Post- Thyroidectomy Haematoma Causing Severe Supraglottic Oedema and Pulmonary Oedema - A Case Report
Leena Harshad Parate1, Vinayak Seenappa Pujari2, Tejesh C Anandaswamy3, Saurabh Vig4
1 Assistant Professor, Department of Anaesthesia, M.S. Ramaiah Medical College, Bangalore, Karnataka, India.
2 Associate Professor, Department of Anaesthesia, M.S. Ramaiah Medical College, Bangalore, Karnataka, India.
3 Assosciate Professor, Department of Anaesthesia, M.S. Ramaiah Medical College, Bangalore, Karnataka, India.
4 Junior Resident, Department of Anaesthesia, M.S. Ramaiah Medical College, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Leena Harshad Parate, Assistant Professor, Department of Anaesthesia, M.S. Ramaiah Medical College, Bangalore. Karnataka, India. Phone : +9480525925, E-mail : dr_leenag@yahoo.co.in
Large, long standing goiters present multiple challenges to anaesthesiologist. Post thyroidectomy haematoma is a rare but life threatening complication of thyroid surgery leading to airway obstruction. We report a case of huge goiter that underwent near total thyroidectomy and developed post thyroidectomy haematoma. Within no time it resulted in near fatal airway obstruction, pulmonary oedema and cardiac arrest. The haematoma was evacuated immediately and patient was resuscitated successfully. Pulmonary oedema was further worsened by subsequent aggressive fluid resuscitation. She was electively ventilated with PEEP and was extubated after five days. Except for right vocal cord palsy her postoperative stay was uneventful. This is unique case where a post thyoidectomy haematoma has resulted in fatal supraglottic oedema and pulmonary oedema. Early recognition, immediate intubation and evacuation of haematoma are the key to manage this complication. We highlight on the pathophysiology of haematoma and discuss the strategies to prevent similar events in future.
Complications, Haemorrhage, Thyroidectomy
Case Report
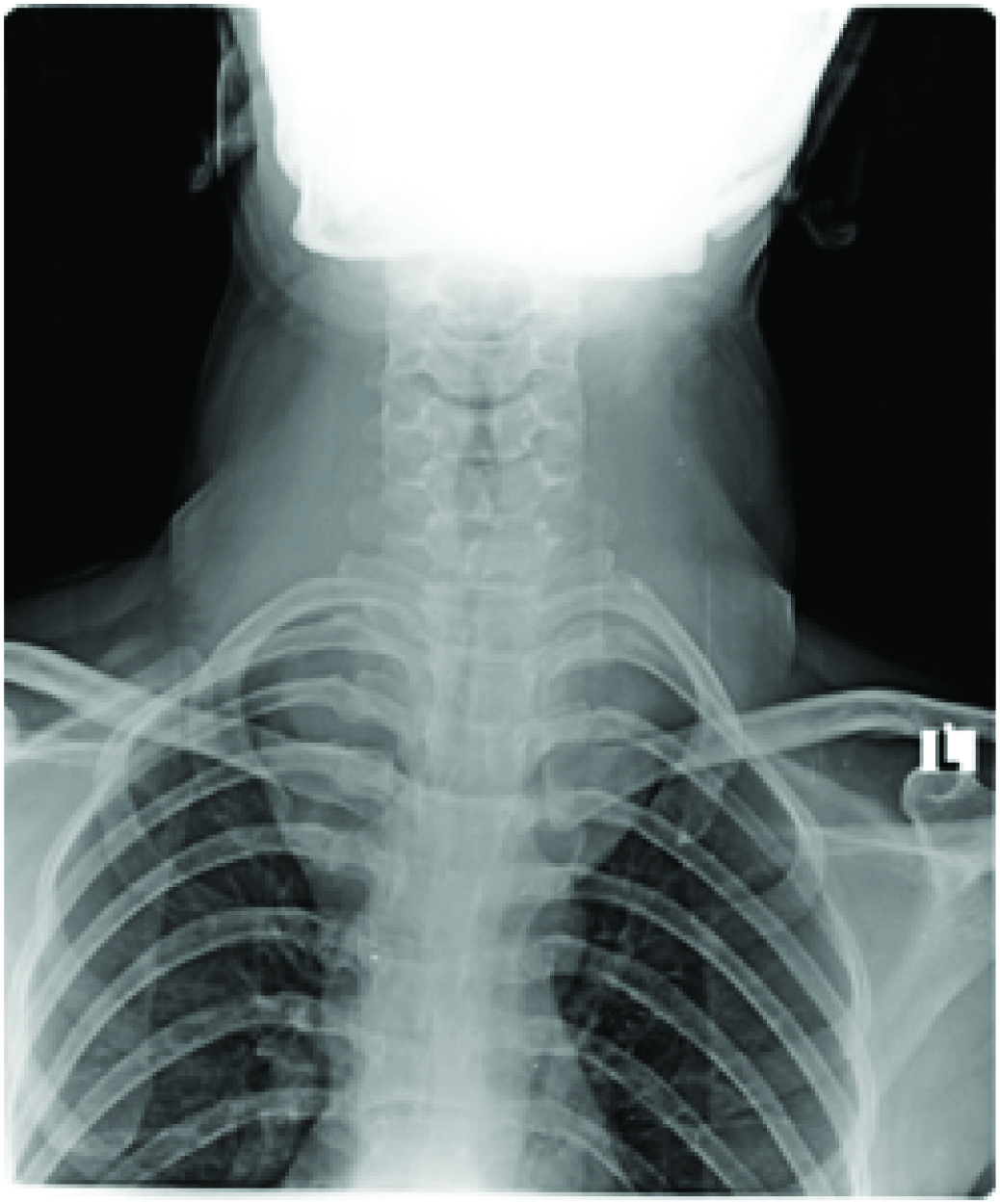
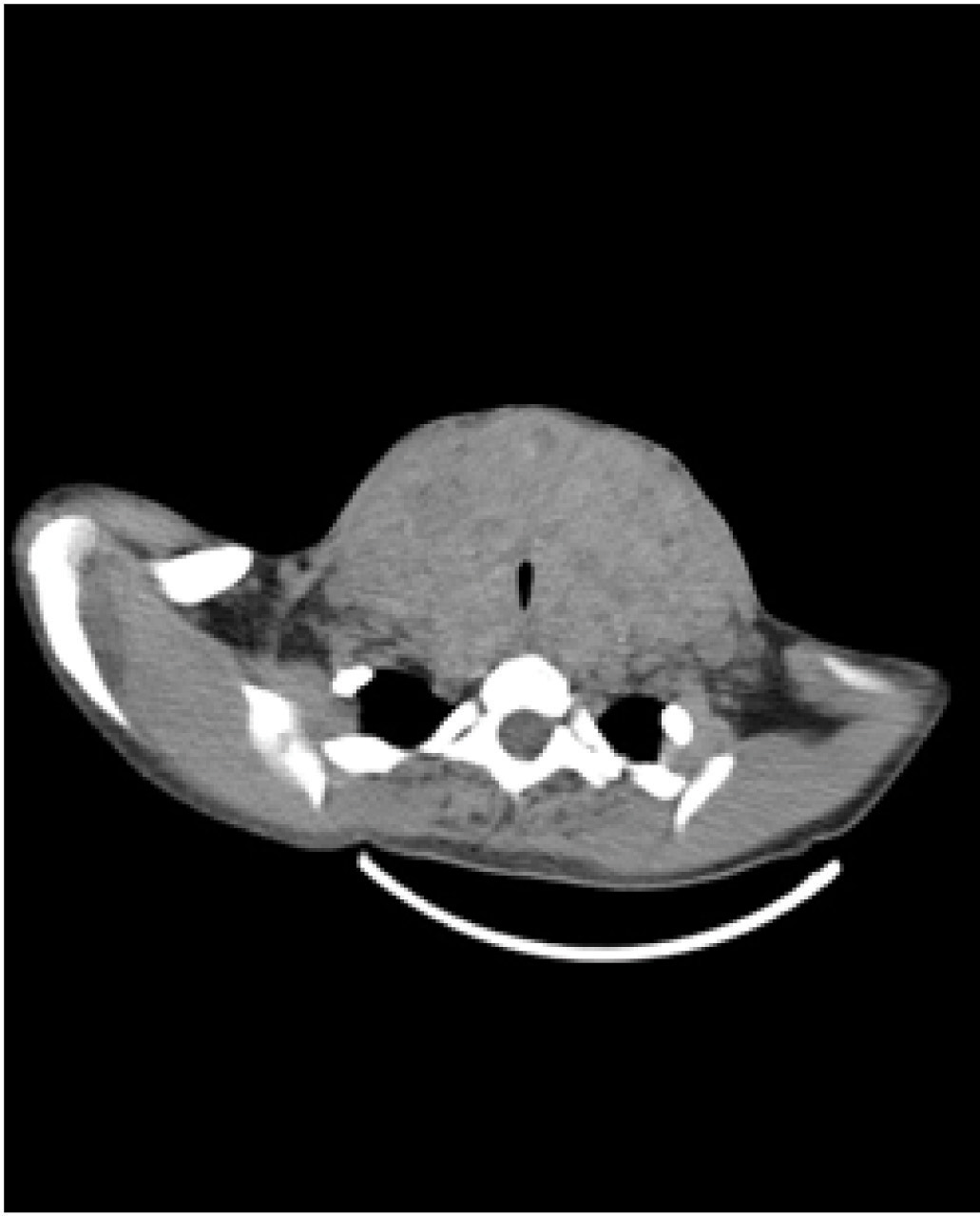
A 42-year-old lady weighing 42kg presented with large goiter since 10y. She denied history of change in voice and difficulty in breathing. She had no other comorbidities and was not on any medications. On examination her vitals were normal. A neck swelling was 15 × 10 cm in size, occupying entire anterior aspect of neck and the lower border of swelling was not palpable [Table/Fig-1]. Airway examination revealed mouth opening less than two fingers and Mallampati score 3. Neck extension was limited and flexion was severely restricted. Electrocardiogram and 2D echocardiogram were normal. Her thyroid profile and routine investigations were normal. Indirect laryngoscopy showed bilateral mobile vocal cords and posteriorly pushed trachea. X-ray neck revealed a large thyroid mass extending retrosternally with significant tracheal narrowing [Table/Fig-2]. CT scan showed diffusely enlarged thyroid gland extending from angle of mandible to retrosternal space upto arch of aorta, significantly compressing trachea with narrowest luminal diameter of 3.5 mm [Table/Fig-3].
Preoperative photograph of patient

X-ray showing tracheal compression
CT showing compression of trachea
An awake fiberoptic intubation was planned. Standard monitors were attached. Topical airway anaesthesia with lignocaine was given. Fiberoptic bronchoscope (FOB) was advanced through vocal cords with difficulty due to airway distortion. A 7.5mm flexometallic tube was threaded over the scope and its placement was confirmed by capnography. Anaesthesia was induced with propofol, fentanyl and atracurium. Anaesthesia was maintained with air, oxygen and isoflurane (1-2%). Near total thyroidectomy was performed and intraoperative feel of trachea was firm. Surgery lasted for three hours and patient remained haemodynamically stable. After reversal a significant leak was noticed on cuff deflation. On spontaneous breathing she was extubated over the FOB which showed no collapse of the trachea and bilateral mobile vocal cords.
One hour after shifting patient to the Intensive care unit (ICU), she developed sudden onset breathing difficulty and became drowsy. Facial flushing and oedema were noted. Immediately pressure bandage was removed and a tense swelling in the neck was noticed. Laryngoscopy revealed grossly edematous laryngopharynx and airway structures could not be visualized separately. A 7mm endotracheal tube was advanced assuming to be laryngeal inlet and its placement was confirmed by capnography. Chest auscultation revealed bilateral crepitations. Skin sutures were opened bedside and around 300ml of blood clots were evacuated. She had bradycardia and blood pressure could not be recorded, resuscitation was started bolus adrenaline 1mg i.v. and one liter of crystalloids was given. Noradrenaline 1μg/kg/ min were started and she was shifted to theatre for wound re-exploration.
She lost another 800ml of blood during re-exploration. All bleeding vessels were ligated and oozing from remnant thyroid tissue was cauterized. Intraoperative ABG revealed severe metabolic acidosis and haemoglobin of 8gm%.She was resuscitated with two units of packed red cells and two liter of crystalloids. She developed pulmonary oedema intraoperatively; furosemide 20mg and morphine 6mg i.v. was given. By end of the procedure patient became haemodynamically stable and was shifted to ICU. She was sedated with morphine and put on positive pressure ventilation with PEEP of 6 cm H2O. An echocardiogram showed global hypokinesia and ejection fraction(EF) of 25-30%. A Chest X ray revealed pulmonary edema. Inj dobutamine 10μg/kg/min and inj furosemide 10mg/hr was initiated. By third postoperative day all inotropes were stopped and CXR showed clearing of pulmonary opacities. Echocardiogram on third day was normal (EF- 60%). Patient was given CPAP trial for two days, which was tolerated well. On fifth day in presence of an Otolaryngologist, extubation was done over a FOB which showed minimal collapse of anterior tracheal wall, mild supraglottic oedema and right vocal cord palsy. She was extubated and had an uneventful recovery except for hoarseness of voice.
Discussion
Post-thyroidectomy haematoma is a rare but life threatening condition. Its incidence reported varies between 0.1% to 1.4% [1,2]. It may present ten minutes to a week postoperatively, most commonly occurring within 6hrs [3,4]. Its aetiology includes slipping of ligatures, reopening of cauterized veins, vomiting, bucking during recovery, and oozing from residual thyroid tissue [5,6].
The pathophysiology of airway obstruction is commonly attributed to tracheal compression due to haematoma. But a healthy trachea is unlikely to be compressed by blood clots. Compartment syndrome caused by haematoma below strap muscles can hamper venous and lymphatic drainage leading to laryngopharyngeal oedema. This could be the cause of severe airway obstruction in our case. Management of this complication includes of immediate intubation followed by evacuation of haematoma. Anaesthetist may face many challenges while intubating in such situation due to airway oedema and multiples attempts may aggravate oedema and hypoxia. Assistance by an experienced anaesthetist armed with difficult airway equipments mandatory.
Incomplete closure of strap muscles in the lower end will help to decompress the deep space in neck [4]. Performing a valsava maneuver before wound closure or placing the patient in 30° head down position to increase venous pressure to locate venous bleeding sites. Smooth recovery from anaesthesia with avoidance of fluctuations in hemodynamics is of prime importance. But at the end nothing can substitute meticulous hemostasis.
The use of pressure bandage in thyroid surgery is controversial. The pressure bandage is used extensively to compress bleeding vessels and to reduce dead space [7]. But, simultaneously it will drain all blood below strap muscles into a deeper compartment leading to airway compression. It obscures the external signs of haematoma like change in neck contour and bulging of skin flaps further delaying the diagnosis of haematoma. Drains may not offer any advantage as it will usually get blocked by blood clots and also are a poor estimate of internal blood loss. Vigilant monitoring for hypoxia is of vital importance.
Savargaonkar AP reported their experience with a post- thyoidectomy haematoma which had resulted in airway oedema [8]. Author describes the difficulty while intubating such patient.
Pulmonary oedema following thyroidectomy may result from negative intrathoracic pressure due to airway obstruction. Other causes are hypoxia, hyperadrenergic state and metabolic acidosis which further aggravates pulmonary oedema by depressing myocardial performance [9]. We ruled out tracheomalacia in this patient as there was significant leak after cuff deflation and there was no airway collapse on extubation over FOB. Absence of leak is a good predictor of tracheomalacia [10]. We also ruled out RLN palsy via visualization through FOB and she could vocalize on recovery. In our case probably multiple factors must have contributed to pulmonary oedema like laryngeal oedema, extensive bleed compressing the trachea, hypotension, myocardial depression, subsequent aggressive resuscitation with adrenaline, crystalloids and blood products. Lack of invasive pressure monitoring made it further difficult to guide fluid resuscitation. Negative pressure pulmonary oedema usually resolves rapidly without any active intervention. Our patient also responded quickly to PEEP, furosemide and morphine.
Kim WH et al., reported a similar case of pulmonary oedema in a post thyoidectomy patient. But in this case bilateral recurrent laryngeal nerve palsy was a cause for negative pressure pulmonary oedema where as in our case it resulted from severe supraglotic airway oedema [11].
Conclusion
Early detection and immediate intervention remains the principal goal to manage this complication. If immediate intubation is not possible then bedside wound decompression will help to prevent worsening of hypoxia. Primary care givers should be educated about the urgency of this situation and importance of vigilant monitoring postoperatively.
[1]. Lang BH, Yih PCL, Lo CY, A Review of Risk Factors and Timing for Postoperative Hematoma After Thyroidectomy: Is Outpatient Thyroidectomy Really Safe?World J Surg 2012 36:2497-502. [Google Scholar]
[2]. Shandilya M, Kieran S, Walshe P, Cervical haematoma after thyroid surgery: management and preventionIr Med J 2006 99:266-68. [Google Scholar]
[3]. Rosenbaum MA, Haridas M, McHenry CR, Life-threatening neck hematoma complicating thyroid and parathyroid surgeryAm J Surg 2008 195:339-43. [Google Scholar]
[4]. Calo PG, Pisano G, Piga G, Medas F, Tatti F, Donati M, Postoperative Haematomas after thyroid surgeryAnn Ital Chir 2010 81:343-47. [Google Scholar]
[5]. Lee HS, Lee BJ, Kim SW, Cha YW, Choi YS, Park YH, Patterns of Post thyroidectomy HaemorrhageClin Exp Otorhinolaryngol 2009 2:72-77. [Google Scholar]
[6]. Harding J, Sebag F, Sierra M, Palazzo FF, Henry JF, Thyroid surgery:postoperative hematoma--prevention and treatmentLangenbecks Arch Surg 2006 391:169-73. [Google Scholar]
[7]. Piromchai P, Vatanasapt P, Reechaipichitkul W, Phuttharak W, Thanaviratananich S, Is the routine pressure dressing after thyroidectomy necessary? A prospective randomized controlled studyBMC Ear, Nose and Throat Disorders 2008 8:1 [Google Scholar]
[8]. Savargaonkar AP, Post-thyroidectomy haematoma causing total airway obstruction. A case reportIndian J Anaesth 2004 48:483-85. [Google Scholar]
[9]. Lang SA, Duncan PG, Shephard DA, Ha HC, Pulmonary oedema associated with airway obstructionCan J Anaesth 1990 37:210-18. [Google Scholar]
[10]. Sinha PK, Dubey PK, Singh S, Identifying tracheomalaciaBr J Anaesth 2000 84:127-28. [Google Scholar]
[11]. Kim WH, Ryu SA, Acute pulmonary edema secondary to upper airway obstruction by bilateral vocal cord paralysis after total thyroidectomyKorean J Anesthesiol 2012 62:387-90. [Google Scholar]