Manual small incision cataract surgery [MSICS] has gained popularity in developing world due to its low cost, speed, safety of surgery, relative ease of learning and outcome comparable to phacoemulsification [1]. Major advantages of MSICS over conventional ECCE are the self sealing tunnel and lesser induced astigmatism [2]. Conventionally, a tunnel of size 5mm to 8mm is used for MSICS [3]. In cases where the nucleus is larger, various techniques for removing the nucleus piecemeal have been described. These techniques need extra instrumentation and have potential serious complications [4,5].
Self sealing incisions are called small incisions if the tunnel length is less than 5.5mm. Junsuke called tunnel of length 5.5 to 7 mm as “relatively large incision” [6]. Larger tunnel of size upto 8mm is considered “large incision”[7]. Large tunnel incision is needed in various settings like hard nucleus, poor mydriasis, pseudoexfoliation, mature or hypermature cataract, subluxated lens, compromised endothelium, etc to facilitate manipulation and easy delivery of nucleus. It is routine to suture large tunnels to maintain tunnel integrity. Large tunnels have disadvantages like wound leak, suturing and higher astigmatism.
With such incision, we could extend its length to “extra large” size of up to 10mm when needed and still have a stable tunnel. In this study we review cases of Extra-large Temporal Tunnel Cataract Extraction [ETCE] for its feasibility and outcomes.
Materials and Methods
Records of MSICS cases performed at our hospital over a period of 3yr between January 2009 and December 2011 were reviewed after taking ethical committee clearance. The study followed guidelines set by the Declaration of Helinski. Written consent was taken from each patient preoperatively.
Cases with temporal incision and tunnel length of 8mm or more were considered for the study. Exclusion criteria were incomplete records, combined surgery, ocular surface diseases including dry eye, Pterygium, long term topical medications, systemic immunosuppressant and previous ocular surgeries.
The database of MSICS cases had 670 records of which 113 records met the criteria set for selection. Of these 17 records were excluded by exclusion criteria. Finally 96 records of 86 patients (10 patients underwent cataract extraction in both eyes) were included in this analysis.
Preoperative data
Age, sex, associated ocular and systemic morbidities, BCVA, grade of cataract (LOCS III classification), keratometry, eye to be operated and IOL power were recorded. Refraction where possible preoperatively and for all postoperative cases and Keratometry were done using an Autorefractokeratometer (ARK). All the cataracts with nuclear grade of NO5 or above, mature and hyper mature cataracts were considered as “dense cataracts” and graded as such during analysis. Axial length was measured using ultrasound A-Scan and contact method. SRK II formula was used for calculation of IOL power.
Surgical procedure
All the surgeries were performed under peribulbar block. The sclerocorneal tunnel was created with a frown incision centered at 9’O (right eye) or 3’O (left eye) clock position. Tunnel was constructed as per our modified technique described above. Tunnel length was decided by the surgeon preoperatively or intraoperatively for each case at his discretion. A rhexis of 6 to 7 mm was made and the nucleus was expressed using sandwich technique. After bimanual I/A through side ports, a rigid IOL of 6mm optic and 12.5mm diameter was placed in the bag. Anterior chamber stability was confirmed. Tunnel length was measured before closing the conjunctiva using Castroviejo caliper and recorded in increments of 0.5mm. Intraoperative complications were recorded.
Post-operative course and data
The patients were started on 1% Prednisolone+ 0.3% Ofloxacin combination on first postoperative day and this was tapered over next 4 to 6 wk. Data was collected at Day 1, one week and six weeks after surgery. At each visit following details were collected - significant symptoms, VA, corneal oedema, AC reaction and keratometry values. In addition, at six weeks BCVA was recorded. All the keratometries were recorded by same optometrist using same ARK. Visual acuities were recorded as Snellen fractions and converted to log MAR for calculation. The data was analysed using SPSS 17.0 for WINDOWS.
SIA was calculated by Holladay method. SIA of individual cases and average SIA were determined as per this technique [9].
Results
The demographic profile is shown in [Table/Fig-1]. Mean age was 64.2 +7.6 yr of which 41(47.7%) of patients were males and 45(52.3%) were females. Right eyes were operated more than left eyes (51/45). Ten patients underwent ETCE in both eyes. There were 13 patients in the study group with other ocular diseases which could lead to reduced visual acuity – including glaucoma and age related maculopathy. Ten study group patients were having systemic diseases including HT, DM, IHD and Asthama.
| Variable | Value |
|---|
| Preoperative Demographic Data |
| No. of eyes (ETCE/Total MSICS cases) | 113/670 |
| No. of eyes excluded | 17 |
| No of Study cases (Eligible/ETCE) | 96/113 |
| No of patients | 86 |
| Age (Mean+SD) | 64.2+7.6 |
| Male/Female (%) | 41/45(47.7/52.3) |
| Preoperative Ocular data |
| Eyes (OD/OS) | 96(51/45) |
| BCVA (Mean) | 6/75 |
| Nuclear density | 4.7+1.1 |
| Associated ocular pathologies-eyes | 13(13.5%) |
| Systemic diseases-patients | 10(11.6%) |
During the 3yr study period, the two surgeons performed MSICS on 670 eyes. 113(16.9%) of these eyes underwent ETCE. 96 (85% of 113) eyes of 86 patients fulfilled study criteria and formed the “study cases”. The average nuclear density was 4.7. Majority of cases (58.3%) had dense cataracts [Table/Fig-1].
Preoperatively BCVA was 1.12+0.54 log MAR. There were 13(13.5%) cases with associated ocular pathologies expected to affect visual outcome. Of these 3 had AMD, 4 had glaucoma and 5 had other pathologies. Ten patients (11.6%) had associated systemic illness. Detailed preoperative data is presented in [Table/Fig-1].
Operative complications occurred in 13 (13.5%) cases. These included one case of tunnel tear requiring suturing, two cases of PCR without vitreous loss and bleeding from tunnel in 10 (10.4%) cases which stopped at the end of surgery. There were no cases with vitrectomy or iridodialysis. None of the cases were left aphakic. These findings are presented in [Table/Fig-2].
| Complication | Value |
|---|
| Operative complications | 13(13.5%) |
| Tunnel tear with suturing | 1(1.04%) |
| Posterior Capsular Rent | 2(2.08%) |
| Bleeding from tunnel | 10(10.4%) |
| Postoperative complications | 7(7.3%) |
| Corneal oedema with <10 DM folds | 7(7.3%) |
| Others | none |
Postoperatively, 7 cases had striate keratopathy on first postoperative day which disappeared by one week. There were no cases of wound leak, persistent corneal oedema or severe iridocyclitis.
At last follow up, none of the cases had corneal oedema. The mean UCVA was 6/14 (0.38 log MAR), with range 6/6 to 6/36 (0.00 to 0.78 log MAR). 50% of these had 6/12 (0.3 log MAR) or better vision and 81.3% had 6/18 (0.48 log MAR) or better VA. No case had vision less than 6/36 (0.78 log MAR) [Table/Fig-3].
| Outcome | Cases (%) |
|---|
| Average Tunnel length | 8.7 mm |
| 8 mm | 16 (16.7%) |
| 8.5 to 9.5 mm | 74 (77%) |
| 10 mm | 6 (6.3%) |
| Average UCVA at 6 weeks | 6/14 (0.38 log MAR) |
| 6/12 or better | 50% |
| 6/18 or better | 81.3% |
| <6/60 | None |
| Average BCVA at 6 weeks | 6/7.5 (0.09 log MAR) |
| 6/9 or better | 93.8% |
| 6/18 or better | 100% |
| SIA at 6 weeks – cumulative data |
| Aggregate SIA | 0.32D @ 850 |
| < 0.5D | 35 (36.45%) |
| < 1.0D | 73 (76%) |
| < 1.5D | 89 (92.7%) |
| >1.5D | 7(7.3%) |
The tunnel length was measured at the end of surgery. The average tunnel length was 8.7+0.3 mm with a range of 8 to 10 mm.
The mean Best spectacle corrected vision (BCVA) was 6/7.5 (0.09 logMAR). 90 cases (93.8%) had 6/9 (0.18 logMAR) or better vision. All patients had 6/18 (0.48 logMAR) or better BCVA.
The aggregate SIA was 0.32 D at 850 with 41 % coherence. SIA had a range of 0 to 3.1D. 76% of cases had SIA <1.0D and 92.7% had SIA < 1.5D.
Thus, ETCE cases had dense cataract requiring a larger tunnel. Even with such large tunnel none had leak, shallow anterior chamber or postoperative blebs, indicating a secure tunnel. There was no excessive uveitis or corneal oedema. Overall, the BCVA of ETCE cases was excellent with all cases having 6/18 or better vision. Most of the cases had SIA of one diopter or less.
Discussion
In this study we are describing for the first time, use of tunnel size of up to 10mm for cataract extraction. In all the cases except one, the tunnel was self sealing. In this case suturing was done due to tear in tunnel during construction. This patient had normal outcome postoperatively with 6/6 BCVA at 6wk.
During difficult situations, it is common to extend scleral tunnel beyond 7mm length and place one or two sutures at the end of surgery. A large self-sealing tunnel with low SIA is desirable in such cases. We intend ETCE method to reduce complication rates and provide a secure tunnel at the end of procedure. Other authors have also noted that larger tunnels can be self-sealing [3,7] [Table/Fig-4].
Comparison with other studies
| Study * | No of cases (n) | Tunnel length (mm) | All parameters are in percentages | SIA (D) |
|---|
| Dense Cata-ract † | Com-plicat-ions ‡ | UCVA ( >6/18) § | BCVA ( >6/18) § | BCVA( >6/9) § |
|---|
| Present study | 96 | 8 – 10 | 58 | 20.8 | 81.3 | 100 | 93.8 | 0.32 |
| Lam et al., [7] | 50 | 8 | NA | 28 | 56 | 100 | 74 | 0.69 |
| Venkatesh et al., [10] | 102 | 6.5 – 7.5 | 100 | 30.4 | 78.4 | 97.1 | NA | 0.72 |
| Ruit et al., [1] | 54 | 6-7 | 100 | 29.6 | 89 | 98 | NA | 0.88 |
| Venkatesh et al., [11] | 100 | 6-6.5 | 100 | 29 | 77 | 99 | 94 | NA |
| Hennig A et al., [12] | 500 | 6-8 | 32 | 17.2 | 70.5 | 96.2 | NA | 1.41 |
*: MSICS arm of study if study includes more than one surgical technique
†: NO5 or more, brunescent, black, mature and hypermature cataract
‡: Operative and postoperative complications up to 6 weeks
§: At six weeks or more postoperatively
The mean UCVA at 6wk was 6/15. 81% of eyes had UCVA of 6/18 or better [Table/Fig-3]. This falls short of WHO target of 90% or more but is comparable to other studies of MSICS [Table/Fig-4]. All the patients had vision of > 6/36 at six weeks postoperatively. The mean BCVA was 6/7.5. In 94% of cases the BCVA was 6/9 and all cases had 6/18 or better vision with correction. We could get only one study of MSICS on dense cataract with BCVA of 6/9 comparable to ours [12]. This exceeds WHO standards and is better than previous studies [Table/Fig-3].
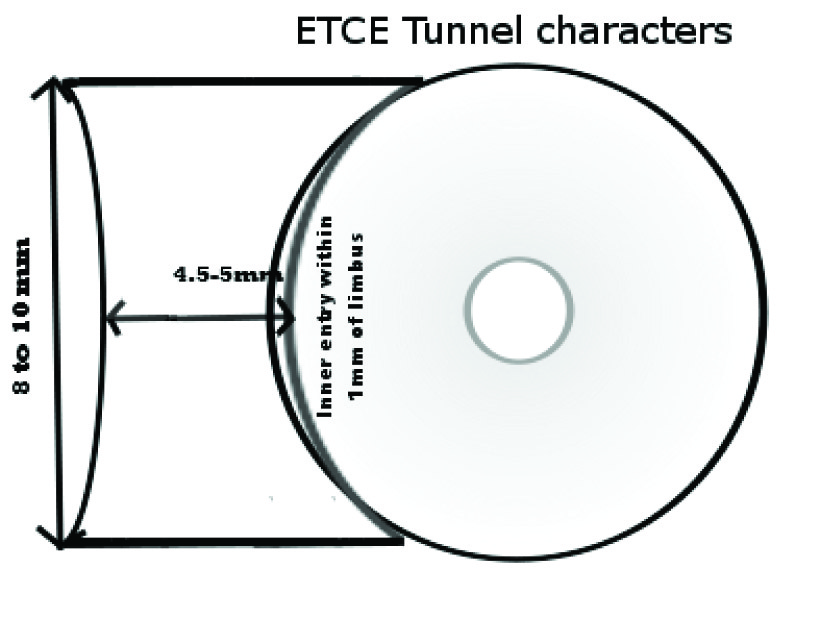
The mean tunnel length of 8.7mm is 32% more than conventional size of 6.5mm. The intended tunnel width of 4.5-5 mm is 28-43% more than conventional size of 3.5mm [Table/Fig-5]. We had not recorded the indication for extra large size of tunnel in all cases. The mean nuclear grade of 4.7 reflects majority of cases had dense cataracts. About 86% of cases in our study had a nuclear grade of NO4 or more. We feel this is the main reason for larger tunnel length in our study. In developing countries patients usually present with denser nuclei [10–12]. Extra-large tunnel is suitable for such cases.
Extra large tunnel features
The overall complication rate in our study was about 21% [Table/Fig-2]. The major intraoperative complication was bleeding from tunnel (10%). Rates of 9-29% bleeds have been reported in other studies [1,12]. Another important complication was mild striate keratopathy. In evaluation of MSICS for black and brunescence cataracts (BBC) Venkatesh et al., recorded corneal oedema in 19.6% of cases as compared to 7.3% in present study. In our study at one week follow up, all the corneas were clear, indicating minimal insults to endothelium or hydration of cornea as cause of SK on day one. Posteriorly placed inner entry in our study may have contributed in reducing endothelial insult by providing more room for passage of nucleus and prevented nucleus scraping endothelium.
When compared to other studies involving various incision sizes and dense cataracts we found many surprises [Table/Fig-4]. Our study had better UCVA than most of the studies. The overall complication rates were nearly 35% more in most of studies with smaller incision. Five studies including ours had recorded SIA. Our method shows lowest SIA (0.32D) among all five, reflecting advantage of having posteriorly placed and wider tunnel. The SIA also depends on method used for calculation and hence this comparison may not reflect true outcome in some of the studies.
The aggregate SIA of 0.32D is low for the tunnel length. Majority of cases had SIA of 1.0D or less [Table/Fig-4]. With 81% of UCVA of 6/18 or better, lower complication rates than smaller incisions and low SIA, this method can be considered for routine use for cataract extraction.
Two major factors affect SIA, the length of tunnel and location of external incision in relation to corneal centre. In conventional MSICS tunnel is made funnel shaped for ease of nucleus delivery and to reduce the incision size. For very hard nucleus where the nucleus can be as large as 8 to 9 mm [13] a 6-7.5 mm tunnel can have complications like nuclear fracture and marked endothelial damage during delivery. It is logical to make larger incision and avoid such complication. Hence, the extra large tunnel of 8 to 10 mm size. The SIA can be reduced by placing the incision farthest from cornea. This can be achieved by shifting to temporal site [6,7], placing incision more posteriorly on sclera and also shifting the inner entry posteriorly as we did in our cases.
We also chose to construct the tunnel using only keratomes and single sweep technique. Here, we use a 3.2mm keratome to create the tunnel and inner entry by passing it in single continuous stroke preventing irregular damage to collagen fibres. A 5.2mm keratome is used to extend the tunnel thus created by single inward stroke of blade for regular cuts and to prevent collapse of AC [Table/Fig-6]. We believe this reduces excessive scarring and hence reduces SIA. But, for the inexperienced surgeons, it is easier to construct these tunnels with a crescent blade followed by entry and extension with keratome which can minimize trauma to tunnel flaps.

ETCE tunnel differs from that of MSICS in its configuration [Table/Fig-5]. In ETCE, tunnel has parallel sides whereas MSICS tunnel is funnel shaped. As the outer lip has same length as inner lip, the stress on it during manipulations is minimal. Conventional MSICS extends about 1.5 to 2 mm into cornea whereas here it is less than 1mm. The outer incision is frown with more posterior location, bringing it nearer to the astigmatic funnel. The SLIMCE incision demonstrated by Lam et al.,[7] is 8mm externally and 9-10 mm internally, but extends into cornea for 2mm which results in higher SIA (0.69D) than ETCE incision (0.32D). SIA in both the studies is calculated using Holladay technique and hence comparable.
There are many advantages to making an extra large tunnel. The creation of such tunnel using our technique ensures less injury to endothelium and secure tunnel. Same surgical technique can be used irrespective of the difficulty involved in individual cases making it universally applicable. Switching to this technique does not demand extra training for surgeons well versed with MSICS; while for a fresh learner the construction of such tunnel gives wide safety margin for remaining steps of surgery. The nucleus can be safely delivered even by an inexperienced person. An important application of this method is - ETCE tunnel architecture can be used for MSICS by reducing tunnel length. This can further reduce SIA. The tunnel can be still extended to extra large size at any stage of surgery.
Construction of tunnel of such width has its own problems. This tunnel cannot be constructed superiorly as manipulation is severely restricted by orbital rim. Surgeons without experience of operating through temporal position may find it difficult to manipulate through wide tunnel and more horizontal approach required during instrumentation. A keratome of short length will not suffice for making tunnel of 4.5 to 5 mm width. We had to select a 3.2 keratome of 8 mm tip length [Table/Fig-6] to avoid damaging the outer lip of tunnel. Aspiration of sub-incisional cortex is difficult, which is also the case in conventional MSICS, but can be circumvented by single or bimanual I/A through side ports.
This study is limited by duration of follow up. Though, SIA is acceptable at 6wk, further decay of astigmatism over longer duration has not been presented. The indication for extra large tunnel size was not recorded in this study. We could not ascertain the cause for SIA of >1.5D which occurred in seven cases. Further, study is needed to look for other factors resulting in such high SIA. Comparison with MSICS cases by same surgeons was not done. A case – control comparison of MSICS and ETCE will determine the indications, significance of SIA and complication rates between the two methods.
Conclusion
For the surgeon operating on dense nucleus, various options are available to express the nucleus through a self sealing tunnel. We have described a new method with extra large tunnel length for all types of nucleus. The complication rates and BCVA of this technique are comparable to other methods of MSICS. UCVA and SIA seem to be better than other MSICS studies. Thus, ETCE seems to be a safe alternative to MSICS.
*: MSICS arm of study if study includes more than one surgical technique
†: NO5 or more, brunescent, black, mature and hypermature cataract
‡: Operative and postoperative complications up to 6 weeks
§: At six weeks or more postoperatively