Insulinoma: A Comprehensive Summary of Two Cases
Pankaj Sharma1, Sonia Sharma2, Shivani Kalhan3, Bhanu Pratap Singh4, Sonam Sharma5
1 Professor, Department of Radiodiagnosis, Army Hospital (Research & Referral), Delhi Cantt, India.
2 Assistant Professor, Department of Pathology, Army College of Medical Sciences, Delhi Cantt, India.
3 Professor and Head, Department of Pathology, Shaheed Hasan Khan Mewati, Government Medical College, Nalhar (Mewat), India.
4 Resident, Department of Radiodiagnosis, Army Hospital (Research & Referral), Delhi Cantt, India.
5 Senior Resident, Department of Pathology, Shaheed Hasan Khan Mewati Government Medical College, Nalhar, (Mewat), India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shivani Kalhan, B 44, Sector 36, Noida, Distt-Gautam Budh Nagar (UP)-201303, India. Phone : +919818 676 354 E-mail : shivani_kalhan@yahoo.co.in
Pancreatic endocrine tumours are rare in occurrence. They may present with a baffling range of symptoms which pose a diagnostic dilemma. Two cases of pancreatic insulinoma are presented herewith. Both presented with neuro-psychiatric complaints and were treated symptomatically for depression, anxiety, seizures etc. The diagnosis in these patients was missed for years. Insulinoma being a great diagnostic challenge, requires reasonably high clinical suspicion, accurate biochemical diagnosis and radiological localization to avoid extensive surgery. The aim is to highlight the occurrence of this rare tumour at a tertiary care hospital.
Insulinoma, Neuropsychiatric presentation, Spontaneous hypoglycaemia
Case Reports
Case 1
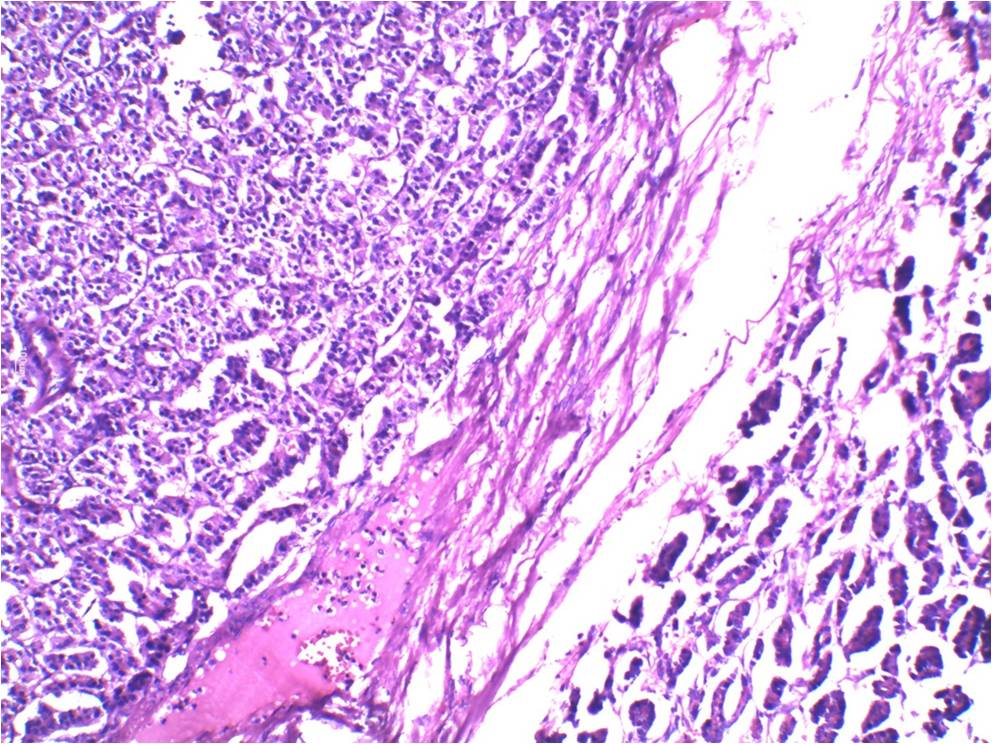
A 40-year-old housewife, resident of Delhi, India, presented with the complaints of weight gain, recurrent episodes of dizziness since two years, sweating & palpitation. She also had anxiety, palpitation & uneasiness. She had gained more than 20 Kg weight in last twoyears and had consulted various specialists including psychiatrist for depression. There was no history of polyuria, polydipsia, polyphagia; episodic headache, palpitation; swelling in the neck or eyes; renal stones, recurrent fractures; visual field defects, headache; acral enlargement or galactorrhea. She had normal regular menstrual cycles and had history of primary hypothyroidism since 16 yrs. She was also a known hypertensive since 12 yrs. She was on tab eltroxin 200μg OD, tab losartan 50 mg BD, tab amlodipine 05 mg OD and tab indapamide SR 1.5 mg OD. Her general and systemic examinations were within normal limits. There were no features of Cushing’s syndrome. Her basic biochemical investigations were also within normal limits. During the episode of spontaneous hypoglycemia in the ward, her blood glucose was 46 mg/dl; serum insulin: 28.96 μIU/ml; C peptide: 16.29 ng/ ml and cortisol was 18.84 ug/dl. Contrast enhanced MRI abdomen showed a complex solid cystic mass lesion (40x45x45mm) in tail of pancreas possibly infiltrating left kidney; likely to be of neoplastic etiology. PET CT revealed mass lesion in tail of pancreas abutting left kidney [Table/Fig-1]. The patient was managed surgically; exploratory laparotomy with distal pancreatectomy and splenectomy was done. She was closely monitored and managed for hyperglycemia and hyperkalemia postoperatively. Gross examination of the resected tumor showed a partly encapsulated tumour with reddish brown cut surface. Histopathological examination revealed a pancreatic neuroendocrine tumour with clear margins [Table/Fig-2]. Immunohistochemistry of the same showed Ki 67 index < 1 %, suggestive of low grade well differentiated tumour with strong positivity for chromogranin and weakly positive CD56. Post operatively, the patient did not have any symptoms of hypoglycemia and lost 13 kg weight.
PET CT: Mass lesion in tail of pancreas, abutting left kidney

Well defined, circumscribed tumour margins. H&E; 200X
Case 2
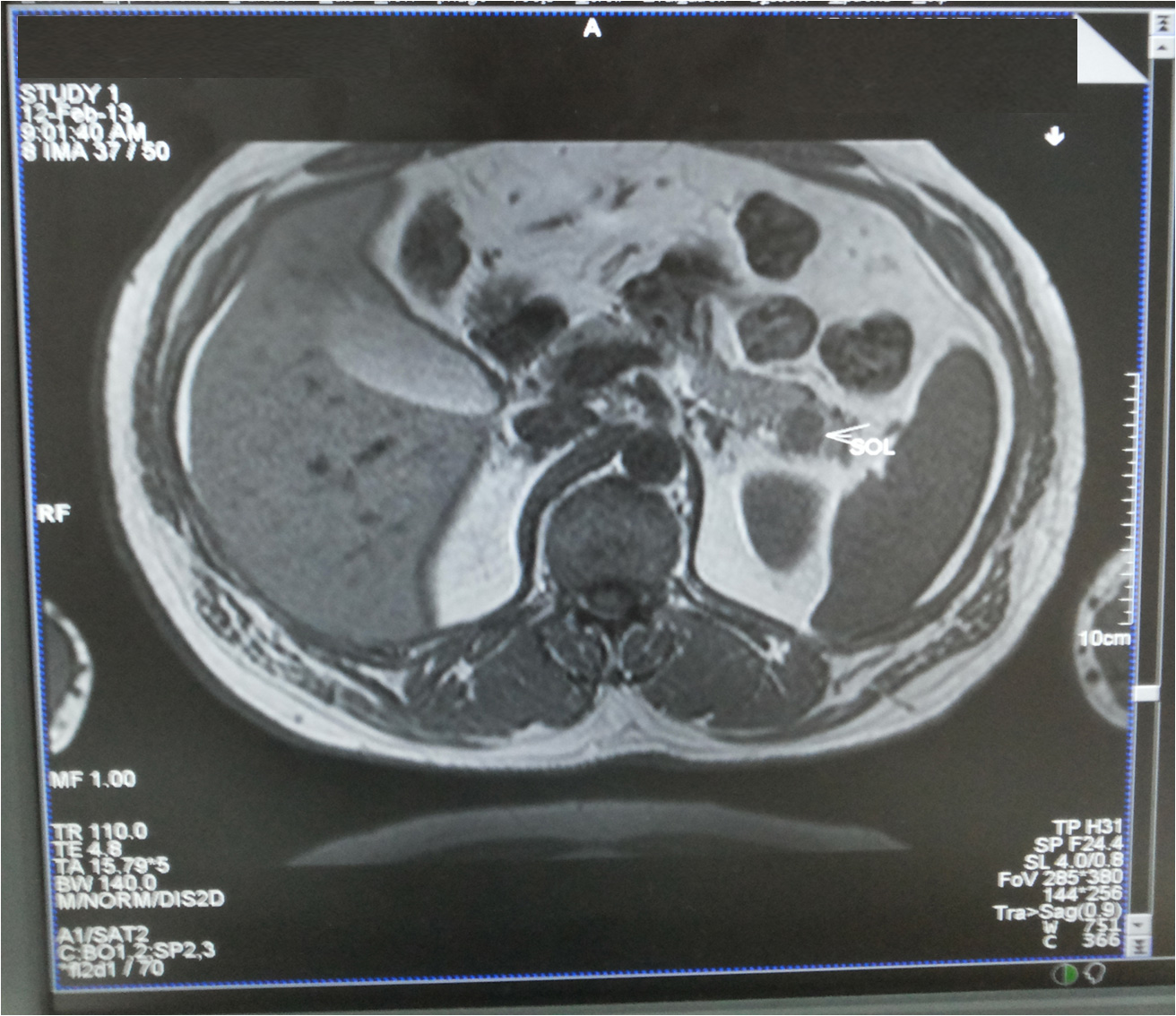
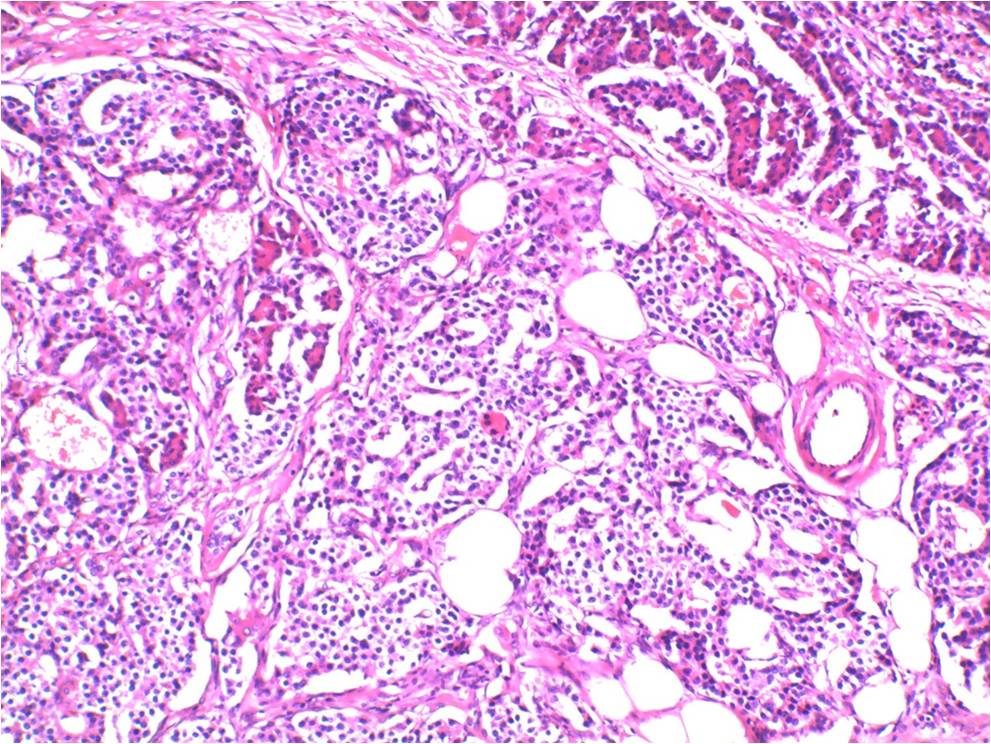
A 52-year-old man presented with the history of recurrent episodes of violent behaviour since 4-5 years. He had the symptoms mostly early morning between 0300 – 0500 hrs. They were relieved on eating food. The patient consulted a neurologist who started him on anti epileptics with a diagnosis of ?seizures. The patient remained on anti epileptics for 4 years. Meanwhile, he gained 28 kg weight in 4 years. These episodes were not associated with any sweating, palpitations. They were associated with increased appetite. The two documented episodes of generalized tonic clonic seizures requiring admission in another hospital were associated with a blood glucose of 30 mg/dl. The general physical examination revealed the patient having a height of 174cm and weighing 105Kg, with a BMI of 34.68Kg/m2. There was acral enlargement. Rest of the general and systemic examination was within normal limits. The patient’s baseline investigations were within normal limits. During an episode of spontaneous hypoglycemia with a documented random blood sugar level of 36 mg/dl, the patient was found to have serum insulin of 20.67 μIU/ml with C Peptide levels being 21.23 ng/ml and serum cortisol of 19.5 ug/dl. MRI abdomen showed a moderate but heterogenously enhancing lobulated mass lesion in the tail of pancreas suspicious of an Insulinoma [Table/Fig-3]. The patient had recurrent episodes of hypoglycemia in the ward. He was started on Inj Octreotide 100ug SC 06hrly. Explorative laparotomy with distal pancreatectomy and splenectomy was done. The patient was closely monitored post operatively and managed for hyperglycemia and hyperkalemia. The gross examination of the resected specimen showed a partly encapsulated tumour with grayish brown cut surface. Histopathology revealed pancreatic neuroendocrine tumour with no necrosis, lymphovascular emboli or perineural invasion. Moderate mitotic activity was seen [Table/Fig-4]. The Ki 67 index was < 2 %. On follow up, there was no recurrence of symptoms of hypoglycemia. The patient lost 12 kg weight and his post operative serum insulin levels were 5.44 μIU/ml.
MRI abdomen: heterogenously enhancing lobulated mass lesion in pancreatic tail
Tumour cells with round to oval nuclei with finely stippled chromatin.H&E;200X
Discussion
Pancreatic endocrine tumors are a rare entity with a reported incidence of 4 cases per million [1]. The commonest amongst these is insulinoma, presenting in 4th to 7th decades, predominating in females [2]. Insulinoma may present with symptoms like irrational behaviour, epileptiform seizures and spells of coma which are very alarming. It can pose a huge diagnostic dilemma and remain undiagnosed for years. It may also be erroneously diagnosed and treated as a neuropsychiatric illness [3].
The role of different imaging techniques in the diagnosis is variable. The sensitivity of transabdominal ultrasonography (TAUSG) and abdominal computerized tomography (CT) scanning are low (between 23–63% and 40–73% respectively) as diagnostic procedures. Angiography and transhepatic venography are relatively more sensitive (60–98%) but are expensive and invasive procedures [4]. Endoscopic ultrasonography has a sensitivity of 95% in the hands of skilled operators.
Hypoglycemia in non diabetic individuals is said to be there when plasma venous glucose is <55 mg/dl. For diagnosis of insulinoma, Whipple’s Triad is required to be fulfilled i.e symptoms of hypoglycemia, blood glucose <55 mg/dl and symptoms relieved after ingestion of food [5]. Insulinomas are often difficult to detect as the symptoms generally precede the occurrence of a clinically detectable tumour [6]. Diagnosis of insulinoma may also be delayed because of nonspecific symptoms. Patients with mainly neuroglycopenic symptoms maybe misdiagnosed as epilepsy or neuropsychiatric disease [3]. Both our cases presented with weight gain. While the accompanying symptoms in the first case were sweating, palpitations, anxiety and dizziness; those in the second case were violent behaviour. The symptoms were prominent early morning in both the cases and sometimes at midnight (first case). In insulinomas, hypoglycemic symptoms, hypoglycemia and hyperinsulinism coexist. If the blood glucose level is < 40 mg/dl and the insulin level > 6 μIU/ml, it is diagnosed as hypoglycaemia due to hyperinsulinism [7]. In case of exogenous insulin use, C-peptide levels are useful in resolving the diagnostic dilemma versus insulinoma. High levels of C-peptide indicate endogenous insulin secretion [8]. After confirmation of biochemical diagnosis, the exact preoperative anatomic localization of insulinoma with ultrasonography (abdominal / endoscopic), CT-scan or MRI is imperative before a major pancreatic surgery [7].
Surgery is the treatment of choice for insulinoma. The nature of surgery depends upon the size, location and resectability. Simple enucleation is preferred for solitary, resectable insulinoma, if it is not impinging on main pancreatic duct or a major blood vessel. On the other hand, distal pancreatectomy with or without splenectomy is preferred for multiple insulinomas occurring in the body and tail of the pancreas.Whipple’s procedure (pancreatoduodenectomy) is recommended for non-enucleable insulinomas located in the head and neck regions of pancreas [9]. Chemotherapy with or without radiotherapy is recommended for malignant, irresectable, residual, recurrent or metastatic insulinomas or in patients unwilling/ unfit for surgery [3].
Grossly, insulinomas are well – circumscribed soft lesions, which are often partially encapsulated with a grayish to reddish brown cut surface.
Histopathologic examination can reveal a variety of architectural patterns. These neoplasms may show a solid/diffuse, lobular,or a trabecular/ gyriform appearance, often surrounded incompletely by a fibrous capsule . Occasional cystic and papillary variants have also been described. The neoplastic cells have uniform round to oval nuclei with finely stippled and evenly distributed granular chromatin. The cells almost always lack prominent nucleoli. Amyloid deposits may be seen in the fibrovascular stroma and around the nests of neoplastic cells [10].
Electron microscopy demonstrates the characteristic crystalline beta granules.
Conclusion
Insulinoma can prove to be a great diagnostic challenge. Adequate clinical suspicion followed up by accurate biochemical diagnosis and radiological localization is a must to avoid blind extensive surgery.
[1]. Service FJ, McMahon MM, O’Brien PC, Ballard DJ, Functioning insulinoma: incidence, recurrence and long-survival of patients: a 60-year studyMayo Clin Proc 1991 66:711-19. [Google Scholar]
[2]. Lack EE, Pancreatic endocrine neoplasms. In: Lack EE, editorPathology of pancreas, gallbladder, extrahepatic biliary tract and ampullary region 2003 New YorkOxford University Press:323-73. [Google Scholar]
[3]. Rehman A, Insulinoma - a deceptive endocrine tumourJ Pak Med Assoc 2011 61(9):911-14. [Google Scholar]
[4]. Brentjens R, Saltz L, Islet cell tumors of the pancreasSurg Clin Nort America 2001 82(3):527-42. [Google Scholar]
[5]. Aisha S, Lubna MZ, Haque N, Recurrent insulinoma - rare among the raritiesJ Coll Phys Surg Pak 2007 17:364-66. [Google Scholar]
[6]. Czupryniak L, Strzelczyk J, Drzewoski J, Diagnostic difficulties in long-standing insulinoma with near-normal plasma insulin levelsJ Endocrinol Invest 2005 28:170-74. [Google Scholar]
[7]. Virally ML, Guillausseau PJ, Hypoglycemia in adultsDiabetes and Metab 1999 25(6):477-90. [Google Scholar]
[8]. Mesut Ozkaya, Mehmet Fatih Yuzbasioglu, Irfan Koruk, Erman Cakal4, Mustafa Sahin, Basak Cakal, Preoperative detection of insulinomas: two case reportsCases Journal 2008 1:362doi:10.1186/1757-1626-1-362 [Google Scholar]
[9]. Nikafarjam M, Warshaw A, Axelrod L, Deshpande V, Thayer S, Ferrone C, Improved Contemporary Surgical Management of Insulinoma: A 25-year experience at the Massachusettes General HospitalAnn Surg 2008 247:165-72. [Google Scholar]
[10]. Lam K, Lo C, Wat M, Malignant insulinoma with hepatoid differentiation: a unique case with alpha-fetoprotein productionEndocr Pathol 2001 12(3):351-54. [Google Scholar]