Methicillin Resistant Staphylococcus Epidermidis Induced Endogenous Endophthalmitis
Undrakonda Vivekanand1, Pradeep Pakalapati2, Gudimetla Sandeep Reddy3, Sritej Talluri4
1 Associate Professor, Department of Ophthalmology, Alluri Sitarama Raju Academy of Medical Sceinces, Malkapuram, Eluru, West Godavari, Andhra Pradesh, India.
2 Professor, Department of Ophthalmology, Alluri Sitarama Raju Academy of Medical Sceinces, Malkapuram, Eluru, West Godavari, Andhra Pradesh, India.
3 Consultant, Department of Ophthalmology, Srikiran Eye Institute, Achampet Junction, Pinamarthi Road, East Godavari, Andhra Pradesh, India.
4 Junior Resident, Department of Ophthalmology, Alluri Sitarama Raju Academy of Medical Sceinces, Malkapuram, Eluru, West Godavari, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Undrakonda Vivekanand, Flat no. 104, Satyachandra Residency, Guttastreet, Satrampadu, Eluru, West Godavari-534007, Andhra Pradesh, India. Phone : +918333044920, E-mail : vivekanandu@gmail.com
Fulminant endogenous endophthalmits, a relatively rare intraocular infection, caused by haematogenous spread of bacteria or fungi is usually seen in immune-deficient patients. We report a case of methicillin resistant Staphylococcus epidermidis causing endogenous endophthalmitis following platelet transfusion and intravenous antibiotic therapy for a suspected dengue fever.
Endogenous endophthalmitis, Pars plana vitrectomy, Retinal necrosis, Uveitis
Case Report
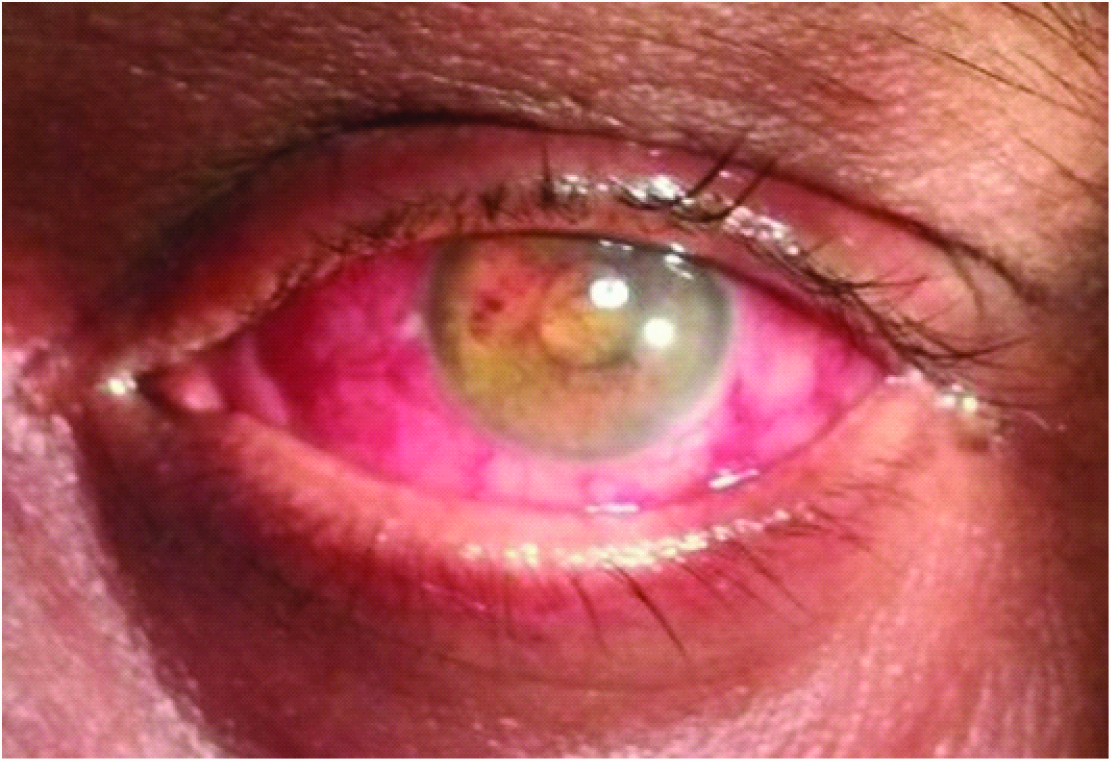
A 45-year-old man presented to ophthalmology outpatient department of Alluri Sitarama Raju academy of Medical sciences in the month September 2013, with 10 days history of painful swelling in left eye. Patient gave a history of undergoing treatment for suspected dengue fever for which he was treated with intravenous Ciprofloxacin (200mg 12th hourly) and platelet transfusion for five days following which he developed painful swelling in left eye. There was no history of trauma or operative procedures on left eye. Ocular examination revealed visual acuity of perception of light with conjunctival chemosis, hazy cornea, blood clots and exudative membrane present in anterior chamber in left eye [Table/Fig-1]. Examination of the right eye was normal with a visual acuity of 6/9. Ocular ultrasonography of left eye suggested extensive vitreous echoes with attached retina [Table/Fig-2]. A vitreous tap and aqueous tap was done under strict aseptic conditions. Intravitreal injection of vancomycin (1 mg/0.1 mL) and ceftazidime (2.25 mg/0.1 mL) was performed. Topical treatment, in addition included dexamethasone (0.1%) eye drops, timolol eye drops (0.5%),and atropine 1% eye ointment along with intravenous broad spectrum antibiotics ampicillin 500mg q4th hourly, gentamicin 80mg q12 hourly and metronidazole 500mg q 8th hourly were administered till the culture reports were awaited.
LE Endogenous endophthalmitis
B scan (LE) showing vitreous echoes

Gram staining of the vitreous sample revealed the presence of gram-positive Staphylococci. Culture and sensitivity of vitreous and aqueous sample revealed methicillin resistant coagulase-negative Staphylococcus epidermidis, sensitive to cefaparazone, cefotaxime, ceftriaxone, azithromycin and vancomycin done by Kirby-bauer antibiotic sensitivity testing [Table/Fig-3].
Antibiogram of Staphylococcus epidermidis isolates
| Drugs | |
|---|
| Amoxicillin-clavulanic acid | S |
| Ampicillin/amoxicillin | S |
| Cefotaxime/ceftriaxone | S |
| Cefaperazone | S |
| Vancomycin | S |
| Oxacillin | R |
| Reserved drugs | |
| Aztreonam | R |
| Cefoperazone-sulbactum | S |
| Cefpirome/cefepime | R |
| Piperacillin-tazobactum | S |
| S- Sensitive, R - resistant |
Other investigations such as total and differential count, peripheral smear, renal function tests,and blood sugars were normal. HIV was non-reactive. Blood culture was sterile. IgG antiboidies against dengue was negative.
One day after the vitreous tap his left visual acuity remained perception of light with dense vitritis. A pars planavitrectomy (PPV) was performed to further decrease microbialload and intravitreal antibiotic was repeated. There were extensive vitreous bands, pus extending in to the zonules, and large areas of retinal necrosis present. A subsequent lensectomy was done in the same sitting to thick fibrous band adhered to the posterior surface of the lens. Lensectomy was performed to avoid chance of developing complicated cataract later. Silicone oil was not injected as there was no retinal detachment or intraoperative break formation during the surgical procedure. Postoperative visual acuity was perception of light with intraocular pressure of 5mmHg. On subsequent followups the eye gradually progressed to phthisis bulbi.
Discussion
Endogenous endophthalmitis (EE) is a relatively rare intraocular infection which account for 2% to 8% of all cases of endophthalmitis. It usually affects immune deficient people, patients on prolonged intravenous drug use and patients on immunosuppressive treatment. Positive culture is the gold standard for identification of causative organism [1–5].
Bacteria and fungi are the most common pathogens, the former typically Staphylococcus sp., Streptococcus sp. and Klebsiella pneumonia. the latter generally Candida sp. or Aspergillus sp. Gram-negative organisms cause 32–37% of all EE cases and typically have poor visual outcomes because these infections are difficult to treat.
Staphylococcus epidermidis, is a gram-positive, skin-colonising cocci, is predominant species of the coagulase negative staphylococcus (CoNS) which does not usually produce aggressive virulence determinants, and usually requires an obvious breach in the host’s defence mechanism to cause severe infection, accounts for an average of 40% postoperative and posttraumatic endophthalmitis cases [6,7]. Methicillin-resistant coagulase negative Staphylococcus (MRCoNS) is one of the species described among the preoperative ones seen at a Japanese eyeclinic [8].
EE is an ongoing diagnostic and therapeutic dilemma for ophthalmologists as it is relatively rare, often presents like uveitis, and requires a high index of suspicion for prompt diagnosis and treatment. The treatment of EE is still controversial due to a lack of clinical trials. Potential treatments include systemic antibiotics, peri-ocular injections, intravitreal injection of antibiotics and possibly corticosteroids, pars planavitrectomy (PPV), or a combination of some of these. A major review of Endogenous Bacterial Endophthalmitis found in patients who had a PPV would benefit significantly in terms of higher likelihood for counting fingers vision or better, and a smaller likelihood of needing evisceration or enucleation. The outcome of EE mainly depends on three factors. First being virulence of the organism, second being the compromised host status and the last being delay in diagnosis. Vision is preserved in only about 40% of cases [9,10]. The greatest prognostic factors in EBE seem to be the infecting bacteria and the timing of initiating treatment.
This case is unusual in that a patient who was systemically well, had an episode of fever with low platelet count, was suspected to have dengue, following which platelet transfusion was done, after which he went on to develop an acute fulminant EE which rapidly progressed causing extensive retinal and other intraocular damage. A similar case report was reported by Whist E et al., where in a systemically normal with no locus of infection went on develop Staphylococcus epidermidis EE [11]. Unfortunately, as this case shows, EBE can occasionally mimic severe panuveitis, in which case salvaging vision or eye could be extremely difficult. The patient described in this case report received the first dose of intravitreal treatment and pars planavitrectomy 10 days after initial symptoms appeared. High clinical suspicion, early diagnosis and prompt aggressive treatment are imperative to minimise visual loss and the risk of losing the eye.
Conclusion
It is recommended that ophthalmic screening should be done routinely in high risk situations such as intravenous drug use, long term antibiotics, immunosuppressive therapy, primary or secondary immunodeficiency, prolonged central line use, debilitated patients and premature infants.
[1]. Jackson TL, Eykyn SJ, Graham EM, Stanford MR, Endogenous bacterial endophthalmitis: A 17-year prospective series and review of 267 reported casesSurv Ophthalmol 2003 48:403-23.[PubMed: 12850229]. Comprehensive review of endogenous bacterial endophthalmitis [Google Scholar]
[2]. Okada AA, Johnson RP, Liles WC, D’Amico DJ, Baker AS, Endogenous bacterial endophthalmitis, report of a 10-year retrospective studyOphthalmology 1994 101:832-38.[PubMed: 8190467] [Google Scholar]
[3]. Romero CF, Rai MK, Lowder CY, Adal KA, Endogenous endophthalmitis: case report and brief reviewAm Fam Phys 1999 60:510-14. [Google Scholar]
[4]. Bohigian GM, Olk RJ, Factors associated with a poor visual result in endophthalmitisAm J Ophthalmol 1986 101:332-34.[PubMed: 3485382] [Google Scholar]
[5]. Schiedler V, Scott I, Flynn HW, Janet DL, Benz MS, Miller D, Culture-proven endogenous endophthalmitis clinical features and visual outcomesAm J Ophthalmol 2004 137:725-31.[PubMed: 15059712] [Google Scholar]
[6]. Davis JL, Koidou-Tsiligianni A, Pflugfelder SC, Miller D, Flynn HW, Forster RK, Coagulase-negative staphylococcal endophthalmitis. Increase in antimicrobial resistanceOphthalmology 1988 95(10):1404-10. [Google Scholar]
[7]. Wong TY, Chee SP, The epidemiology of acute endophthalmitis after cataract surgery in Asian populationOphthalmology 2004 111(4):699-705. [Google Scholar]
[8]. Kato T, Hayasaka S, Methicillin-resistant Staphyloccocus aureus and methicillin-resistant coagulase-negative staphylococci from conjunctivas of preoperative patientsJpn JOphthalmol 1998 42(6):461-65. [Google Scholar]
[9]. Romero CF, Rai MK, Lowder CY, Adal KA, Endogenous endophthalmitis: case report and brief reviewAm Fam Phys 1999 60:510-14. [Google Scholar]
[10]. Shankar K, Gyanendra L, Hari S, Dev Narayan S, Culture proven endogenous endophthalmitis in apparently healthy individualsOcular Immun Inflam 2009 17:396-99. [Google Scholar]
[11]. Whist E, Hollenbach E, Dunlop A, Severe Acute Endogenous Endophthalmitis with Staphylococcus Epidermidis in a Systemically Well PatientOphthalmol Eye Dis 2011 3:25-28. [Google Scholar]