Background: Feeling of pain is one of the most important emotional determinants which dominate the perception of females who undergo the process of labour and delivery. Patient controlled epidural labour analgesia (PCEA) is convenient and safer technique for this purpose. Very few studies compared clonidine and fentanyl with ropivacaine in labour analgesia in past. This study was undertaken to compare fentanyl and clonidine in PCEA.
Aims: To compare low concentration ropivacaine with or without fentanyl or clonidine for labour analgesia and its effect on maternal and foetal safety.
Settings and Design: Prospective, double blind, randomized, comparative study.
Materials and Methods: Ninety primegravida in labour were divided into three groups (n=30) and patient controlled epidural labour analgesia was given to them: Initial bolus of 10ml of ropivacaine 0.125% in Group I; with fentanyl 2 μg/ml in Group II and with clonidine 1μg/kg in Group III. Subsequently each group received ropivacaine 0.125% through patient controlled epidural analgesia (PCEA) as background infusion of 5 ml/hr with lockout interval time of 10min and subsequent bolus of 5ml. Hemodynamic parameters, sensory level, motor block and pain relief were noted. Total analgesic dose of local anaesthetic and feto-maternal adverse effects were also recorded.
Results: At baseline, groups were matched demographically, hemodynamically as well as for intensity of pain. There was a statistically significant decrease in hemodynamic parameters from baseline in all groups with maximum reduction in group III. A significant difference among groups in VAS was observed at zero min and from 120min till 240min intervals and lowest values were in Group III. No significant difference was observed among the groups for mode of delivery and expulsive efforts. Total analgesic dose and PCA bolus requirement was maximum in Group I and minimum in Group III and the difference was statistically significant among groups. Six (20%) patients had shivering in Group II and hypotension was recorded in only 1 (3.3%) patient of Group III.
Conclusion: Ropivacaine 0.125% was effective in decreasing labour pain without any motor blockade. Clonidine 1μg/kg was superior to fentanyl 2μg/ml as an adjuvant in PCEA for labour without any significant feto-maternal adverse effects.
Introduction
Epidural analgesia is widely regarded as a boon for pregnant patients as it provide relief from labour pain for a longer duration and uneventful smooth delivery. Though a slightly larger dose of ropivacaine is required to achieve analgesia, addition of opioids and clonidine to ropivacaine provides opportunity to use more diluted solutions for better analgesia, and reduces the risk of systemic toxicity and incidence of motor block [1-3].
Clonidine has been used as an adjuvant to epidural local anaesthetics to improve the quality of analgesia after major abdominal surgeries [4-6]. At low doses, epidural clonidine improves the quality of anaesthesia, reduces the dose requirement of the anaesthetic agents and provides better hemodynamic stability during anaesthesia [7]. Keeping all these pharmacological interactions in consideration, we compared fentanyl and clonidine as an adjuvant to ropivacaine in patient controlled epidural analgesia (PCEA) in parturient.
Materials and Methods
After getting approval from the institutional ethical committee, this study was conducted on healthy term primegravida parturient admitted to Department of Obstetrics and Gynaecology. This was a prospective, double blind, randomized, comparative study. Informed written consent was taken from every patient and her attendants. Anaesthesia SectionInclusion criteria were: healthy term primegravida parturient aged 18 – 35 yrs of ASA grade 1 and 2 in active stage of labour with singleton foetus in vertex presentation without systemic analgesic administration. Exclusion criteria were: patient refusal, pre-eclamptic toxaemia or eclampsia and pregnancy induced hypertension, systemic hypertension, diabetes mellitus, heart disease, previous LSCS or absolute indication for LSCS, allergy to study drugs, patient inability to use PCEA pump or patient not willing to use PCEA pump, failed blocks, technically difficult block or accidental dural punctures.
Each patient received an intravenous infusion of 500 ml of Ringer’s lactate over 10-15 min before induction of epidural analgesia. At 3-4 cm of cervical dilatation epidural block was performed. Patient was placed in sitting position. With proper aseptic and antiseptic precautions, under local anaesthesia a multi-hole epidural catheter was inserted at L3-4 intervertebral space with 18G Touhy needle using loss of resistance technique to air. Catheter was placed 3-4 cm in epidural space in cephalic direction. A test dose of 3ml 2% lignocaine with 1:200000 epinephrine was administered to exclude intravenous or subarachnoid catheter placement.
Patients were divided in 3 groups using a computer generated random number table into one of the following groups:
Group I received: initial bolus of 10ml of ropivacaine 0.125% alone;
Group II received: initial bolus of 10ml of ropivacaine 0.125% with fentanyl 2 μg/ml of solution;
Group III received: initial bolus of 10ml ropivacaine 0.125% with clonidine 1 μg/kg body weight.
Subsequently each patient group received ropivacaine 0.125% alone through PCEA as background infusion of 5 ml/hr with lockout interval of 10min and patient demand bolus of 5ml. Maximum drug allowed in 4h was 80ml. Each study solution was freshly prepared using normal saline as diluents to achieve the desired concentration at room temperature. After catheter placement, patients were placed in the supine position with left uterine displacement and 30o elevation of the head end of the bed.
After giving drugs, hemodynamic parameters, sensory level, motor block and pain relief were noted. Level of analgesia was checked by pin prick with 23G needle in mid-clavicular line, every 5min till maximum level was achieved. The severity of pain was assessed before the block and at 15, 30, 45, and 60 min and then at 30min interval. Pain was evaluated using 10cm visual analogue scale (where 0 represents no pain and 10cm represents worst pain ever experienced). Postpartum parturient were asked to rate their overall analgesia for labour and delivery from 0 - 2 (where 0 = worse than expected, 1 = about as expected, 2 = better than expected). Motor block was assessed bilaterally after attainment of maximum sensory block and then at hourly interval using Bromage scale. Analgesia was considered adequate if pain score was ≤4. Onset of analgesia was defined as from time of first bolus dose to time of achieving VAS <4. If pain relief was inadequate at the peak of uterine contraction 15min after the second dose of ropivacaine; it was classified as ropivacaine failure, and patient was withdrawn from the study.
Maternal blood pressure and pulse rate were monitored at 15, 30, 45, 60 min and subsequently every 30min. Foetal heart rate was also monitored every 15min. The presence and severity of maternal complications including hypotension (defined as SBP <100 mmHg or decrease of more than 20% of baseline), nausea and vomiting, pruritis, drowsiness and respiratory depression were also recorded. At delivery quality of natural expulsive efforts (poor, fair, moderate or good) was evaluated by the obstetrician. Mode of delivery was recorded and neonates were evaluated by means of Apgar score at 1, 5 and 10 minutes. Total analgesic dose of local anaesthetic required in each group and any other side effects on the mother and neonate was also recorded.
Demographic profile of patients in different groups
| S No | Variable | Group I (n=30) | Group II (n=30) | Group III (n=30) | Significance of difference |
| Mean | SD | Mean | SD | Mean | SD | “F“ | “p“ |
| 1. | Age (in years) | 23.93 | 1.87 | 24.10 | 2.34 | 25.13 | 2.39 | 2.589 | 0.081 |
| 2. | BMI (kg/m2) | 24.72 | 1.09 | 24.86 | 2.53 | 23.89 | 0.89 | 2.990 | 0.056 |
| | | No. | % | No. | % | No. | % | x2 | P |
| 3. | Cervical dilatation rate (cm/hr) |
| | 3 | 4 | 13.3 | 6 | 20.0 | 3 | 10.0 | 4.612 | 0.329 |
| | 4 | 26 | 86.7 | 21 | 70.0 | 24 | 80.0 |
| | 5 | 0 | 0 | 3 | 10.0 | 3 | 10.0 |
Comparison of heart rate among groups at different time intervals
| Time interval | Group I (n=30) | Group II (n=30) | Group III (n=30) | Significance of difference |
| n | Mean | SD | n | Mean | SD | n | Mean | SD | “F“ | “p“ |
| Pre | 30 | 83.03 | 8.84 | 30 | 79.87 | 8.32 | 30 | 79.63 | 9.24 | 1.394 | 0.253 |
| 0 min | 30 | 87.10 | 9.36 | 30 | 81.13 | 7.64 | 30 | 77.13 | 9.45 | 9.625 | <0.001 |
| 15 min | 30 | 89.10 | 10.28 | 30 | 86.13 | 6.28 | 30 | 69.17 | 9.36 | 54.737 | <0.001 |
| 30 min | 30 | 90.73 | 7.67 | 30 | 90.23 | 7.71 | 30 | 67.40 | 9.52 | 76.493 | <0.001 |
| 45 min | 30 | 89.57 | 5.95 | 30 | 87.03 | 6.50 | 30 | 64.93 | 8.50 | 110.208 | <0.001 |
| 60 min | 30 | 89.30 | 9.85 | 30 | 88.00 | 5.68 | 30 | 64.33 | 4.54 | 118.596 | <0.001 |
| 90 min | 30 | 87.27 | 7.02 | 30 | 85.03 | 5.35 | 30 | 64.70 | 3.27 | 156.952 | <0.001 |
| 120 min | 30 | 86.50 | 6.79 | 30 | 86.53 | 4.60 | 30 | 65.93 | 4.39 | 146.803 | <0.001 |
| 150 min | 30 | 84.57 | 4.65 | 30 | 85.23 | 6.47 | 30 | 70.70 | 5.64 | 63.596 | <0.001 |
| 180 min | 28 | 82.57 | 11.43 | 30 | 85.43 | 5.32 | 30 | 70.13 | 3.85 | 35.158 | <0.001 |
| 210 min | 25 | 79.28 | 6.22 | 30 | 85.27 | 6.81 | 23 | 69.22 | 2.13 | 53.254 | <0.001 |
| 240 min | 19 | 80.89 | 5.40 | 21 | 85.24 | 3.33 | 17 | 68.82 | 1.67 | 90.173 | <0.001 |
| 270 min | 16 | 76.25 | 7.33 | 12 | 84.00 | 2.92 | 12 | 69.83 | 2.92 | 22.521 | <0.001 |
| 300 min | 7 | 79.43 | 6.55 | 6 | 85.50 | 0.84 | 6 | 68.33 | 0.82 | 27.579 | <0.001 |
Comparison of SBP among groups at different time intervals
| Time interval | Group I (n=30) | Group II (n=30) | Group III(n=30) | Significance of difference |
| n | Mean | SD | n | Mean | SD | n | Mean | SD | “F“ | “p“ |
| Pre | 30 | 127.70 | 10.00 | 30 | 130.30 | 9.27 | 30 | 130.80 | 6.98 | 1.062 | 0.350 |
| 0 min | 30 | 123.20 | 9.97 | 30 | 126.53 | 8.35 | 30 | 125.80 | 7.87 | 1.195 | 0.308 |
| 15 min | 30 | 119.40 | 11.47 | 30 | 120.33 | 12.33 | 30 | 119.97 | 8.86 | 0.055 | 0.947 |
| 30 min | 30 | 118.37 | 8.85 | 30 | 121.50 | 6.60 | 30 | 117.33 | 7.95 | 2.289 | 0.107 |
| 45 min | 30 | 119.83 | 9.16 | 30 | 123.37 | 7.31 | 30 | 117.83 | 6.60 | 3.906 | 0.024 |
| 60 min | 30 | 119.30 | 9.25 | 30 | 123.00 | 5.39 | 30 | 118.07 | 7.57 | 3.450 | 0.036 |
| 90 min | 30 | 118.77 | 8.24 | 30 | 122.33 | 7.84 | 30 | 119.50 | 7.22 | 1.759 | 0.178 |
| 120 min | 30 | 120.83 | 7.32 | 30 | 121.40 | 7.35 | 30 | 121.40 | 6.28 | 0.066 | 0.937 |
| 150 min | 30 | 123.40 | 8.32 | 30 | 125.30 | 6.72 | 30 | 122.67 | 6.45 | 1.066 | 0.349 |
| 180 min | 28 | 117.25 | 9.20 | 30 | 123.97 | 5.71 | 30 | 120.03 | 6.49 | 6.326 | 0.003 |
| 210 min | 25 | 117.44 | 7.22 | 30 | 124.77 | 6.04 | 23 | 117.35 | 5.18 | 12.977 | <0.001 |
| 240 min | 19 | 80.89 | 5.40 | 21 | 85.24 | 3.33 | 17 | 68.82 | 1.67 | 90.173 | <0.001 |
| 270 min | 16 | 115.75 | 8.00 | 12 | 125.33 | 2.61 | 12 | 119.50 | 2.84 | 10.377 | <0.001 |
| 300 min | 7 | 108.29 | 2.63 | 6 | 128.00 | 1.79 | 6 | 120.67 | 5.32 | 52.319 | <0.001 |
Comparison of DBP among groups at different time intervals
| Time interval | Group I (n=30) | Group II (n=30) | Group III (n=30) | Significance of difference |
| n | Mean | SD | n | Mean | SD | n | Mean | SD | “F“ | “p“ |
| Pre | 30 | 80.10 | 8.87 | 30 | 82.30 | 4.96 | 30 | 79.97 | 6.24 | 1.087 | 0.342 |
| 0 min | 30 | 77.43 | 7.60 | 30 | 82.0 | 6.07 | 30 | 77.57 | 7.03 | 4.221 | 0.018 |
| 15 min | 30 | 72.90 | 8.48 | 30 | 76.37 | 5.25 | 30 | 71.63 | 6.54 | 3.801 | 0.026 |
| 30 min | 30 | 72.53 | 6.90 | 30 | 73.47 | 5.96 | 30 | 69.47 | 6.28 | 3.216 | 0.045 |
| 45 min | 30 | 70.67 | 7.30 | 30 | 75.67 | 4.51 | 30 | 69.47 | 4.03 | 10.835 | <0.001 |
| 60 min | 30 | 71.93 | 6.02 | 30 | 76.47 | 4.49 | 30 | 71.13 | 5.53 | 8.565 | <0.001 |
| 90 min | 30 | 71.80 | 9.18 | 30 | 77.07 | 6.41 | 30 | 70.90 | 4.21 | 6.979 | 0.002 |
| 120 min | 30 | 71.83 | 6.99 | 30 | 76.03 | 8.64 | 30 | 73.17 | 4.11 | 2.953 | 0.057 |
| 150 min | 30 | 77.27 | 8.00 | 30 | 81.50 | 6.42 | 30 | 74.38 | 7.25 | 7.340 | 0.001 |
| 180 min | 28 | 73.75 | 7.28 | 30 | 78.53 | 6.49 | 30 | 74.80 | 5.43 | 4.453 | 0.014 |
| 210 min | 25 | 71.64 | 6.53 | 30 | 78.23 | 7.21 | 23 | 71.17 | 5.22 | 10.301 | <0.001 |
| 240 min | 19 | 73.68 | 6.09 | 21 | 83.57 | 6.38 | 20 | 72.70 | 5.38 | 20.813 | <0.001 |
| 270 min | 16 | 77.00 | 5.85 | 12 | 81.75 | 6.24 | 12 | 72.17 | 7.70 | 6.396 | 0.004 |
| 300 min | 7 | 71.86 | 3.53 | 6 | 83.67 | 2.34 | 6 | 68.83 | 2.04 | 48.472 | <0.001 |
Comparison of total analgesic dose and total PCA bolus
| Variable | Group I (n=30) (Mean ± SD ) | Group II (n=30) (Mean ± SD ) | Group III (n=30) (Mean ± SD ) |
| Total analgesic dose (ml) | 47.42 ± 9.70 | 41.25 ± 7.30 | 35.0 ± 4.82 |
| Total no. of PCA bolus | 3.40 ± 1.22 | 1.90 ± 1.06 | 1.03 ±1.03 |
Comparison of total analgesic dose and total PCA bolus
| S No | Variable | Group I vs Group II | Group I vs Group III | Group II vs Group III |
| "t" | "p" | "t" | "p" | "t" | "p" |
| 1 | Total analgesic dose | 2.891 | 0.007 | 6.275 | <0.001 | 3.911 | <0.001 |
| 2. | Total PCA bolus | 5.078 | <0.001 | 8.106 | <0.001 | 3.204 | 0.002 |
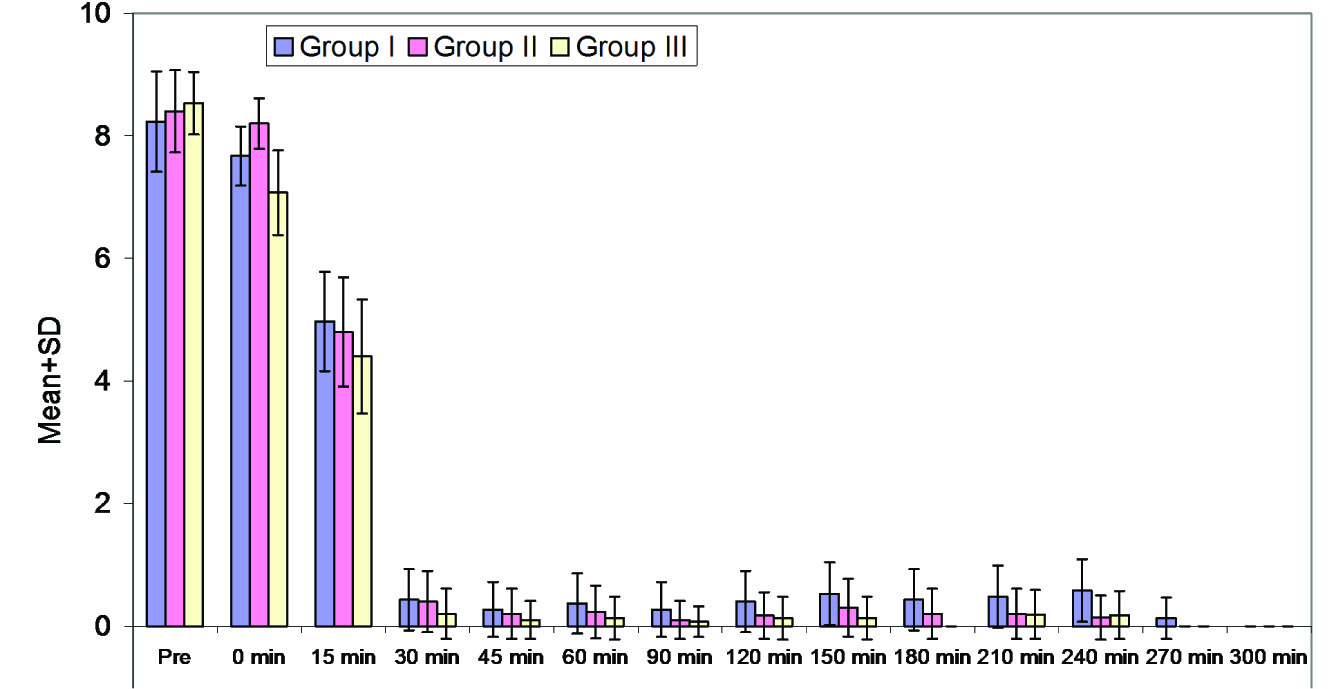
Comparison of VAS scores in three groups over time
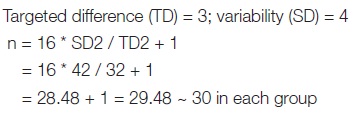
Statical Analysis
The results are presented in mean ± SD and percentages. The chi-square test was used to compare the categorical/dichotomous variables among the groups. The ANOVA with Tukey’s multiple comparison tests was used to compare the means of the variables among the three groups. The repeated measures of analysis of variance were used to test the differences at different time intervals and among the groups. The interaction between time and groups was also tested. The Tukey’s test was used for pair wise comparisons. The p-value<0.05 was considered as significant. All the analysis was carried out by using SPSS 16.0 version.
Sample size estimation
Results
The groups were matched for demographic variables as well as for cervical dilatation at the time of initiation of epidural analgesia. At baseline, all the hemodynamic parameters and VAS score were matched [Table/Fig-1] Sensory level up to T-10 was achieved in all patients.
At all the time intervals during the study period, heart rate was minimum in Group III while Group I had maximum values till 120min interval and thereafter, Group II had maximum values. Although the difference in heart rate was statistically significant among the groups but it was clinically non- significant [Table/Fig-2].
After epidural block, a reduction in SBP was observed in all the three groups with a constant descending trend in all the groups till 15min followed by a random trend in all the groups [Table/Fig-3]. No significant intergroup difference was observed till 30 min. At all time intervals the difference was statistically significant among groups except from 45 to 180 min. At all time intervals after baseline, DBP in Group II had higher value as compared to Groups I and III and the difference among groups was also found to be significant statistically throughout the study period except at baseline and 120min intervals [Table/Fig-4].
Total analgesic dose and PCA bolus requirement was maximum in Group I and minimum in Group III and the difference among groups was significant statistically. None of the patient in three groups was exclude from the study due to ropivacaine failure [Table/Fig-5a,5b].
At baseline no significant difference among groups in VAS was observed, however, a significant difference among groups was observed at 120min till 240min intervals. At all these time intervals, 11Group III had lower mean values as compared to Groups I and II [Table/Fig-6]. Difference in onset of analgesia was statically insignificant in three groups (11.0±3.4 min in I, 10.30±2.03 min in II and 9.89±3.50 min in III).
In all the three groups, motor blockade was assessed at 1h, 2h, 3h and 4h intervals and was recorded as 0. Majority of patients in three groups applied good expulsive effort
(90% in I and III and 80% in II) and did not show a statistically significant intergroup difference.
On comparing adverse effects, shivering being significantly higher in Group II (20%) as compared to that in Groups I and III (0%). Hypotension was recorded in only 1 (3.3%) patient of Group III. No other complication was observed in any group.
No significant difference was observed among the groups for mode of delivery. Majority of women in all the three groups had a normal vaginal delivery (80% in I and II while 73.3% in III). None of the babies born had Apgar score <7 at 1, 5 and 10 min intervals in any of the three groups. Majority of women in all the three groups were satisfied (80% in I and II while 83.3% in III).
Discussion
Safe foetal outcome without any adverse maternal effect is the chief goal of pain relief during labour and lumbar epidural analgesia is the most efficient and widely employed modality for this. Of all the available methods of labour analgesia, epidural analgesia satisfies the basic requirements of labour analgesia by fulfilling the objective of decreasing the pain of labour without affecting other sensations such as a desire to push and to allow normal walking while preserving the tone of pelvic floor muscles as well as retaining the sensation of the baby’s head in the vagina; thus, allowing labour to proceed unhindered.
Epidural bupivacaine had been used extensively in the past for providing, pain relief in patients undergoing labour and delivery. However, in recent years, ropivacaine and levobupivacaine has increasingly replaced bupivacaine for the said purpose because of its similar analgesic properties and decreased propensity of cardio toxicity [8]. The concentration of ropivacaine used in our study was 0.125% because higher concentration may lead to more adverse effects. The concentration used in our study has been shown to be effective in treating labour pain in many studies[9,10].
Lim et al., reported another adaptation of the epidural delivery pump technology. This computer-integrated PCEA (CI-PCEA) controls background infusion rates depending on the previous hour’s demand boluses. This randomized trial compared a standard PCEA technique of 0.1% ropivacaine with fentanyl administered as bolus-only by patient demand to the CI-PCEA technique that initiated an infusion algorithm with changing infusion rates depending on the demand boluses. Despite patients with the CI-PCEA technique receiving background infusions, the hourly consumption of ropivacaine was no different from that of the standard group thus illustrating that there is room for improvement in administering epidural medication, especially for women with prolonged labour. It allows patient to match dose of analgesia to amount of pain as labour progresses and patient variability in local anaesthetic requirement, instils a degree of control to the woman and may improve maternal satisfaction. There is reduction in the need for clinician top-ups, in the amount of local anaesthetic and opioid delivered and incidence of motor block [11,12].
Opioid are the most widely used class of adjuvant to epidural local anaesthetic in labour analgesia practice. Fentanyl and remifentanyl are the two most commonly used opioid for this purpose. The dose of fentanyl used in our study was 2 mcg/ml of drug solution, in loading bolus. This dose was consistent with the dose used in previous study which concluded that this concentration of the fentanyl intensifies the analgesic action of ropivacaine but in their study, they used fentanyl in every top up which led to cumulative higher dose of fentanyl [13]. Therefore, in our study we avoided use of fentanyl in top up boluses to reduce the cumulative dose of fentanyl.
Clonidine being a α-2 agonist, is known to increase the effectiveness of local anaesthetic agent in epidural labour analgesia in many studies [11,14-16]. The dose of clonidine used in our study was 1mcg/kg in loading bolus, which approximates to 50-70 mcg clonidine in loading bolus. Previous studies have shown that clonidine used in doses greater than 100 mcg have been associated with maternal and foetal bradycardia, maternal hypotension and adverse foetal outcome while doses less than 30mcg are ineffective in increasing the potency of local anaesthetics [17], but 75 mcg clonidine is effective in labour analgesia when given with local anaesthetics [11], So we used the clonidine in 1 mcg/kg dose as patients in our study were of lesser height and weight as compared to the patients enrolled in above study, thus avoiding overdosing of clonidine in the patients.
PCEA for labour analgesia is safe in experienced hands. It has the advantage of giving local anaesthetic medication via continuous infusion. When compared with continuous epidural infusion, PCEA has been shown to reduce local anaesthetic requirement [18-20].
We found that the heart rate was lowest in group III followed by group II and highest in group I. The lower heart rate decreases the myocardial oxygen demand of the parturient and none of the patients in our study required any type of intervention for decreased heart rate. In spite of the fact that clonidine crosses placenta and can lead to foetal bradycardia as seen in the previous studies using higher doses of clonidine, the dose in our study did not caused bradycardia to the foetus and the incidence of caesarean deliveries were same and comparable in all the three groups [17].
We preloaded the patients to avoid any hypotension due to sympathectomy and it seems that the preloading is adequate to prevent any episode of hypotension associated with initiation analgesia. No patient in any of the group required any vasopressor for treatment of hypotension; therefore we can say that there is no risk of hypotension with the use of epidural analgesia with the drug combinations used in our study.
The VAS score of the three groups were comparable at baseline and throughout the labour and no significant difference was found between the three groups except at 180min. Although, at 180min the difference in VAS was statistically significant, however, it was clinically insignificant as at 180min the mean VAS in all the three groups was less than 0.5 which was clinically acceptable grade of analgesia. Thus, we can say that all the three drug solution used in our study were able to achieve adequate and acceptable analgesia in labouring females.
In our study the effect of epidural analgesia in all the three groups over maternal expulsive efforts showed that no patient in our study had weak expulsive efforts that may lead to increase incidence of assisted /caesarean deliveries. 90% patient had good expulsive efforts in group I and Group III while 10% patient in both the groups has moderate expulsive efforts. In Group II 80% patient had good expulsive effort and 20% had moderate expulsive efforts. The difference between the three groups was statistically and clinically insignificant. The rate of forceps, caesarean and spontaneous vaginal dliveries in all the three groups were comparable and there was no statistically significant difference among them. The rate of assisted delivery in group I, II and III was 10% and the rate of LSCS in group I, II, III was 10%, 10% and 16.7% respectively. The incidence of assisted and caesarean deliveries in patient receiving epidural labour analgesia was 10-30 % in previous studies which was much higher than found in our study [21]. Previous studies found that the rate of spontaneous delivery was similar in both fentanyl and clonidine group which is also seen in our study [10,22]. The incidence of maternal complication was 20% in group II while 0% in group I and 3.3% in group III. The only reported complication in group II was shivering that was easily controlled with injection tramadol 0.5mg/kg IV. Only 1 patient in group III suffered hypotension which was treated with 200ml fluid bolus. No other adverse effect was seen in our study.The incidence of hypotension and bradycardia was much lower in our study than previous studies which used higher concentration of drugs [17,22]. The total amount of ropivacaine 0.125% in the three groups were 47.2ml, 41.25ml, and 35ml respectively and the number of PCA bolus required in the three groups were 3.4, 1.9, 1.03 respectively. There was a statistically significant reduction in the requirement of ropivacaine due to addition of fentanyl and clonidine as adjuvant and clonidine is more effective in this respect as it causes 26.19% reduction in requirement of ropivacaine. While fentanyl causes only 13% reduction in requirement of ropivacaine. Previous observation that 75 mcg clonidine had a dose sparing effect on ropivacaine is supported by our study [11,23].
Conclusion
The maternal satisfaction in all the three groups was comparable and most of the patients were extremely satisfied. None of the patient in our study showed dissatisfaction with our regimen. Therefore we can say that all the three drug combination were effective in controlling labour pain. 0.125% concentration of ropivacaine was sufficient for labour analgesia and it does not cause any motor weakness which can affect the ambulation of the patient or the maternal expulsive efforts. The addition of fentanyl and clonidine as an adjuvant can decrease the requirement of ropivacaine and helps in reduction of local anaesthetic toxicity. Clonidine and fentanyl does not cause any adverse foetal or maternal outcome.
Our study was done on primegravida of grade ASA I &II having no obstetric complication, therefore the results of this study cannot be applied on patient of ASA grade III, IV or patients having any obstetrical complications like pre eclamptic toxaemia, multiple pregnancies, etc.
We have not used fentanyl in doses according to weight as obese or malnourished patients were excluded from our study, therefore careful titration of drug dose is required in these patients. Thus in our study we found that both fentanyl and clonidine have dose sparing effect on 0.125% ropivacaine with stable hemodynamic and no significant feto-maternal adverse effects. Clonidine is better than fentanyl in the dose sparing effect.
[1]. R Landau, E Schiffer, M Morales, G Savoldelli, C Kern, The dose-sparing effect of clonidine added to ropivacaine for labour epidural analgesia.Anesth Analg. 2002 95(3):728-34. [Google Scholar]
[2]. AC Santos, GR Arthur, H Pedersen, HO Morishima, M Finster, BG Covino, Systemic toxicity of ropivacaine during ovine pregnancy. Anesth. 1991 75:137-41. [Google Scholar]
[3]. G Turner, DA Scott, A comparison of epidural ropivacaine infusion alone and with three different concentration of fentanyl for 72 hours of postoperative analgesia following major abdominal surgery.Reg Anesth. 1998 23:A39 [Google Scholar]
[4]. J Motsch, E Graber, K Ludwig, Addition of clonidine enhances postoperative analgesia from epidural morphine: A double-blind study.Anesth. 1990 73:1067-73. [Google Scholar]
[5]. H Finegold, G Mandell, Comparison of ropivacaine 0.1%-fentanyl and bupivacaine 0.125%-fentanyl infusions for epidural labour analgesia.Can J Anesth. 2000 47(8):740-45. [Google Scholar]
[6]. JG Forster, PH Rosenberg, R Kalra, Small dose of clonidine mixed with low-dose ropivacaine and fentanyl for epidural analgesia after total knee arthroplasty.Br J Anaesth. 2004 93:670-77. [Google Scholar]
[7]. I Acalovschi, C Bodolea, C Manoiu, Spinal anesthesia with meperidine, effects of added-adrenergic agonists: Epinephrine versus clonidine.Anesth Analg. 1997 84:1333-39. [Google Scholar]
[8]. JA Katz, PO Bridenbaugh, DC Knarr, SH Helton, DD Denson, Pharmacodynamics and pharmacokinetics of epidural ropivacaine in humans.Anesth Analg. 1990 70:16-21. [Google Scholar]
[9]. T Girard, C Kern, I Hösli, A Heck, MC Schneider, Ropivacaine versus Bupivacaine 0.125% with Fentanyl 1 μg/ml for Epidural Labour Analgesia.Acta Anaesth Belg. 2006 57:45-9. [Google Scholar]
[10]. T Ismet, Tuna E, Melek T, Oznur T, Rusen K, Melek I, The Comparison of Efficiency of Ropivacaine and Addition of Fentanyl or Clonidine in Patient Controlled Epidural Analgesia for Labour.The Int J Anesth. 2006 11(2) [Google Scholar]
[11]. Y Lim, AT Sia, D Woo, Comparison of computer integrated patient controlled analgesia and patient controlled epidural analgesia with a basal infusion for labour and delivery.Anaesth Intensive Care. 2009 37:46-53. [Google Scholar]
[12]. ST Pandya, Labour analgesia: Recent advances.Anesth. 2010 54(5):400-08. [Google Scholar]
[13]. YK Chhetty, U Naithani, S Gupta, V Bedi, I Agrawal, L Swain, Epidural labour analgesia: A comparison of ropivacaine 0.125% versus 0.2% with fentanyl.JObs Anaesth and Critical Care. 2013 1(1):16-22. [Google Scholar]
[14]. B Claes, M Soetens, AV Zundert, S Datta, Clonidine added to bupivacaineepinephrine-sufentanil improves epidural analgesia during childbirth.Reg Anesth Pain Med. 1998 23(6):540-47. [Google Scholar]
[15]. RK Parker, NR Connelly, T Lucas, S Serban, R Pristas, E Berman, Epidural clonidine added to a bupivacaine infusion increases analgesic duration in labour without adverse maternal or fetal effects.Jr Anesth. 2007 21(2):142-47. [Google Scholar]
[16]. C Aveline, SE Metaoua, A Masmoudi, PY Boelle, F Bonnet, The effect of clonidine on the minimum local analgesic concentration of epidural ropivacaine during labour.Anesth Analg. 2002 95(3):735-40. [Google Scholar]
[17]. F Roelants, The use of neuraxial adjuvant drugs (neostigmine, clonidine) in obstetrics.Curr Opin Anaesth. 2006 19(3):233-37. [Google Scholar]
[18]. AT Sia, JL Chong, Epidural 0.2% ropivacaine for labour analgesia: parturientcontrolled or continuous infusion.Anaesth Intensive Care. 1999 27:154-58. [Google Scholar]
[19]. VM Vyver, S Halpern, G Joseph, A Heck, MC Schneider, Patient-controlled epidural analgesia versus continuous infusion for labour analgesia. A meta-analysis.Br J Anaesth. 2002 89:459-65. [Google Scholar]
[20]. DR Gambling, CJ Huber, J Berkowitz, Patient-controlled epidural analgesia in labour: varying bolus dose and lockout interval.Can J Anaesth. 1993 40:211-17. [Google Scholar]
[21]. JP Smedvig, E Soreide, L Gjessing, G Savoldelli, C Kern, Ropivacaine 1 mg/ml, plus fentanyl 2 μg/ml for epidural analgesia during labour.Acta Anaesthesiol Scand. 2001 45(5):595-99. [Google Scholar]
[22]. S Celleno, G Capogna, P Costantino, A Zangrillo, M Finster, BG Covino, Comparison of fentanyl with clonidine as adjuvants for epidural analgesia with 0.125% bupivacaine in the first stage of labour.Int J Obstetr Anesth. 1995 4(1):26-9. [Google Scholar]
[23]. I Cigarini, A Kaba, F Bonnet, E Brohon, F Dutz, F Damas, Epidural clonidine combined with bupivacaine for analgesia in labour. Effects on mother and neonate.Reg Anesth. 1995 20(2):113-20. [Google Scholar]