Introduction: Rise of hypertension among younger age group has increased the prevalence of intracranial haemorrhage. Conflicting reviews regarding the mode of treatment has been a concern to the treating physicians especially in a developing country like India. This study was undertaken to underline the importance of management and propose a local protocol for primary supra-tentorial haemorrhage.
Materials and Methods: Patients presenting with primary supratentorial (ST) haemorrhage fulfilling inclusion criteria are included in the study. Decompression craniotomy done in all the patients and the patient particulars noted. The primary outcome of death is correlated with various particulars and statistical analysis done with SPSS version 16.
Results: Mean age of presentation was 54.2 years, ranging from 38-71years. Male comprised 82.1% (23 patients). Seven out of eight patients with Glasgow coma scale (GCS) ≤7 (87.5%) expired whereas only 3 out of 20 (15%) patients with GCS >7 expired. 50% of the patients with intracranial haemorrhage (ICH) in temporo-pari et al., (2/4) or in basal ganglia with cortical extension (5/10) expired whereas the mortality in cases of ICH in parietal lobe and frontal lobes were 25% (1/4) and 20% (2/10) respectively. Clot volume ≤100ml had a mortality of 19% (4/21) whereas the mortality was as high as 85.7% (6/7) with clot volume >100ml.
Conclusion: Emergency Craniotomy and Evacuation of the Hematoma could be a feasible option in between 40 ml to 100ml of Primary ST ICH without intra-ventricular extension. In cases of intra-ventricular extension of haematoma surgery is less helpful. Midline shift of 5 mm or more might be a poor prognostic factor.
Introduction
Various studies on surgery, in comparison to conservative management, in cases of primary intracranial haemorrhage (ICH) have given conflicting results. Spontaneous ICH is known to have higher mortality rate among various causes of stroke and predominantly affects younger age group.
The high prevalence of chronic kidney disease in local population of Manipur not only increases incidence of non-traumatic ICH but also forms a major factor predicting mortality.
This study was undertaken to underline the importance of management and propose a local protocol for a resource constraint setup.
Materials and Methods
Study design: Cross-sectional study.
Study duration: January 2011- March 2014.
Patients with primary supratentorial (ST) haemorrhage, volume of bleed > 40mL, Glasgow coma scale (GCS) ≥5, haemorrhage close to the cortex (≤1cm) were included.
Whereas, patients with secondary intracranial haemorrhage, infratentorial haemorrhage, volume of bleed < 40mL, refused to give consent for surgery, hematoma deeper than 1cm from cortex and GCS <5 were excluded from the study.
Volume of haemorrhage was calculated using the formula “volume = abc/2”, where a ,b and c stand for maximum measurements of haemorrhage in cm in 3 dimensions
Sample size: One hundred fifty six patients presented with intracranial haemorrhage (ICH). Of which 96 cases were excluded because of traumatic aetiology, 16 patients had a haemorrhage < 40ml and were excluded. GCS <5 was seen in 12 patients and were excluded from the study. Four patients had infratentorial haemorrhage and they were also excluded. Finally 28 patients satisfying the inclusion criteria were analysed.
All the patients presenting with primary ST haemorrhage fulfilling inclusion criteria were included in the study. All the patient particulars were noted. The option of decompression craniotomy is given to all the patients. The procedure is undertaken for the consenting patients within 36 hours of diagnosis. Decompression craniotomy and evacuation of clot was performed in all cases and if necessary, lax duraplasty was performed. Postoperatively the patients were monitored in intensive care unit (ICU) till the time of extubation.The preoperative and postoperative GCS is noted. Statistical analysis was done with SPSS version 16.
Patient Particulars: Age, sex, history of alcoholism, hypertension, type 2 diabetes mellitus, weight, hemiparesis; preoperative GCS, pulse rate, blood pressure, oxygen saturation (SpO2); Computerized tomography (CT) findings - site, size of haemorrhage, midline shift, depth from cortex; type of surgery undertaken, duration of surgery, Postoperative GCS (1wk). All the patients were followed up for 1month after surgery.
Institutional ethical committee approval was taken before commencing the study.
Results
Twenty eight patients satisfying the inclusion criteria in the study period were recorded and analysed. Mean age of presentation was 54.2 years, ranging from 38-71years. Skewness of 0.1 suggests that the disease was uniformly distributed. Twenty of the total 28 patients belonged to the age-group of 40-60 years and 7 patients in the same age group died in the post-operative period[Table/Fig-1]. Male comprised 82.1% (23 patients) and females 17.9% (5 patients). 9 out of the 10 deaths belonged to male sex [Table/Fig-2].
When outcomes of patients with GCS ≤7 was compared with those with GCS>7 its observed that 7 out of 8 patients with GCS ≤7 (87.5%) expired whereas only 3 out of 20 (15%) patients with GCS >7 expired [Table/Fig-3,Table/Fig-4].
When the location of the ICH was compared with outcome [Table/Fig-5], it was observed that 50% of the patients with ICH in temporo-parietal (2/4) or in basal ganglia with cortical extension (5/10) expired whereas the mortality in cases of ICH in parietal lobe and frontal lobes were 25%(1/4) and 20%(2/10) respectively.
Based on clot volume, it was observed that patients with clot volume ≤100ml had a mortality of 19% (4/21) whereas the mortality was as high as 85.7% (6/7) when the volume >100ml [Table/Fig-6].
Discussion
Though ICH accounts for only 10 to 15% of all strokes, it remains most fatal subtype with 40 % mortality [1] . Haemorrhage is classified into primary or spontaneous haemorrhages and secondary haemorrhages based on aetiology. Primary haemorrhages are spontaneous haemorrhages, which are mainly caused by arterial hypertensive diseases. Secondary haemorrhages are due to trauma, tumour or pharmacological causes.
The symptomatology mostly depends on localisation and volume of haematoma often compelling emergency admission. Lobar ICHs are associated with the symptoms localised to affected cerebral lobe, like homonymous hemianopia, paresis of arm or leg, or aphasia and the same were observed in our cases. ICH of basal ganglia as mentioned in literature could be asymptomatic if small and larger ICH in this region leads to sensory-motor contralateral hemiparesis, sometimes in combination with aphasic disorders or homonymous hemianopia. Hence thorough clinical examination holds a key role in order to locate the lesoion. In our study 10 cases had basal ganglia bleed and 5 of them succumbed in their early postoperative period.
The universal availability of CT scan of the brain round the clock makes it as the first choice of imaging modality in the diagnostic work up of such cases. The sensitivity of CT brain has been reported to be more than 95% [2], in our cases CT scan was the only modality of imaging used.
In spite of large randomized trials, the role of a neurosurgery in management of haemorrhagic stroke is a question unsolved even after 100 years. The lack of uniform protocol in primary ICH makes it an open debate for researchers to experiment different protocol in order to conclude in the near future. In STITCH II trial [3], the authors couldn’t find evidence to support the hypothesis that early surgery in comparison to early conservative treatment, in cases of conscious patients with superficial ICH of 10-100ml without intra ventricular extension, improves outcome. Kanaya et al., observed surgical treatment as beneficial in patients with hematoma volume between 20-80ml [4]. However Shahid Siddique quotes that certain meta-analysis of randomized controlled trials (RCT) contradict the usefulness of surgery considering volume as a parameter [5]. On the basis of present study authors propose that, in patients with GCS <7 along with clot volume >100ml or intraventricular extension of haemorrhage the prognosis remains poor in spite of surgical intervention. Whereas, in patients with GCS <7 with clot volume between 40-100ml and without intraventricular extension, the prognosis is slightly better (33%) after surgical intervention. Finally in patients with GCS>7 with isolated lobar haemorrhage of 40-100ml, surgery has a better prognosis (94.2%).
Our patients had a varying GCS at presentation, ranging from (5-11) and Reichart R et al., [6] quotes that patients suffering from medium-sized lobar ICH should undergo surgery, particulary if GCS is below seven.
We had 10 basal ganglia bleed of varying amount and symptomatology with a positive recovery in five patients, but Reichart R et al., [6] opines that small haemorrhages especially of the basal ganglia with small or absent neurological deficits should not be treated surgically.
Surgical therapies described include open craniotomy and evacuation of the hematoma, endoscopic evacuation of the hematoma, CT - guided stereotaxy. The choice of therapeutic modalities adopted depends on local availability and patients’ choice. Though endoscopic evacuation of the hematoma, CTguided stereotaxy sounds technically sound , long term RCTs are awaited to make it as standard of care. Hence craniotomy and evacuation of the hematoma with lax duraplasty is till date the most commonly performed emergency surgery in such cases. The authors also practised open craniotomy in day to day practice with good outcome and all the 28 cases were done by open approach.
In STICH II trial the mortality at 6 months follow-up was 18% in the early surgery group when compared with 24% seen in early conservative group and concluded that early surgery in case of superficial spontaneous ICH has survival benefit [3]. In this background, we had a mortality of 35.7% (10/28) in our study. On analysing the mortality group, basal ganglia bleed with cortical extension (5/10), intraventricular extension (2/10) were the major factors predicting adverse outcome. These factors suggest that patient selection could give a survival advantage in the surgery group.
Showing comparing the outcome in different age groups
| Age group (in years) | Total |
| 31-40 | 41-50 | 51-60 | 61-70 | >70 |
| Outcome | Recovered | 0 | 7 | 6 | 4 | 1 | 18 |
| Expired | 2 | 2 | 5 | 1 | 0 | 10 |
| Total | 2 | 9 | 11 | 5 | 1 | 28 |
Comparing the outcome in relation with sex
| Sex | Total |
| Male | Female |
| Outcome | Recovered | 14 | 4 | 18 |
| Expired | 9 | 1 | 10 |
| Total | 23 | 5 | 28 |
GCS at presentation of all the patients is as depicted in the bar diagram
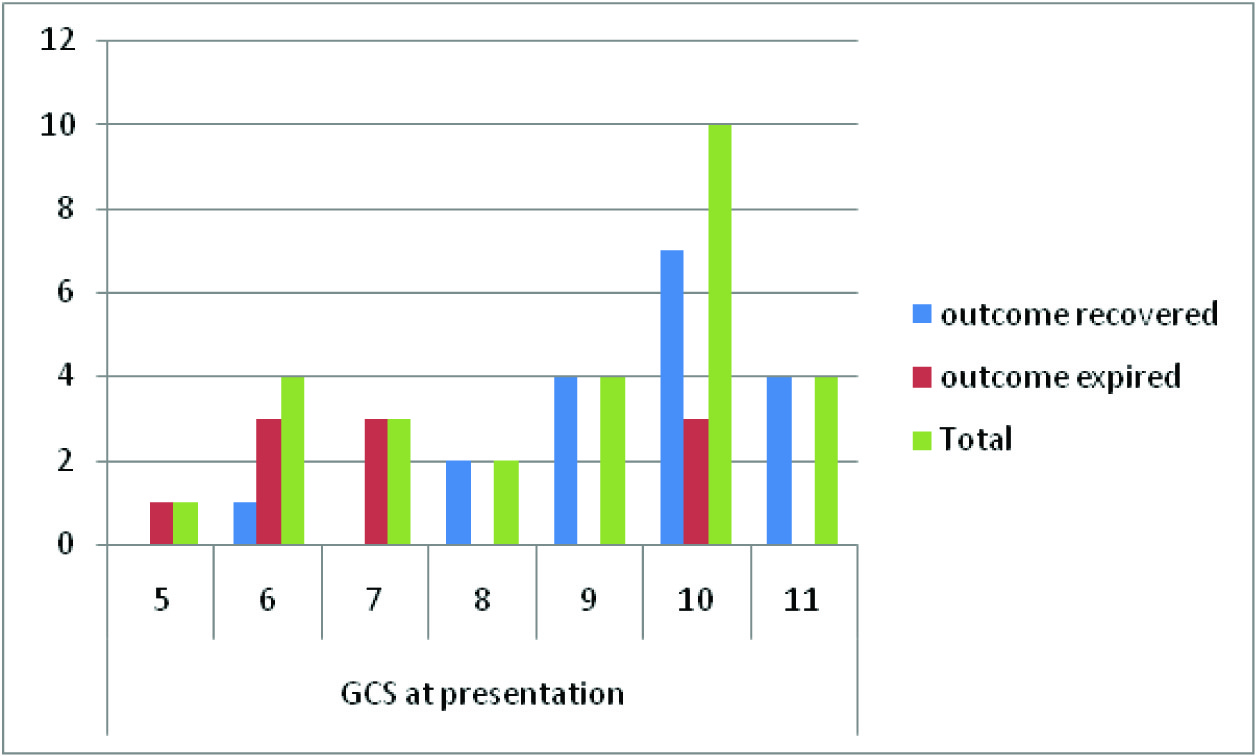
Comparison of outcome in relation to GCS at presentation
| GCS at presentation | Total |
| ≤7 | >7 |
| Outcome | Recovered | 1 | 17 | 18 |
| Expired | 7 | 3 | 10 |
| Total | 8 | 20 | 28 |
Outcome in relation to clot location
| Clot location on CT | Total |
| Frontal | Temporo-parietal | Parietal | Basal ganglia with cortical extension |
| Outcome | Recovered | 8 | 2 | 3 | 5 | 18 |
| Expired | 2 | 2 | 1 | 5 | 10 |
| Total | 10 | 4 | 4 | 10 | 28 |
Outcome in comparison to clot volume
| Clot volume | Total |
| ≤100ml | >100ml |
| Outcome | Recovered | 17 | 1 | 18 |
| Expired | 4 | 6 | 10 |
| Total | 21 | 7 | 28 |
Conclusion
Emergency Craniotomy and Evacuation of the Hematoma could be a feasible option in between 40 ml to 100ml of Primary ST ICH without intraventricular extension. In cases of intra-ventricular extension of haematoma with basal ganglia or any lobe involvement, surgery is less helpful. Midline shift of 5mm or more might be a poor prognostic factor and reiterates the need for surgical intervention.
[1]. MA Kirkman, W Mahattanakul, BA Gregson, AD Mendelow, The effect of the result of the STICH trial on the management of spontaneous supratentorialintracerebral haemorrhage in Newcastle.Br J Neurosurg. 2008 22(6):739-46. [Google Scholar]
[2]. CS Kidwell, JA Chalela, JL Saver, Comparison of MRI aand CT for detection of acute intracerebralhemorrhage. JAMA. 2004 292:1823-30. [Google Scholar]
[3]. AD Mendelow, BA Gregson, EN Rowan, GD Murray, A Gholkar, PM Mitchell, Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013 382:397-408. [Google Scholar]
[4]. H Kanaya, K Kuroda, Development in neurosurgical approaches to hypertensive intracerebral haemorrhage in Japan. In: Kaufman HH..Raven 1992 New YorkIntracerebral Hematomas:197-209. [Google Scholar]
[5]. MS Siddique, AD Mendelow, Surgical Treatment of Intracerebralhemorrhage. Brmed bull 2000 56(2):444-56. [Google Scholar]
[6]. R Reichart, S Frank, Intracerebral. Hemorrhage, indication for surgical treatment and surgical techniques. The Open Critical Care Medicine Journal. 2011 4:68-71. [Google Scholar]