Hepatoblastoma is the most common primary liver tumor of childhood and after neuroblastoma and nephroblastoma the third most common abdominal neoplasm in this age group. Hepatoblastoma is an embryonal tumor classified by histology as epithelial (including pure fetal subtype, mixed embryonal/fetal subtype, macrotrabecular subtype and small cell undifferentiated subtype), mixed epithelial and mesenchymal type (with teratoid and non-teratoid features) and hepatoblastoma not otherwise specified.
We present a case of a five-months old girl with embryonal/fetal subtype hepatoblastoma. The clinical presentation was asymptomatic abdominal mass. Ultrasound and MRI scan demonstrated a solid hepatic tumor. She presented thrombocytosis and serum alpha-fetoprotein was increased. A left lobe hepatectomy was performed and the pathological examination revealed complete excision of a mixed embryonalfetal subtype hepatoblastoma.
Case Report
We present a case of five months old female infant hospitalized for the evaluation of an abdominal mass. The infant was born mature and prenatally, perinatally and family history were insignificant. The physical examination at hospitalisation revealed an infant with very good general status without fever. At the abdomen examination revealed a palpable mass in the epigastric area and over the midline in the left abdomen under the rib border without pain and with relatively smooth surface.
Laboratory investigations revealed thrombocytosis and high values of the serum alpha-fetoprotein (AFP) >35350ng/ml, betahuman chorionic gonadotropin (βHCG) < 0.605 mIU/ml, lactate dehydrogenase (LDH) 991 U/I, ferritin 163.44 ng/ml, c-reactive protein (CRP) 1.89 mg/dl, aspartate aminotransferase (AST) 74 U/I, alanine aminotransferase (ALT) 19 U/I, gamma-glutamyl transpeptidase (GGT) 252 U/I, hematocrit (Ht) 37%, hemoglobin (Hb) 11g/dl, platelets (PLT) 834000/mm3. We excluded the infection with B and C hepatitis viruses.
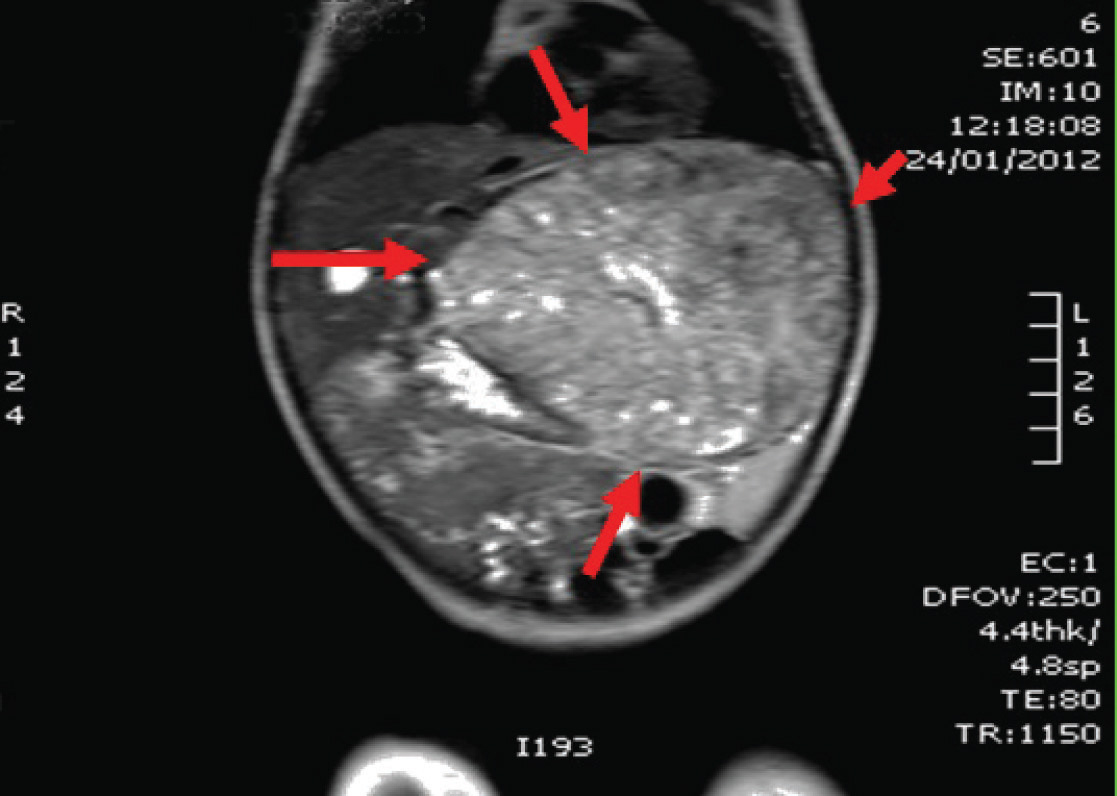
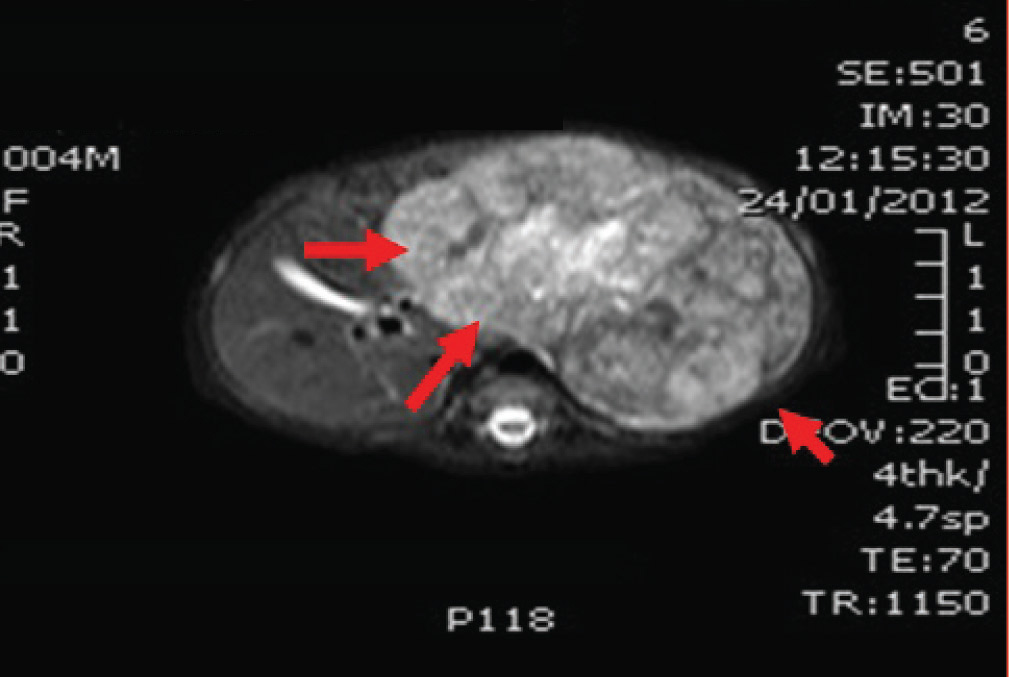
The abdominal ultrasound [Table/Fig-1] showed a well-defined tumoral mass with non-homogenous, hypoechogenous parenchymatous structure placed in the left side of liver. The portal and hepatic veins as well as the inferior vena cava did not show tumoral invasion. MRI showed a well-defined tumoral mass of 10x9.7x6.2 cm placed in the II-III segments of liver [Table/Fig-2,3].
The patient’s age, clinical-imaging data, thrombocytosis and high value of AFP raised the suspicion of a hepatoblastoma.
The patient was operated and a well-defined tumor 10/10 cm without vascular invasion was detected in the segments II-III [Table/Fig-4,5]. A left lobectomy (segmentectomy 2 and 3) was performed.


The pathological diagnosis was of embryonal/fetal subtype hepatoblastoma, totally removed. In multiple section received from the tumour, there has been a histological picture of hepatic neoplasm of areas consisting of trabecular solid or rosette like formation with cells with dark staining nuclei and frequent mitosis. There are cells with less atypia among which several foci of hepatopoeiesis. Mesenchymal elements are not recognised. Immunohistochemical analysis showed the neoplasmatic cells were positive to a FP, focally positive to CD99 and negative to S-100.
The postsurgical evolution was favourable. The patient was transferred to the Department of Pediatrics where she tolerated well- treatment with Cisplatin 2mg/Kg for 3 courses every 2 weeks.
Two months after the surgery the clinical biological evaluation was normal without hepatosplenomegaly, normal platelets values and AFP was 823ng/ml. The echographic re-evaluation indicate a hepatic parenchyma without foci lesions.
Discussion
The incidence of hepatoblastoma in USA and Europe seems to be 1.2 to 1.5 cases per million population and the rates in boys (1.57) are higher than in girls (1.09). In all pediatric malignancies it is still a rare tumor, comprising approximately 1% [1–3].
The suspicion of child’s hepatic tumor is based on history, clinical, biological and imaging data.
The clinical presentation usually is an asymptomatic abdominal\ mass and sometimes accompanied with fever, fatigue, anorexia and weight loss. Severe symptoms such as obstructive jaundice and tumor rupture are relatively rare occurrences [1,4].
Laboratory evaluations for suspected hepatoblastoma include blood count, liver function tests, lactate dehydrogenase, alphafetoprotein (AFP), beta-human chorionic gonadotropin (β-HCG), ferritin, carcinoembryonic antigen (CEA), neuron-specific enolase, catecholamines and hepatotrophic viral titers [1,4].
AFP is the most important marker for hepatoblastoma which is increased in 90% of patients. Low AFP levels (<100 ng/mL) are aggressive and associated with a poor prognosis [1]. In neonates the interpretation of AFP measurements is more difficult because of the naturally high serum levels.
There are several environmental risk factors associated with hepatoblasoma. Premature birth and very low birth weight have been found to be associated with the later appearance of hepatoblastoma [1–4].
Oxygen therapy, furosemide, total parenteral nutrition, radiation and other toxins are thought to play a role [1].
A large number of congenital syndromes have been described in patients with hepatoblastoma, but only Edward’s syndrome, familial adenomatous polyposis and Beckwith-Wiede mann syndrome have been clearly shown to increase the risk of hepatoblastoma [1].
Cytogenetic analysis performed on hepatoblastomas investigators have found several alterations with chromosomal gains occurring more frequently than losses. The most common alterations are trisomy 2, 8, 20 [5]. The implementation of whole-genome DNA chipbased technologies led to the detection of many altered genomic regions, of which gain of material on chromosome 2q 13-22, 2q 36-37 and deletions of 2p and 4q were associated with advanced tumors and poor prognosis [5,6].
The diagnosis of hepatoblastoma is suspected in the patient aged between six months and three years old, in the presence of a hepatic tumor, thrombocytosis and a high level of serum AFP. Our patient presented all these pathognomonic associations.
Abdominal ultrasound is the first technique of choice as the initial diagnostic procedure for abdominal mass. Magnetic resonance imaging (MRI), in many centers is the best modality for revealing morphologic details and to differentiate liver tumors. Computed tomography (CT) is essential for the evaluation of pulmonary metastasis [1].
For histologic confirmation of the diagnosis a biopsy is usually taken in patients who do not undergo primary tumor resection [1].
A complete surgical resection remains the mainstay of hepatoblasoma treatment [1]. Our case had a complete excision of the tumor. The hepatoblastoma treatment is relatively standardized, the only controversy matter between the European and American study groups being the time of the surgical intervention. The SIOPEL Group recommends the presurgical chemotherapy followed by the tumoral excision and then a short period of postsurgery chemotherapy. The American study group recommends the surgical intervention when diagnosed (applicable on 50% of the patients) followed by postsurgical chemotherapy [7,8].
The liver transplantation is indicated either initially for the nonexcisable tumor or after the relapse. The AFP level monitoring represents a valuable marker of the response to the presurgical chemotherapy, in the evaluation of the excision result and for the precocious diagnosis of the hepatoblastoma relapse. The complete excision of the tumor determines the decrease of the AFP serum level, which will be normalized after 4-6 weeks [9]. The AFP serum level increases very much before the imagistic demonstration of the tumor relapse. The ultrasound monitoring is compulsory [10].
Conclusion
We believe that the surgical intervention is possible when diagnosed followed by postsurgical chemotherapy remains the mainstay of hepatoblastoma treatment.
[1]. Dietrich von Schweinitz, Hepatoblastoma: recent developments in research and treatmentSeminars in Pediatric Surgery 2012 21:21-30. [Google Scholar]
[2]. McLaughlin CC, Maternal and infant birth characteristics and hepatoblastomaAm J Epidemiol 2006 163:818-28. [Google Scholar]
[3]. Birch JM, Epidemiology of pediatric liver tumors, in Zimmermann A, Perilongo G, Malogolowkin M, von Schweinitz D (eds)Pediatric Liver Tumors 2011 HeidelbergSpringer:15-26. [Google Scholar]
[4]. Meyers RL, Pediatric liver tumors in Pizzo PA, Poplack DG (eds)Principles and Practice in Pediatric Oncology 2011 PhiladelphiaLippincott. William Wilkins:838-60. [Google Scholar]
[5]. Kappler R, von Schweinnitz D, Molecular aspects of hepatoblastoma, in Zimmermann A, Perilongo G, Malogolowkin M, von Schweinitz D (eds)Pediatric Liver Tumors 2011 HeidelbergSpringer:27-42. [Google Scholar]
[6]. Arai Y, Honda S, Haruta M, Genome-wide analysis of allelic imbalances reveals 4q deletions as a poor prognostic factor and MDM4 amplifi cation at 1q32.1 in hepatoblastomaGenes Chrom Cancer 2010 49:596-609. [Google Scholar]
[7]. Perilongo G, Shafford E, International Society of Paediatric Oncology-SIOPEL 2. Risk-adapted treatment for childhood hepatoblastoma;fi nal report of the second study of the ISPO-SIOPEL 2Eur J Cancer 2004 40:411-21. [Google Scholar]
[8]. Ortega JA, Randomized comparison of cisplatin/nincristine/5-fl uoracil and cisplatin/continuous infusion Doxorubicin for the treatment of pediatric hepatoblastoma (HB): a report from the Children’s Cancer Group and the Pediatric Oncology GroupJ Clin Oncol 2000 18:2665-75. [Google Scholar]
[9]. Kubota M, Yagi M, Kanada S, Effect of postoperative chemotherapy on the serum alpha-fetoprotein level in hepatoblastomaJ Pediatr Surg 2004 39:1775-78. [Google Scholar]
[10]. Daniela Iacob, Mixed hepatoblastoma in child. Case reportMed Ultrason 2010 12:157-62. [Google Scholar]