Hypertension and its complications are a global concern, due to its high prevalence especially as it often remains undiagnosed [1]. In India, the prevalence of hypertension in the last six decades has increased from 2% to 25% among urban residents and from 2% to 15% among the rural residents [2]. Primary care physicians play an extremely important role as the first level of contact for individuals, screening family as well as the community in the national health system. General practioners (GPs) in India provide comprehensive primary healthcare for people of all ages and are usually the first point of contact for the health system. Studies have shown that across the globe the awareness and adherence of general practitioners and primary care physicians especially with regards to guidelines may have certain lacunae [3–8]. Adhering to goals and recommendations has the potential of contributing substantially to decreasing the national health and financial burden. We conducted a cross sectional survey of general practitioners (GPs) in the western part of Vadodara city of India to determine their approach and awareness regarding detection, evaluation and treatment of HTN.
Materials and Methods
Survey instrument
The questionnaire was prepared from guidelines of JNC7 (Joint national committee) [9] and Harrison’s principle of internal medicine (17th edition) [10]. The questionnaire comprised of questions based on the following concepts.
Technique of measurement of blood pressure
Diagnosis of prehypertension and hypertension
Evaluations of newly diagnosed hypertensive patients
Role of non-pharmacological measures to treat prehypertension and hypertension
Level of blood pressure to start pharmacological treatment
Choice of antihypertensive agents in different clinical conditions.
Sample size and sampling
This cross-sectional study was conducted in the western part of Vadodara city (total population: 1.66million) of Gujarat state. Approximately 110 GPs were practicing in western part of city and we approached 80 GPs personally who were practicing in government and private clinics or hospitals (From the list of GP Association of Vadodara city). Seventy eight GPs agreed to participate in the study. Each GP was visited by one of the authors and given the questionnaire to complete after obtaining verbal consent from them.
Statistical Analysis
The data was compiled and analyzed, using Microsoft Excel 2007.
Results
A total of 78(97.55%) GPs completed the questionnaire and their responses are analysed as below.
Majority of GPs {60(77%)} had opined that essential HTN (primary HTN) is more common then secondary hypertension [Table/Fig-1]. shows their responses for presenting symptoms of hypertension.61 (78%) GPs reported that they enquire about dietary, personal and social history. 64 (82%) GP s also inquire about other risk factors for HTN i.e. positive family history. 76 (97.4%) GPs considered stroke, 67(85%) myocardial infarction and 57(73%) considered chronic kidney disease as complications of HTN.
Presenting symptoms of hypertension
| Symptoms of hypertension | No. of Responders(%) |
|---|
| Dizziness | 57(73%) |
| Morning Headache | 36(46.15%) |
| Palpitation | 43(55%) |
| Easy fatigability | 43(55%) |
| Impotence | 2(2.56%) |
Fifty one (65.3%) GPs report that they do examine peripheral pulses as a part of the initial clinical examination but out of 51 GPs, 27(52.94%)GPs were unaware of the reason behind doing it. Twenty (43%)GPs examined it to check the volume and 7(13.7%) to rule out peripheral vascular disease. [Table/Fig-2] displays their technique of blood pressure (BP) measurement and [Table/Fig-3] shows laboratory tests ordered by GPs in their newly diagnosed hypertensive patients.
Technique of blood pressure measurement
| Technique of blood pressure measurement % | No. of correctresponders |
|---|
| Cuff placement | Covering 2/3 of arm at heart level | 63(80.76%) |
| Preferred position of patient | Sitting | 45(57.69%) |
| Supine | 23 (29.48%) |
| Standing and supine | 10(12.82%) |
| Blood pressure in both arms | | 43(55.12%) |
| No. of readings of blood pressure required to diagnose hypertension | One | 1(1.28%) |
| Two | 24(30.7%) |
| Three | 42(56%) |
| Four | 11(14.66%) |
Initial Investigations for newly diagnosed hypertensive patients
| Investigations | Number of responders(%) |
|---|
| ECG | 74(94.87%) |
| Urine examination | 53(67.94% |
| Serum creatinine | 67(85.89% |
| Lipid profile | 64(82.05%) |
| Ultrasound of Abdomen | 26(33.33%) |
| RBS | 63(80.76%) |
| Serum potassium level | 53(67.94%) |
According to JNC classification, 58(74.35%) GPs know the correct definition of prehypertension. Fifty two (66.66%) GPs have considered BP of ≥140/90 mm of hg as HTN. Fifteen(19.23%)GPs diagnose BP of 136/≥90 mm of hg as isolated diastolic hypertension (IDH) and only 13 (16.6%)GPs consider isolated systolic hypertension (ISH) for BP of 156/80 mm of hg.
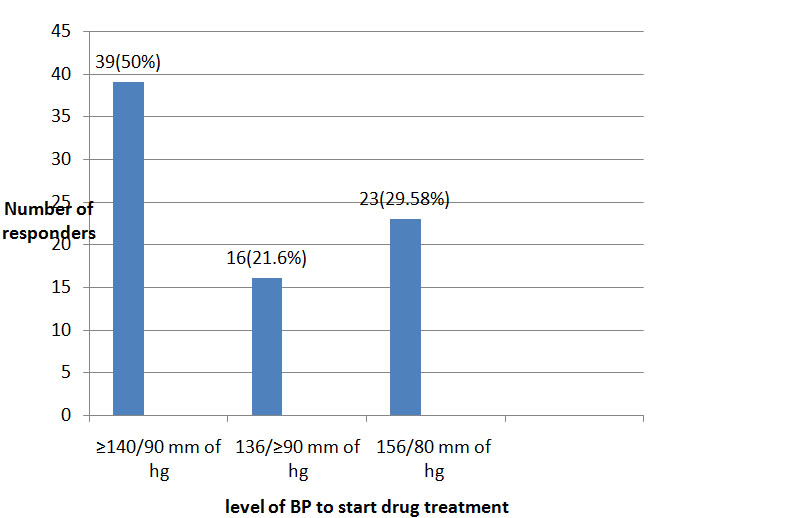
All 78 GPs responded unanimously that they advised avoiding foods having high salt and fat content like preserved foods, pickles, poppadums etc. The majority, as the preferred types of exercise, advised walking and Yoga. Sixty one (48%)GPs considered dietary modification and exercise to treat pre-hypertension where as 47(37%)GPs opined that weight loss contributes to lowering BP in pre hypertensive obese and overweight individuals. [Table/Fig-4] illustrates the thresholds to start pharmacological treatment after unsuccessful implementation of non-pharmacological measures reported by the participants.
Level of blood pressure to start pharmacological treatment after unsuccessful non pharmacological measures
[Table/Fig-5] demonstrates the choice of the class of anti hypertensive drug in different group of patients by GPs. On analysing awareness regarding side effects of anti hypertensive drugs,50(64%) GPs considered avoiding beta-blockersin COPD and asthmatic patients. Approximately 75(96%)GPs were aware about the fact that ACE inhibitors can induce dry cough in some patients as a side effect and switching to ARB (angiotens in receptor blocker) from ACE inhibitor is recommended for such patients. Pedal oedema was considered as a side effect of amlodipine by 42(53.84%) GPs. ACE inhibitor was contraindicated in pregnancy by 35(44.87%)GPs. Fourty nine(62%) GPs considered HTN as a side effect of corticosteroids. Fifty two (66%)GPs and 37(47%)GPs respectively were aware that oral contraceptive pills and ephedrine are also known to elevate blood pressure.
Choice of antihypertensive agents in different clinical conditions
| Class of drug | Uncomplicated hypertension No. of responders (%) | Patients with Coronary artery disease(CAD) No. of responders (%) | Patients with DM No. of responders (%) |
|---|
| Beta blocker | 20(27.02%) | 38(50.66%) | 12(15.38%) |
| ACE inhibitor | 8(10.8%) | 18(24%) | 50(64.10%) |
| Calcium channel blocker | 30(40.54%) | 12(16%) | 12(15.38%) |
| Diuretics | 16(21.62%) | 7(9.33%) | 4(5.12%) |
Discussion
This study investigated the approach and management of hypertension of general practitioners from the western part of Vadodara city in the state of Gujarat,India with a population of 1.66 million. Analysis of the results show that majority of the GPs are aware of the common presenting symptom of hypertensive vascular disease and the importance of asking family history of hypertension and other cardiovascular disease. Most GPs do examine peripheral pulses but the reasons to examine peripheral pulses in hypertensive patients do not seem clear. Review of history taking and importance of physical examination in routine clinical practice should be stressed in future CMEs.
Correct measurement and interpretation of the BP (BP) is essential in the diagnosis and management of HTN. Popular and commonly used auscultatory office BP measurement has major shortcomings [11]. Surveys of mercury devices in clinical practices have shown that there are frequently mechanical defects, and physicians’ rarely follow official guidelines for their use [12]. In our study, we observed incongruous techniques for applying the cuff by some of the GPs. Very few GPs reported measuring BP in the supine and standing position and in both arms and by doing so they are prone to miss the diagnosis of orthostatic hypotension and underlying vessel disease respectively [13]. Patients with newly identified hypertension should be seen at two further visits before a decision about treatment is made [14]. In the present study 30.7% GPs take less than three measurements of BP to diagnose HTN and this may lead to over or under diagnosis. Similar barriers to adherence to national and international guidelines by GPs are reported in other countries.In Saudi Arabia a study by Al Gelben KS et al., showed that only 5% of physicians measured blood pressure with patients standing and sitting [15]. In another study carried out in China by Qian Chen et al., on GP’s hypertension knowledge and training needs showed 44.2% of GPs believe that hypertension can be diagnosed if two measurements on different days show systolic blood pressure >140 mm of hg and/or diastolic blood pressure> 90 mm of hg [8]. Similarly, a study in Australia on management of hypertension in general practice revealed uncertainty regarding the best way to measure, record and interpret blood pressure [16].
HTN is a major risk factor for myocardial infarction, cerebral vascular disease, chronic renal failure [17–20]. So screening patient’s for other concomitant diseases and complications of HTN is a must at the time of diagnosis to decrease morbidity and mortality. In our study most GPs do report screening their patients by ordering the necessary tests at the time of diagnosis and seem well aware about the complications of HTN.
Comprehensive lifestyle modification is essential for management of HTN [20]. Baseline information regarding diet and lifestyle is necessary before advising dietary and lifestyle modification but one third of GPs in our study do not seem to enquire about it in their practice. Though, non pharmacological measures are advised by most of GPs to their hypertensive patients, not asking baseline information regarding those may result in to inadequate and perfunctory counseling. Moreover, non-pharmacological measures are still widely underused in the treatment of prehypertension. Little less than half of the GPs consider dietary modification, exercise and weight loss in the treatment of prehypertension. This approach can result in many untreated prehypertensive patients progressing to HTN and related complications [10]. Similarly, a study by Qian et al., in China showed that 7 in 10 physicians spend only one third to one quarter of their practice time during consultation to educate patients about lifestyle changes that may help to reduce blood pressure and benefit their health status [8]. Although, individual counseling is time consuming and can prove challenging in a busy general practice, using brochures, posters and group sessions in their clinics and waiting rooms maybe the answer.
Very few GPs considered diagnosis and treatment of IDH(DBP ≥90 mm of hg with SBP of <140 mm of hg.) [Table/Fig-4]. Although, the importance of IDH may be still uncertain [21], it has been recommended that subjects with IDH should be monitored over time as they tend to have other concomitant cardiovascular risk factors and their management should focus on the control of all major cardiovascular factors and not solely the optimization of BP [22].
One of the most worrisome findings in our study is the under diagnosis and under treatment of ISH and Systolic diastolic hypertension (SDH)by most of GPs [Table/Fig-4]. ISH is responsible for endothelial dysfunction and a prothrombotic state as similar as SDH and treatment of it significantly decreases over all mortality, cardiovascular mortality and stroke rate. Disregarding its diagnosis and treatment increases the prevalence of complications in community [22]. A similar study which was carried out on 1000 GPs of urban Pakistan in 2002 by Jafar et al., showed that 69.4% GPs diagnosed hypertension. However, awareness on diagnosis were not studied and it showed significant under treatment of HTN in patients> 60 years [3]. The present study demonstrates a deficiency in the diagnosis and treatment of IDH,ISH as well as SDH by GPs. Future CMEs should address these lacunae in their approach. Standard guidelines for diagnosis and treatment of HTN should be simplified in such a way that it’s easy to remember and practice for GPs. Large studies in Europe to understand the attitudes and awareness of physicians in the management of hypertension and the adherence to guidelines have also shown that physicians may be undertreating their patients and underestimating the challenge of achieving blood pressure targets [5–7].
Thiazide type of diuretics should be used in drug treatment for most patients with uncomplicated HTN, either alone or combined with drugs from other classes. Diuretics enhance the antihypertensive efficacy of multidrug regimens, can be useful in achieving BP control, and are more affordable than other anti hypertensive agents. Despite these findings diuretics remain underused [3,9,15]. Our study demonstrates the same results for using diuretics for treatment of uncomplicated HTN [Table/Fig-5]. India is a developing country and patients or government endures cost of medicine. So the use of cost effective and potent anti hypertensive medicine should be promoted among physicians.
Choosing the correct drug as per individual patient requirement plays a pivotal role in optimizing management, also important is identifying side effects of the drug to increase patient compliance and prevent treatment complications [15]. Most GPs in the study seemed well aware about using ACE inhibitor to treat HTN in diabetic patients and side effects of beta-blocker and ACE inhibitors. Though betablockers are the preferred antihypertensive agent for patients with coronary artery disease (CAD), only48% of GPs considered using it. Although CAD, diabetic and pregnant hypertensive patients are usually treated by specialists but basic awareness regarding choice of anti hypertensive agent in concomitant medical condition is important.
Limitations
GPs from urban area were included so it failed to provide any insight of clinical practice by GPs in rural areas. We believe that studying characteristics of GPs such as their age,gender,time since graduation, type of practice (government or private hospitals, teaching or non teaching institutions) would make them feel uncomfortable and to be judged. Motivation for future CMEs or other means for regular updates on recent advances and guidelines were not assessed [23]. However, analysing these characteristics might assist in creating effective measures to improve care.
Conclusion
Considering the wide scope of clinical practice of GPs, they are well aware and updated about some aspects of diagnosis and treatment of HTN but may lack an effective approach towards history taking for HTN,diagnosis and treatment of IDH, ISH and SDH.Also some deficits in the technique for taking BP measurements are apparent. Treatment of pre-hypertension is disregarded and non-pharmacological measures are underused to treat it. Thiazide diuretics seem to be underutilized for treatment of uncomplicated HTN and beta blocker are often not considered as the preferred anti hypertensive in CAD. This study gives us an insight into their approach and awareness regarding recent guidelines and updates for treatment of HTN which may be utilized in the future in a strive towards effective control of blood pressure and related risk factors at the primary health care level. Measures like in regular CME (compulsory or otherwise) for GPs or recertification exams have been shown to be effective and may be the solution to address the lacunae identified.