Azithromycin-Induced Rash in a Patient of Infectious Mononucleosis – A Case Report with Review of Literature
Indranil Banerjee1, Somnath Mondal2, Sukanta Sen3, Santanu Kumar Tripathi4, Gautam Banerjee5
1 Final year Post-Doctoral Trainee, Department of Clinical and Experimental Pharmacology, School of Tropical Medicine, Kolkata, West Bengal, India.
2 Technical Associate, ADR Monitoring Centre, Department of Clinical and Experimental Pharmacology, School of Tropical Medicine, Kolkata, West Bengal, India.
3 Second Year Post-Doctoral Trainee, Department of Clinical and Experimental Pharmacology, School of Tropical Medicine, Kolkata, West Bengal, India.
4 Professor and Head, Department of Clinical and Experimental Pharmacology, School of Tropical Medicine, Kolkata, West Bengal, India.
5 Professor and Head, Department of Dermatology, School of Tropical Medicine, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Indranil Banerjee, DM (Clinical Pharmacology) Post-doctoral Trainee, Department of Clinical and Experimental Pharmacology, School of Tropical Medicine, Kolkata, West Bengal, India. Phone : 9432184197, E-mail : dronineo@yahoo.co.in
Antibiotic induced skin rash in setting of infectious mononucleosis is often encountered in clinical practice. However, macrolides like azithromycin are considered relatively safe and till date only two cases of azithromycin induced rash in setting of infectious mononucleosis have been reported. The following report illustrates the case of a 23-year-old man suffering from infectious mononucleosis who exhibited a generalized cutaneous rash following treatment with azithromycin. Using the Naranjo ADR probability scale, this case of acute onset rash following azithromycin administration was found to be in ‘probable’ category. The mechanism of antibiotic-induced rash in patients suffering from infectious mononucleosis is incompletely understood. It has been suggested that the rash could result from virus mediated immunomodulation or due to altered drug metabolism. The report calls for cautious use of antibiotics in the setting of suspected viral infections like infectious mononucleosis as injudicious use might increase the risk of deleterious skin reactions and increase the cost of healthcare.
Azithromycin, Infectious Mononucleosis, Rash
Case Report
A 23-year-old male patient presented in the Dermatology OPD with complaints of a pruritic rash distributed all over his body. He gave a history of fever with sore throat, malaise, fatigue three days back for which he consulted a general practitioner. He was prescribed tablet azithromycin (500 mg) once daily for six days. Two days after complying with the prescription, patient observed a pruritic rash distributed throughout his body. On physical examination, there was a diffuse, symmetric, generalized maculopapular eruption with no evidence of any mucosal involvement. An erythematous patch was observed in the posterior oropharynx. His lungs were clear on auscultation. There was no evidence of hepatosplenomegaly. There was no significant personal or family history of similar kind of cutaneous adverse reaction on exposure to any drug. A thorough lab investigation for complete blood count (CBC), liver function tests (LFT), estimation of serum urea, creatinine, mono spot test and throat culture was ordered. The significant laboratory findings included mild decrease in hemoglobin (Hb%) - 10.2gm/dl (Normal range 13-14gm/dl in males), raised total leukocyte count - 14,200/cubic mm (4000-11,000/cubic mm), raised lymphocytes - 56%, and decreased neutrophils - 32%. The monospot test was found to be positive. These findings were in concordance with the diagnosis of infectious mononucleosis (IM). The dermatologist stopped azithromycin treatment and advised topical 0.1% triamcinolone cream to be applied locally twice daily and 5mg of levocetrizine tablet to be taken orally twice daily for two weeks. On follow-up, the patient reported complete resolution of his pruritus and rash within one week of treatment. Using the Naranjo ADR probability scale [1], this case of acute onset rash following azithromycin administration was found to be in ‘probable’ category, with a score of five.The case has been duly reported to the Pharmacovigilance Programme of India (No. IN-IPC-2013-21868). A written informed consent was obtained from the patient for publication of this case report and accompanying image.
Discussion
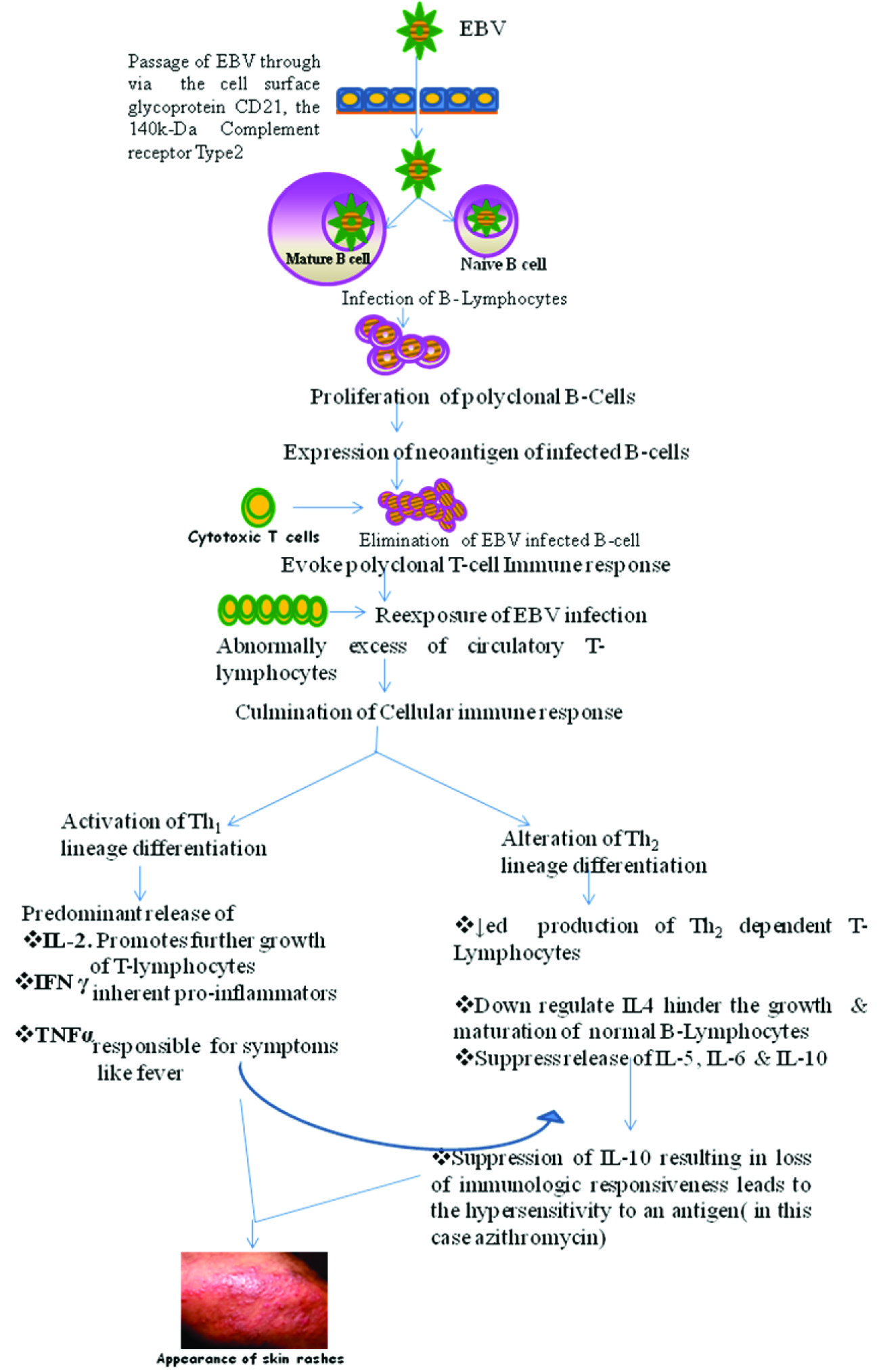
Infectious mononucleosis is caused by Epstein-Barr virus (EBV) which primarily affects older children and young adults [2]. Skin rashes in infectious mononucleosis has been reported with the use of antibiotics like ampicillin, amoxicillin [3,4], cephalexin [5], minocycline [6]. However, macrolides like azithromycin are considered relatively safe in this respect and despite our diligent search, we find only two cases of azithromycin-induced rash in setting of IM in the published literature [7,8]. The salient features of the earlier two cases have been compared with the present case report in [Table/Fig-1]. The mechanism of antibiotic-induced rash in setting of IM is not fully understood. It is hypothesized that the skin rash could result from EBV mediated immunomodulation or due to an altered drug metabolism caused by the disease. Virus induced abnormal immunomodulation in IM patients is believed to be a key factor for development of skin rashes during concomitant antibiotic therapy [9]. Patients infected with EBV have an increased level of circulating Th1 lymphocytes which produce cytokines like interleukin (IL)-2, interferon (IFN)-gamma, and tumor necrosis factor-alpha (TNF-α). Interferon-gamma inhibits the function of Th2 lymphocytes with consequent decrease in cytokines secreted by them like IL-5, IL-6, and IL-10 [7]. The suppression of IL-10 is associated with consequent loss of immune tolerance resulting in hypersensitivity to an antigen, which in the case of antibiotics - in this case, azithromycin - could manifest as drug rashes. This has been schematically detailed in [Table/Fig-2]. In 1974, Webster and Thompson suggested that ampicillin polymer-mediated lymphocyte stimulation could play a critical role in the development of the skin rash seen in IM patients on concomitant ampicillin therapy [10]. In this perspective, it is only speculated that the high molecular weight soluble antigens of azithromycin or of any of its metabolites might have played a similar role in development of rashes in the IM patient, and this remains to be investigated. A well designed in-vitro study to examine this hypothesis is warranted.
Salient features of the two already published cases as compared with the present case report
| Schissel DJ [7] | Dakdauki et al., [8] | Present case |
|---|
| Age and sex of the patient | 20 years old, male patient | 19 years old, male patient | 23 years old, male patient |
| Occurrence of rash | Two days after completion of 5 day course of azithromycin | On the same day of starting azithromycin therapy | Two days after starting azithromycin therapy |
| Clinical features | Cervical lymphadenopathy, mild posterior pharyngeal wall erythema | Cervical and inguinal lymphadenopathy, pharyngeal erythema, hepatomegaly | Cervical lymphadenopathy, posterior pharyngeal wall erythema |
| Lab findings | WBC 11,700/ cu.mm Lymphocytes: 68% Monospot test : Positive | WBC 10,900/ cu.mm Lymphocytes: 40% Neutrophils: 47% Monospot test : Negative Hepatomegaly | WBC 14,200/ cu.mm Lymphocytes: 56% Neutrophils: 32% Monospot test: Positive |
| Outcome | Pruritus resolved in two days and eruptions after five weeks of stopping azithromycin. | Resolved within two weeks after stoppage of therapy. | Resolved within one week of stopping azithromycin therapy. |
Proposed mechanism of azithromycin induced rash in infectious mononucleosis
Conclusion
In routine clinical practice, physicians have a tendency to prescribe antibiotics to patients presenting with fever and sore throat without exploring the underlying aetiology. The current case report calls for judicious use of antibiotics in setting of suspected viral infections like IM as indiscriminate antibiotic use might invoke deleterious skin reactions and thus increase the cost of healthcare.
[1]. Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberst EA, A method for estimating the probability of adverse drug reactionsClin Pharmacol Ther 1981 30:239-45. [Google Scholar]
[2]. Luzuriaga K, Sullivan JL, Infectious mononucleosisN Engl J Med 2010 362:1993-2000. [Google Scholar]
[3]. Chovel-Sella A, Ben Tov A, Lahav E, Mor O, Rudich H, Paret Incidence of rash after amoxicillin treatment in children with infectious mononucleosisPediatrics 2013 131:e1424-27. [Google Scholar]
[4]. Shapiro S, Slone D, Siskind V, Lewis GP, Drug rash with ampicillin and other penicillinsLancet 1969 8:969-72. [Google Scholar]
[5]. McCloskey GL, Massa MC, Cephalexin rash in infectious mononucleosisCutis 1997 59:251-54. [Google Scholar]
[6]. Lupton JR, Figueroa P, Tamjidi P, Berberian BJ, Sulica VI, An infectious mononucleosis-like syndrome induced by minocycline: a third pattern of adverse drug reactionCutis 1999 64:91-96. [Google Scholar]
[7]. Schissel DJ, Singer D, David-Bajar K, Azithromycin eruption in infectious mononucleosis: a proposed mechanism of interactionCutis 2000 65:163-67. [Google Scholar]
[8]. Dakdouki GK, Obeid KH, Kanj SS, Azithromycin-induced rash in infectious mononucleosisScand J Infect Dis 2002 34:939-41. [Google Scholar]
[9]. Huston DP, The biology of the immune systemJAMA 1997 278:1804-14. [Google Scholar]
[10]. Webster AW, Thompson RA, The ampicillin rash: lymphocyte transformation by ampicillin polymerClin Exp Immunol 1974 18:553-64. [Google Scholar]