Tandem Rhomboid Flap Repair: A New Technique in Treatment of Extensive Pilonidal Disease of the Natal Cleft
Naveen N1, Kamal Kumar M2, Ramesh Babu K3, Prema Dhanraj4
1 MCh Resident, Department of Plastic Surgery, Rajarajeswari Medical College & Hospital, Kambipura, Bangalore, India.
2 Associate Professor, Department of Plastic Surgery, Rajarajeswari Medical College & Hospital, Kambipura, Bangalore, India.
3 Professor, Department of Plastic Surgery, Rajarajeswari Medical College & Hospital, Kambipura, Bangalore, India.
4 Professor and HOD, Department of Plastic Surgery, Rajarajeswari Medical College & Hospital, Kambipura, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Naveen N, #90, 14th Main, 14th Cross, 2nd Stage, 2nd Phase, West of Chord Road, Mahalakshmipuram, Bangalore - 560086, India. Phone : 9980023372, E-mail : naveen_uno1@yahoo.co.in
Pilonidal sinus is an annoying chronic benign disease causing disability in young adults, mainly affecting the intergluteal furrow. Treatment of this condition remains controversial and is represented by a myriad of techniques available. Most of the techniques are judged against open excision and secondary healing in terms of minimizing disease recurrence and patient discomfort. More recently superiority of flap reconstruction to non-flap techniques is accepted. An ideal operation should be simple, associated with minimal pain and wound care after surgery, minimize hospital stay and have a low recurrence rate. We hereby present a new type of rhomboid flap technique for an extensive pilonidal sinus disease. This technique has given good results in our hands considering the aforementioned factors of an ideal operation. The following case report is of our first stint with the procedure.
Extensive pilonidal sinus, Rhomboid flap, Transposition flap
Case Report
A 29-year-old, male driver presented in surgery out-patient with complaints of a pus discharging swelling in the sacral region with intermittent bouts of pain and fever since 18 mnth. Treatment for the same had been taken elsewhere with frequent relapses. Patient had no co-morbidities and except for intermittent treatment of the pilonidal disease he was not on chronic medication. Family history was not contributory. On examination, the patient had a hairy back with deep intergluteal cleft with two sinuses 17 cm apart in the midline. One was present 6 cm away from the anal verge and second 23 cm away. Since the General surgeons were in favour of a primary closure of the resulting defect after wide excision we (Plastic surgeons) were called in. After examination, to achieve primary closure we planned for the use of double rhomboid flaps which were in tandem to cover the resulting defect.
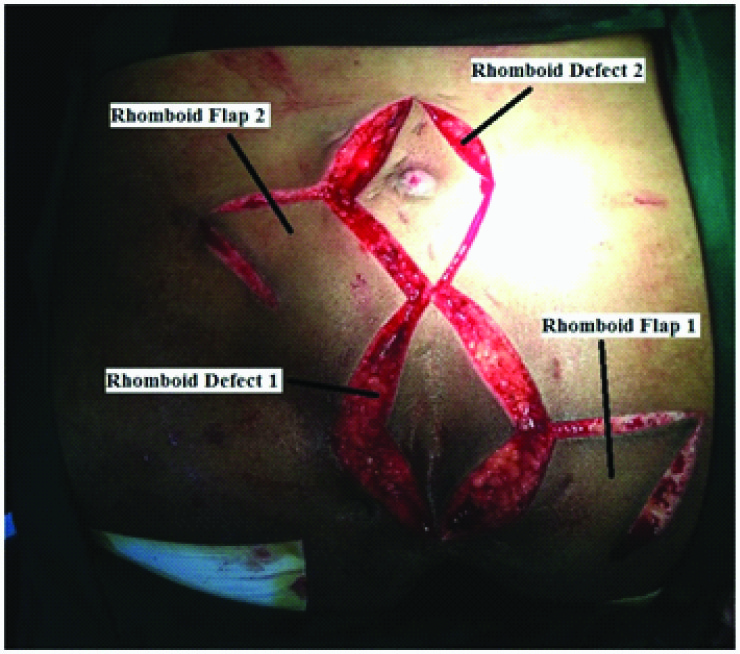
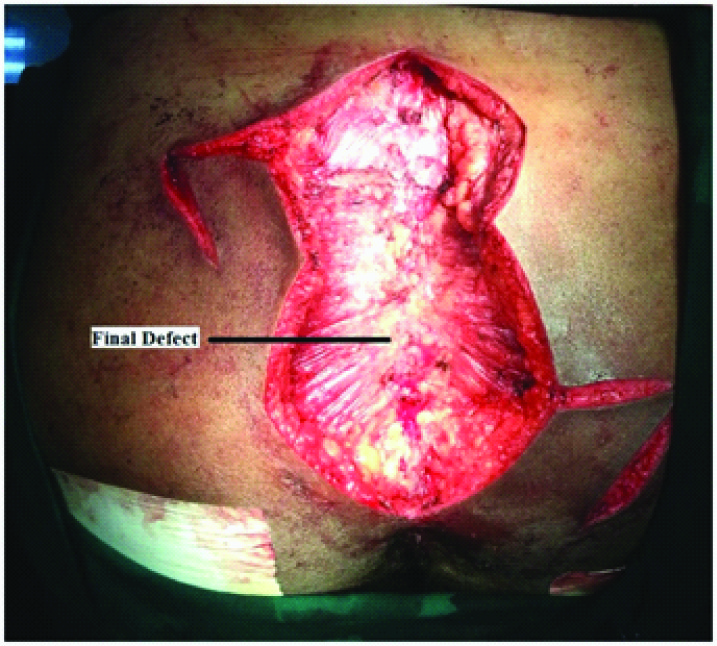
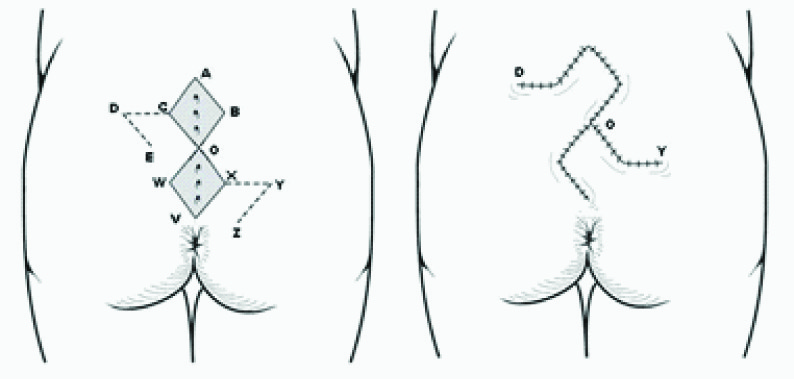
Technique – With patient in jack knife position and buttocks parted using adhesive tapes on either side two rhomboids with their long axis in tandem and falling in the midline covering the entirety of all the sinuses of the disease were planned [Table/Fig-1]. The long axes of the two rhomboids measured 10 & 11 cm individually and 21 cm put together. All sinuses and tracts were excised with two rhomboid defects in tandem on the skin but the underneath adipofacial tissue formed a single bloc and disease was removed en-bloc [Table/Fig -2, 3, 4]. Excision of the diseased tissue down to the presacral fascia was done. Two rhomboid fasciocutaneous flaps (incorporating the gluteal fascia) were raised on either sides of the two rhomboid defects and transposed onto the defects with 2 layered intermittent suturing using Vicryl and Nylon without tension over suction-drains [Table/Fig-5]. Postoperative period was uneventful and the patient was mobilized 24 h later, drains removed after 48 h [Table/Fig-6] and discharged on 3rd day. Sutures are removed after 14 d. Patient was followed on a regular basis for duration of 18 mnth with no complications and recurrence. [Technique Diagrammatic Presentation - [Table/Fig-7].
Two distant pilonidal sinuses with planned rhomboids and future flaps on either side. Note the buttocks parted with adhesive tapes

Rhomboid defects and their respective rhomboid flaps
Final defect after the removal of the pilonidal disease
En-bloc resected pilonidal disease

Transposed rhomboid flaps to their respective defects sutured in two layers

Healthy flaps on 3rd day before removal of the drains

Planning and marking of tandem rhomboid flap and the final resulting scar
Discussion
A pilonidal sinus, also referred to as pilonidal cyst or sacrococcygeal fistula, is a cyst near or on the natal cleft that often contains hair and skin debris. It has an incidence of 0.7 % in the general population and affects mainly young males with a peak incidence at the age of 16-25 yrs [1,2].
Treatment varies according to the clinical presentation of the disease. Although many surgical methods have been suggested, an ideal method is still lacking because of high recurrence rates. Recurrent disease causes significant morbidity, particularly missing time from work. Wide excision of the pilonidal disease followed by natal cleft flattening would be an idyllic stratagem remedy for optimal result and reduced recurrence risk. In the aim to achieve this, an assortment of surgical techniques have been illustrated, such as excision & primary closure, excision & open packing, excision & marsupialization, Bascom technique, excision & skin grafting, and flap reconstruction. However, a long list of surgical techniques reflects the inability to find an efficient mode of treatment approved by all surgeons. Main problems associated with the conventional techniques are the high infection and recurrence rate. On the other hand procedures that flatten the intergluteal sulcus and bring the suture line aside midline seem to be superior in terms of postoperative morbidity and recurrence rate [3].
Professor Alexander Alexandrovich Limberg devoted his entire career to flap design [4]. Rhomboid flap is basically a parallelogram with opposing angles of 120° and two of 60°. Four individual flap choices are theoretically possible for any defect. However, the most suitable one is determined by skin laxity in the donor area and surgeon’s preference. Rhomboid transposition flap was introduced in the treatment of pilonidal disease by Azab et al.,[5].
Although the conception of ‘reconstructive ladder’ is that primary closure of a defect followed by skin grafting is the initial choice in reconstruction, it does not hold well in many circumstances. Though defect size is a limiting factor, texture, pliability and colour match of a local flap supports its use. In the treatment of recurrent and complex pilonidal disease, rhomboid transposition flaps are reliable and have a higher success rate. There is little data on treatment of very large (> 12 cm) pilonidal sinuses. The purpose of the present paper is to describe a new technique which demonstrates that instead of a single rhomboid flap, two rhomboid flaps in tandem can be used to close a huge defect following wide excision in treatment of an extensive pilonidal sinus of the sacrococcygeal region. To cram a rhomboid defect with similar tissue of good vascularity, the versatility of a rhomboid transposition flaps is that a random pattern flap can be heaved from any of the four corners.
This is the first description of the use of two tandem rhomboid flaps for very large recurrent pilonidal disease. The above case discussed describing this procedure is one of the 5 cases operated by us and has been detailed with clinical photographs of a single patient. The described technique is a safe and simple choice in treatment of an extensive disease in contrast to any other major reconstruction procedures frequently optioned. It is a very efficient method to flatten the natal cleft and with simple modifications it will displace the incision scar from the midline diminishing skin maceration and debris accumulation and sweating resulting from frictional movements of the buttocks. It allows early return to full activity, does not necessitate prolonged postoperative care and has very low complications rates. Though it’s early to comment on recurrence rate, however, in our 5 case series followed up for duration ranging from 6 to 18 mnth none of them had recurrence. The biggest problem with any treatment for this disease is the risk of recurrence. Various operations that have been tried in the past in an attempt to minimize the risk of recurrence have an unacceptable recurrence rate. In our case the postoperative outcome after the procedure was excellent for an extensive disease. The advantages of this Tandem Rhomboid Transposition in pilonidal sinus are:
Technical ease to learn and perform when planned well
Short operation time
Recruitment of tissue for covering the 2 rhomboid defects is on either side of the midline from two different areas thus preventing the necessity to extensively mobilize larger flap from a single donor site
Decreased pain and discomfort in the wound area – compared to open techniques
Low risk of wound infection
Does not necessitate prolonged postoperative care like frequent change of dressings in ‘lay open’ and skin grafting techniques
Early functionality with short convalescence period
Short healing period
Decreased follow-up duration in regard to concern with the flap
Early return to full activity
Lower complication and recurrence rates
Aesthetically more acceptable since skin texture and color are similar due to recruitment of tissue around the defect.
Shortcomings of the procedure include random pattern blood supply with limited length of the flap, donor site closure may sometimes distort surrounding structures, donor region skin extensibility should be significant and flap may not give enough bulk for deep defects. Also, the procedure should be weighed against other procedures while considering it in younger patients or when the skin is dense as it may result in difficult closure resulting in bulges, dog ears and surrounding tissue distortion.
A well-planned tandem rhomboid flap with scars parallel to tension lines provides the best results and success for an extensive pilonidal sinus disease but as in any local flaps, depends on the pliability of the adjacent skin.
[1]. Armstrong JH, Barcia PJ, - Pilonidal sinus disease: the conservative approachArch Surg 1994 129:914 [Google Scholar]
[2]. Bulent Mentes B, Leventoglu S, Cihan A, Tatlicioglu E, Akin M, Oguz M, Modified Limberg flap transposition flap for sacrococcygeal pilonidal sinusSurg Today 2004 34:419 [Google Scholar]
[3]. Cihan A, Mentes BB, Tatlicioglu E, Ozmen S, Leventoglu S, Ucan BH, Modified Limberg flap reconstruction compares favourably with primary repair for pilonidal sinus surgeryAust N Z J Surg 2004 74:238 [Google Scholar]
[4]. Gibson T, Modern Trends in Plastic Surgery 1964 LondonButterworths [Google Scholar]
[5]. Azab ASG, Kamal MS, Saad RA, Radical cure of pilonidal sinus by a transposition rhomboid flapBr J Surg 1984 71:154 [Google Scholar]