, Chan JW, Ng CK, Tsang DN, Lee MP, Li PC, Clinical presentations and outcomes of Penicillium marneffei infections: a series from 1994 to 2004Hong Kong med J 2008 14(2):103-09. [Google Scholar]
[10]. Antinori S, Gianelli E, Bonaccorso C, Ridolfo AL, Croce F, Sollima S, Disseminated Penicillium marneffei infection in an HIV-positive Italian patient and a review of cases reported outside endemic regionsJ Travel Med 2006 13(3):181-88. [Google Scholar]
[11]. Duong TA, Infection due to Penicillium marneffei, an emerging pathogen: review of 155 reported casesClin Infect Dis 1996 23:125-30. [Google Scholar]