Introduction
Blood has an essential role in patient management within health care systems. Despite the advances in the field of medicine for treating many conditions with synthetic and semi synthetic products, the importance of biological blood products can’t be undermined. Blood is an important resuscitative tool and saves many lives at the times of need. A well organised Blood Transfusion Service is a vital component of any health care delivery system. The blood donors are the backbone of this system. Though blood donation is relatively safe, there are few potentially harmful complications associated with it. These complications are an important reason why the donors fail to return for repeat blood donation. This emphasizes the need of looking into the frequency of the complications and the factors influencing them, so that they can be minimized.
Vasovagal reactions (VVRs) constitute the majority of complications associated with blood donations. These may manifest with mild symptoms like weakness, nausea, sweating, etc or with severe symptoms like total loss of consciousness, seizures etc. Other complications include venous hematomas, arterial punctures, neurological deficits etc. These complications have been reported to have an association with the donor related factors like age, sex, height, weight of the donor, type of blood donation, history of previous donation, etc [1-3].
The aim of our study was to look into the various complications associated with blood donation in our blood bank, their frequency and the possible association with above mentioned factors.
Materials and Methods
An ethically approved, prospective study was carried out at the blood bank of the premiere Indian tertiary care hospital, over 4 months, from January 1st to December 30th, 2010, to keep an account of the various complications before, during or after blood donations. All the necessary details like age, sex, body mass index (BMI), history of previous donation, type of donation (voluntary and replacement), blood groups, amount of blood donated (350 ml or 450 ml) and clinical signs and symptoms of the donors who developed complications and consented for the study were recorded. The patients who had experienced VVR at the time of previous blood donation, apheresis donations were excluded from the study. The donors who developed any complication were followed up for at least two week to assess the late reactions, if any. The recording of data was done by a single, experienced researcher, who acted as an observer and did not interfere with the blood donation process in any way.
The statistical analysis was done by using the SPSS software (version 17, SPSS Inc, Chicago). Analysis was done using univariate analysis, paired t-test and cross tabulations, wherever applicable. A p-value was <0.05 was considered to be significant.
Selection of the blood donors: At our blood bank, the age criterion that defines the blood donation eligibility ranges from 18 to 60 y. Weight of the donor is taken at the time of presentation and it should be more than 45kg. History of any infectious diseases, chronic illnesses or drug usage is ruled out before the selection and it is ensured that the donor had taken food in the last 4h. Potential donor’s pulse rate should be in the range of 50-100. Systolic blood pressure should be between 90-160 mm of mercury and diastolic blood pressure between 50-100 mm of mercury. Hemoglobin should be at least > 12.5 gm. The body temperature should be normal. There should be no evidence of any skin disease, or needle marks at the site of phlebotomy. The donors then sign on an informed consent form. The amount of blood collected is based on the BMI of the donors. 350ml of blood is collected from donors with BMI< 25 and 450ml from those with a higher BMI.
Blood donation is carried out by an experienced phlebotomist, with proper precautions and asepsis.
Definitions of the terms used: Vasovagal reaction (VVR) - According to Standard Operational Procedures guidelines of our blood bank, VVR’s were divided into the following subtypes:
Mild VVR- These manifest as weakness, sweating, dizziness, pallor, slow pulse rate, low BP, cold skin.
Moderate VVR- Symptoms of mild VVR associated with nausea, vomiting or tetany.
Severe VVR- These are characterized by mild or moderate VVR associated with urinary or fecal incontinence, loss of consciousness or convulsions.
VVR’s are also categorized as pre donation VVR’s, those occurring during donation and post donation VVR’s.
Hematoma - Hematoma is defined as a localized collection of blood under the skin associated with swelling, with or without skin discoloration.
Arterial puncture – Accidental puncture of an artery instead of vein. It is characterized by faster blood flow, bright red color of the blood and needle pulsations seen in some cases.
Voluntary donor: A donor donates blood out of his free will without expecting anything of monetary value from the blood bank or patient.
Replacement donor: A member of the family or friend who donates blood in replacement of blood needed for the patient without any monetary or other benefits.
Results
Out of 7450 blood donations, 7118 were from replacement donors, while 321 and 11 were from voluntary and autologous donors, respectively. Total donation associated complications were 74, out of which majority were VVRs (n=48), followed by venous hematomas (n=24) and arterial punctures (n=2). One person had a pre-donation VVR (mild) and was deemed unfit for donation. As the patient did not give his consent, he was excluded from the study.
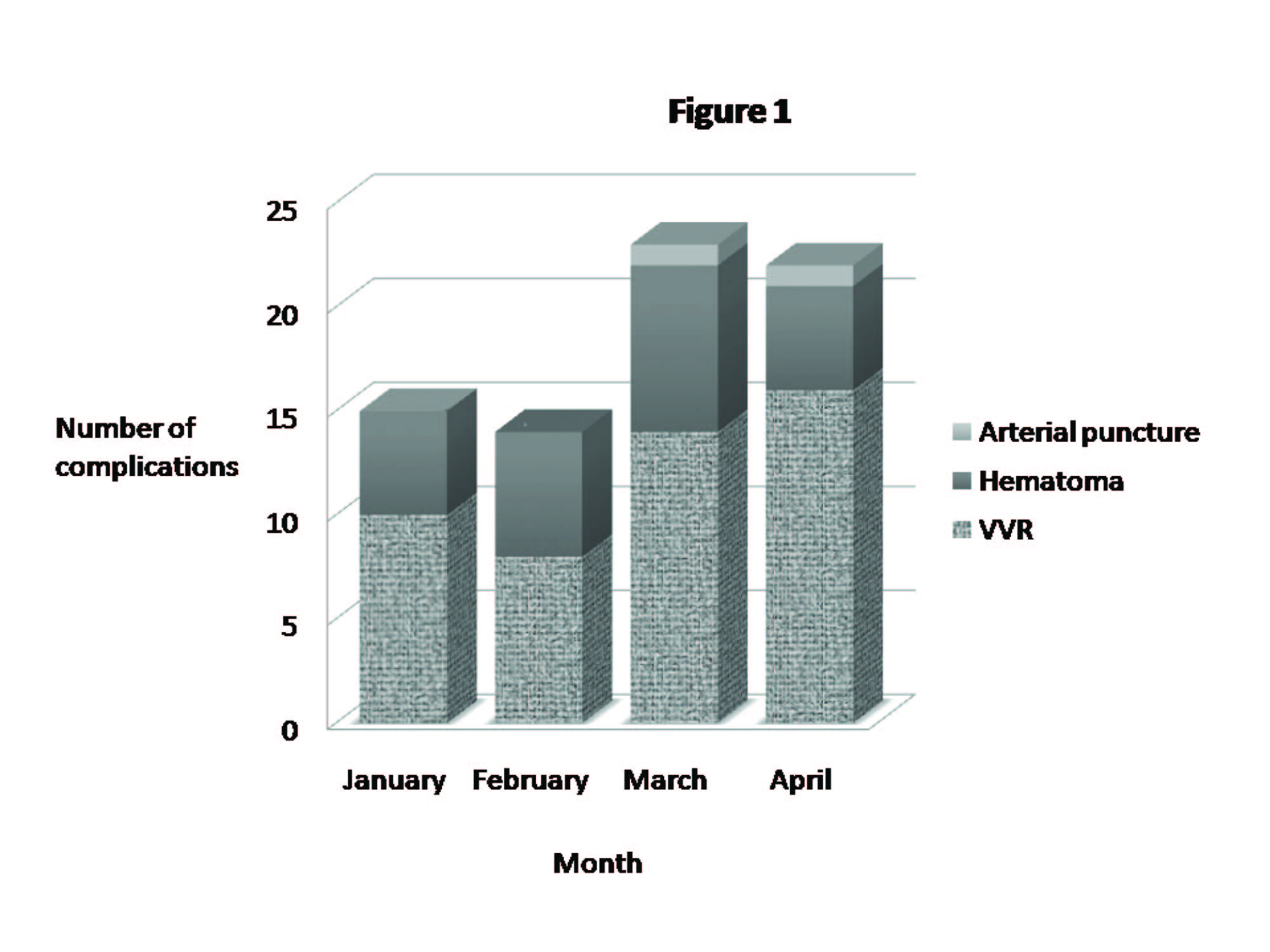
Of the 48 donors who had a VVR after blood donation, the incidence was higher in females (0.68% v/s 0.64%). However, this gender predilection was not statistically significant (p= 0.99). Forty-five of the total VVRs occurred in replacement donors, two in voluntary and one in autologous donor. Though the incidence was higher in the replacement donors, this was not statistically significant (p= 0.5). The incidence of VVRs were higher amongst the donors who had a history of previous blood donation but when compared to the donors who no history of previous donation, this was not statistically significant (p= 0.91). The highest incidence of VVRs was observed in the 21-30 age group though this age specific preponderance was not statistically significant (p= 0.1, univariate analysis). The highest incidence of VVRs were noticed in the donors who had a body-mass-index (BMI) ranging from 18.5-24.9 though even this was not statistically significant (p=0.24). The donors who donated 450ml of blood had significantly higher number of VVRs as compared to ones who donated 350ml (p<0.001). It was also observed that the donors developed more VVRs in the month of April which was statistically significant (p= 0.002, univariate analysis) [Table/Fig-1] .[Table/Fig-2] shows the frequency and distribution of donors with VVRs on the basis of their various attributes.
Mild VVRs constituted the majority of the cases. 44 replacement donors had mild VVR while only one had a moderate VVR. Two of the voluntary donors had mild VVR. One autologous donor also experienced a mild VVR. None of the donors developed severe VVR. [Table/Fig-3] shows the distribution of signs/symptoms of the donors who experienced VVRs.
The mean systolic and diastolic blood pressure and heart rate of the donors before and after the VVR have been summarized in [Table/Fig-3]. It was observed that the donors experienced fall in the systolic as well as diastolic blood pressures along with a fall in the heart rates. This fall was highly significant in the donors between the age group of 21-40.
Twenty four donors developed hematomas during/after blood donation of which 8 donors had to undergo a second/repeat phlebotomy due to the blood stasis in the transfusion set during blood donation. [Table/Fig-2] shows the frequency and distribution of donors who developed hematomas on the basis of their various characteristics. The females had higher incidence of hematoma as compared to males but this was not statistically significant (p= 0.54). Hematomas developed more frequently amongst voluntary donors as compared to replacement donors although this was not statistically significant. Repeat donors had higher incidence of hematomas which, when compared to the incidence in the first time donors, was statistically significant (p<0.001). Hematomas were more often seen in the age group of 41-50 as well as in those who had a BMI less than 18.5 though both of them were not statistically significant (P-value 0.08 and 0.27, respectively). People who donated 450ml of blood had higher incidence of hematoma formation but this was not statistically significant as compared to the incidence in those who donated 350 ml of blood (p= 0.06). Significantly lower number of hematomas occurred in donors in the month of January (p= 0.004) [Table/Fig-1] .
Two donors had inadvertent arterial punctures. None of them had any immediate complications like hematoma, vasovagal reactions etc [Table/Fig-4]. Shows the donor characteristics, why the arterial puncture was suspected and the duration in which the blood donations were performed in these cases.
None of the donors had any neurological deficits due to inadvertent neural damage. No deaths related to blood donation were reported during this period [Table/Fig-5].
All the donors who developed any of the above mentioned complication were followed for at least two weeks. There were no delayed complications.
Discussion
Our hospital has over hundred and fifty thousand admissions per year. The high demand for the blood products can very well be estimated considering the high patient load. The average number of donations at our blood bank range from 60-90 donations per day. The donor, who donates his blood for someone else, should be respected. The safety and well being of the donor is of paramount importance and every step is to be taken to minimize the complications or injuries inflicted on him/her due to the process of blood donation.
Though blood donation is safe, it still carries risk of potential complications. Donation related complications, even mild ones, were found to be 0.99% of the total donations in our study. VVRs were the most frequently encountered of all the complications (64.9%) followed by venous hematomas (32.4%) and arterial puncture respectively (2.7%). In a study done in Italy, the total complication rate was reported to be 0.28% and VVRs constituted 71% of the total complications, post blood donation [4]. A study done in Tehran reported the overall complication rates to be 13.4%, though they studied only the vasovagal complications [5].
VVRs are caused by a reflex of the parasympathetic nervous system, mediated by the vagus nerve, causes the heart to slow down and at the same time, affects the nerves to the blood vessels in the legs permitting them to dilate, leading to lesser blood flow to the brain, thus causing vasovagal syncope (if severe). In the blood donors, they are hypothesized to occur on the sight of blood or due to anxiety and stress levels associated with blood donation. They are also known to occur predominantly in young people [1]. They manifest with symptoms like nausea, dizziness, light headedness, sweating, fainting, loss of consciousness, convulsions etc. On developing VVR, donors are asked to lie down with leg elevated and a free airflow access is ensured. Aromatic spirits of ammonia may be given via inhalation. Hydration status, pulse, BP and heart rate are periodically checked. Use of intravenous calcium gluconate is reserved for the donors who developed tetany.
The reported incidence of VVRs amongst blood donors varies according to different studies. In our study the incidence of vasovagal reactions was 0.64% of the total donations. A study in Pakistan reported it to be as high as 13.2% while it was 0.87% in a study in Greece [1,6]. The reasons for this high variance may be due to the different clinical set-up, nature of the study, threshold of the observer, environmental conditions, heterogeneous study population, racial differences etc. The VVRs most often are mild in intensity. In our study, 98% of the donors with VVRs had mild episodes with varying presentation as mentioned before [Table/Fig-3] . Majority of the donors (95.8%) experienced weakness as the commonest manifestation of VVRs [Table/Fig-5] . Only one donor experienced a moderate reaction, with vomiting and development of tetany. There were no severe reactions. This is in contrast to a study done in India which reports the rates of moderate to severe VVRs to be as high as 7% [3].
An interesting observation was made in our study that significantly more number of overall complications as well as VVRs were observed in the months of March and April as compared to the previous two months. The probable reason for this may be that these are the months when temperature is high as compared to the months of January and February. This could lead to increased perspiration and water loss from the donors leading to dehydration and more chances of developing VVRs and associated complications [Table/Fig-1].
The incidence of VVR has been reported to be associated with age, sex, weight and history of previous donation [1-3]. Tondon et al., found 89% VVR rate in the first time donors, with majority lying between the age group of 31-40 y. Females were found to have 2.5 times higher incidence than males [3]. Zervou et al., also stressed on the high incidence of VVR in first time donors and attributed this to the high stress or anxiety levels [1]. Our study showed higher incidence of VVRs in females, replacement donors, donors with previous history of blood donation, donors in the age group of 21-30 and with a BMI ranging from 18.5-24.9, though these were not statistically significant when compared to their respective counterparts. Our study showed statistically significant association in the incidence of VVRs in donors who donated 450ml of blood. About 90% of the donors who developed a VVR experienced a fall in blood pressure as well as heart rate substantiating the objectivity of the symptoms experienced.
One donor in our study developed a pre donation VVRs, due to which he was declared unfit for the donation process. Newman coined a term epidemic fainting for it, which could be due to the sight of blood or other donors being bled [7].
Hematomas constitute the next important complication of blood donation. A Study in Denmark reported the incidence of venous hematomas to be 33% of all the adverse reactions, which is comparable to our study which shows their incidence to be 32.4% of all the complications [8]. Of the 24 donors who developed venous hematomas following blood donation, 14 donors had thin or hardly visible veins, due to which they underwent blind phlebotomy on the basis of clinical acumen and experience of the phlebotomist. Eight donors had to undergo a repeat phlebotomy. Duration for blood donations for this group varied from 5 to 11 minutes (mean- 8.5 minutes). Our study shows a higher, though statistically insignificant, incidence of hematomas in the 41-50 year age group, donors with a BMI less than 18.5, females, replacement donors, people who donated 350 ml of blood. Statistically significant correlation with the development of hematomas was observed in donors with history of previous donations. Incidentally, less number of hematomas developed in the month of January. The donors were advised to do cold compresses and take serratiopeptidase for three days. Five of the donors came back within a week of blood donation complaining of the skin pigmentation in the phlebotomy area. They were counseled that the pigmentation would subside on its own in due course of time.
Arterial punctures are rare and most often occur due to the blind phlebotomies, faulty technique or inexperienced phlebotomist. A study in Michigan reported this event to be as low as 0.0029% of the total donations [9]. In our study, arterial puncture occurred in two donors (0.027%), which was characterized by a comparatively lesser duration required for the blood donation (mean duration- 3 min), the presence of bright red blood in the collection bag and needle pulsation (seen in one patient). Donors were asked to press the bleeding site for at least 10 min followed by application of tight pressure band aid and were asked to follow up in case of any complications. However, none of them reported with any sequel.
Arm injuries like sore arm, thrombophlebitis, nerve injuries along with long term systemic symptoms of fatigue, iron deficiency are reported to occur as the other few complications following blood donation but none of these were seen in our study [7,8].
Bar chart showing the number of arterial punctures, hematomas and vasovagal reactions occurring during the study period
Frequency distribution of donors with vasovagal reflexes and venous hematomas according to sex, age, type of donation, body mass index, frequency of donation, and amount of blood collected
| Characteristics of Donors | Frequency of Vasovagal reflexes | Frequency of Venous Hematomas | Total Donors |
| Sex distribution | Males | 142 | 66 | 20014 |
| Females | 9 | 6 | 588 |
| Age distribution (in years) | 18-20 | 3 | 3 | 2766 |
| 21-30 | 78 | 6 | 6073 |
| 31-40 | 59 | 31 | 6240 |
| 41-50 | 9 | 29 | 3251 |
| 51-60 | 2 | 3 | 2272 |
| Type of donor | Voluntary | 8 | 10 | 963 |
| Replacement | 143 | 62 | 19639 |
| Body Mass Index [Weight in Kg/(Height in metres)2] | Underweight ( <18.5) | 3 | 12 | 1304 |
| Normal (18.5-24.9) | 104 | 21 | 10408 |
| Over weight ( 25-29.9) | 31 | 30 | 5707 |
| Obese (>30) | 13 | 9 | 3183 |
| History of previous donation | Yes | 38 | 55 | 4426 |
| No | 113 | 17 | 16176 |
| Amount of Blood Collected | 350 ml | 78 | 45 | 18153 |
| 450ml | 73 | 27 | 2449 |
Age wise distribution of changes in systolic, diastolic blood pressure and heart rate after blood donation in patients who experienced a vasovagal reaction SD- standard deviation.
| Age | Mean systolic blood pressure (mm of Hg) | Mean diastolic blood pressure (mm of Hg) | Mean Heart rate |
| Pre donation | Post donation | p-value | Pre donation | Post donation | p-value | Pre donation | Post donation | p-value |
| 18-20 | 124 | 118 | - | 80 | 76 | - | 78 | 70 | - |
| 21-30 | 123.52 (SD=5.26) | 117.84 (SD= 7.76) | <0.001 | 80.3 (SD=6.18) | 76.4 (SD=6.50) | <0.001 | 79.84 (SD= 3.91) | 76.2 (SD=7.23) | 0.001 |
| 31-40 | 125.07 (SD= 10.71) | 116.84 (SD= 8.41) | <0.001 | 79.26 (SD=6.43) | 72.73 (SD= 5.38) | <0.001 | 79.68 (SD= 4.17) | 76.73 (SD= 3.34) | 0.001 |
| 41-50 | 134.66 (SD= 13.6) | 119.33 (SD= 16.1) | 0.157 | 84 (SD=15.1) | 76.6 (SD= 9.45) | 0.173 | 77.33 (SD= 1.15) | 74.66 (SD= 4.16) | 0.270 |
| 51-60 | 135 (SD= 4.24) | 121 (SD= 7.07) | 0.330 | 87 (SD= 1.41) | 65 (SD= 7.07) | 0.170 | 85 (SD= 1.41) | 68 (SD= 2.82) | 0.037 |
Characteristics of the donors with arterial puncture.
| No | Age (in years) / Sex | Bright Red Colour | Pulsatile Needle | Duration of blood donation (in minutes) |
| 1. | 28/Male | Yes | No | 3.5 |
| 2. | 56/Male | Yes | Yes | 2.5 |
| 3. | 57/Female | Yes | Yes | 4 |
| 4. | 24/Male | Yes | Yes | 3.7 |
| 5. | 48/Male | Yes | Yes | 3 |
Frequency of Characteristic signs/symptoms of VVRs occurring in donors.
| Signs/Symptoms of Vasovagal reflexes | Frequency (n) |
| Weakness | 119 |
| Dizziness | 84 |
| Sweating | 68 |
| Headache | 45 |
| Nausea | 33 |
| Vomiting | 6 |
| Loss of Consciousness | 4 |
| Tingling | 3 |
| Convulsions | 0 |
Conclusion
Our study emphasizes on the fact that though blood donation is safe, it still has a complication rate of nearly 1%. Every possible measure should be taken in order to further reduce the rate of complications to encourage people to donate blood at a regular basis. This starts right from spreading awareness about the safety and importance of blood donations along with the discussion of the process with the donors, to alleviate their anxiety related to it. The donor should take adequate sleep a night before donation and should have a proper meal before donation. Strict screening should be done to check the general health status of the donors. The waiting room as well as the donation block can have a television set or light music in background to divert the donor’s attention. The “at risk” donors should be identified and given more medical attention. To avoid the sight of the blood, the collecting bags can be covered, which may decrease the incidence of VVRs. The phlebotomist/physician should have good rapport with the donors and they should try to engage them in conversation to divert their attention. This can ensure high rate of repeat donations by allaying the fears associated with the blood donation, while ensuring the health and safety of the donors