Oral Manifestations in a Renal Osteodystrophy Patient - A Case Report with Review of Literature
Parthiban J1, Aarthi Nisha V2, Asokan GS3, Prakash CA4, Varadharaja MM5
1 Reader, Department of Oral and Maxillofacial Surgery, Tagore Dental College and Hospital, Chennai, Tamil Nadu, India.
2 Senior Lecturer, Department of Oral Medicine & Radiology, Sree Balaji Dental College & Hospital, Bharath University, Chennai, Tamil Nadu, India.
3 Reader, Department of Oral Medicine and Radiology, Tagore Dental College and Hospital, Chennai, Tamil Nadu, India.
4 Reader, Department of Oral Surgery, CSI Dental College & Hospital, Madurai. Tamil Nadu, India.
5 Senior Lecturer, Department of Orthodontics, Tagore Dental College and Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Parthiban J, Reader, Department of Oral and Maxillofacial Surgery, Tagore Dental College and Hospital, Rathinamangalam, Vandalur, Chennai, India. Phone : +91-09500027640, +91-09443529399, E-mail : drparthij@yahoo.in
Renal Osteodystrophy (ROD) is a common complication of chronic renal disease (CRD) and is the part of a broad spectrum of disorders of mineral metabolism that occurs in the clinical setting. It occurs early in the course of chronic renal failure and progresses as the kidney function deteriorates. It is an osseous alteration believed to arise from increased parathyroid function associated with inappropriate calcium, phosphorus and vitamin D metabolism. Involvement of the jaws is common and radiographic alterations are often one of the earliest signs of chronic renal failure. Herein, reporting a case of Chronic Renal Failure (Bilateral Grade I Neuropathy) with ROD presenting oral manifestations in an 11-year -old male child.
Renal osteodystrophy, Hyperparathyroidism, Vitamin D deficiency, Oral manifestations
Case Report
An 11-year-old male child reported with a chief complaint of loss of his front teeth along with spacing of upper and lower teeth of his jaws since six months. The patient was apparently normal three years back when his parents suddenly noticed mobility of teeth with drifting and his maxillary right and left central incisors started to become mobile and eventually got exfoliated. Medical history revealed that he was suffering from chronic renal failure (Bilateral Grade I Nephropathy) and was known hypertensive since one year. Patient has also loss of weight and inability to stand or walk unsupported since one year. He was also on haemodialysis since six months and on medications such as diuretics, calcium channel blockers, calcitriol and multivitamins since one year. He was advised to take high potassium and a low protein diet. He was reported to dentist for the first time. Family and personal history were noncontributory. General physical Examination revealed that patient had stunted growth with bowing of legs [Table/Fig-1]. Head was normal but the inferior face was widened due to maxillary and mandibular overgrowth. Generalized pallor of skin nails and palpebral conjunctiva was observed. Extaoral examination revealed generalized swelling of the labial surface of alveolus that produced enlargement of maxilla and mandible [Table/Fig-2]. Swelling was non tender, non compressible on palpation. Intraorally, on inspection, patient had delayed eruption of permanent teeth compared to that age group. Upper maxillary central incisors were missing [Table/Fig-3] with drifting of maxillary lateral incisors. Mandibular anteriors were present. There was presence of generalized enamel hypoplasia. There was no tenderness on palpation. Patient had poor oral hygiene, halitosis suggestive of uremic odour with increased calculus formation on the teeth. Salivary secretions were reduced leading to xerostomia. Tongue blade sign was positive in this case which indicated xerostomia. Soft tissue examination revealed generalized gingival inflammation, gingival recession and periodontal pockets were present. Generalized erythema of buccal and labial mucosa was noticed.
Based on history and clinical examination a provisional diagnosis of Renal Osteodystrophy (ROD) was given. Rickets, hypothyroidism, hyperparathyroidism, hypopituitarism were considered under the differential diagnosis. Periapical Radiograph of maxillary central and lateral incisors revealed missing maxillary right and left central incisors with drifting of maxillary right and left lateral incisors which were having wide open apex. Periapical Radiograph of Mandibular anteriors revealed teeth with open apex and narrow pulp chamber.
Stunted growth and bowing of legs

Enlargement of maxilla and mandible

Missing maxillary canines multiple with increased spacing

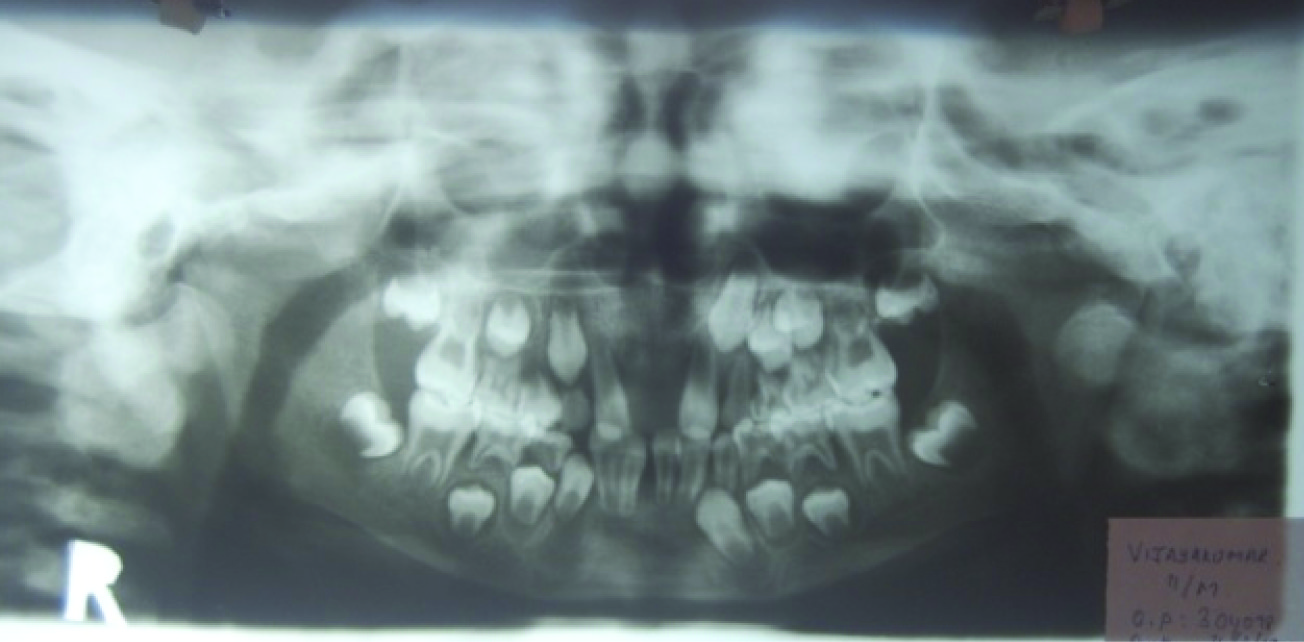
Panoramic Radiograph [Table/Fig-4] showed multiple teeth in the erupting and exfoliating stage (mixed dentition) with wide open apex and narrow pulp chambers, delayed eruption of the permanent teeth compared to that age group was also observed. Diffuse lytic areas of bone were present with loss of inferior cortical thickness. In addition, there was reduction of trabecular pattern which assumed a ground glass appearance. Ultrasonography of the abdomen confirmed the presence of bilateral renal nephropathy.
Panoramic radiograph showing teeth in the erupting and exfoliating stage, diffuse lytic areas of bone with loss of inferior cortical thickness and reduction of trabecular pattern with ground glass appearance
Patient was subjected to various haematological investigations [Table/Fig-5].
Investigations done for the patient
| Investigations | Observed Values | Normal Values |
|---|
| Total Red Blood Cell Count | 3.5 million cells /mm3 | 4.2-5.4million cells/mm3 |
| Hb% | 9.9 gm% | 14.5 gm/dL |
| Hematocrit value / Packed Cell Volume | 32% | 38-48% |
| Total White Blood Cell Count | 87,000 cells/mm3 | 4000-11000 cells/mm3 |
| - Neutrophils | 68 | 40-74 |
| - Eosinophils | 4 | 1-7 |
| - Basophils | 00 | 00 |
| - Lymphocytes | 26 | 20-40 |
| - Monocytes | 02 | 1-9 |
| Erythrocyte Sedimentation Rate | 100mm/hour | 0-9 mm/hour |
| Peripheral blood smear | Normocytic Normochromic Anemia | _ |
| Platelet count | 2.48 lacs /mm3 | 1.5-4.5 lacs /mm3 |
| Activated Plasma Prothrombin time | 49.3 seconds | 18-45 seconds |
| Prothombin Time | 15.9 seconds | 10-15 seconds |
| INR ratio | 1.08 | 0.9-1.2 |
| Blood group | O+ | - |
| Serum Calcium | 5.9 lacs /mm3 | 9-11.5 lacs /mm3 |
| Serum phosphorus | 3.6 mg/dl | 4.5-6 mg/dl |
| Random Blood sugar | 83mg/dL | 90-150 mg/dL |
| Urea Nitrogen (BUN) | 47mg/dL | 5-35 mg/dL |
| Alkaline phosphatase | 638 U/L | 50-136 U/L |
| Serum Creatinine | 3.1 mg/dL | 0.8-1.3 mg/dL |
| Serum Sodium | 185 mmol/L | 135-145mmol/L |
| Serum Potassium | 4.5 mmol/L | 3.5-5.1 mmol/L |
| Serum Chloride | 119 mmol/L | 95-105 mmol/L |
| C. Reactive protein | 0.8mg/dL | > 1.0 mg/dL |
| Rheumatoid Factor | Negative | - |
| VDRL | Negative | - |
| HIV and HBsAg | Negative | - |
| Urine protein | 338/24 hrs | > 150mg/day |
| Urine Volume | 1000ml/ day | 750-2000ml/day |
| Parathyroid hormone(PTH) | 108 pg/ml | 10-70pg/ml |
| Serum Triglycerides | 134mg/dL | - |
| Serum Vitamin D | 13pg/ml | - |
Based on the investigations, in this case serum calcium was below normal and parathyroid hormone (PTH) was above normal which suggested secondary hyperparathyroidism. Low haemoglobin levels indicated that the patient was anaemic. Increased serum levels of creatinine, erythrocyte sedimentation rate, BUN, sodium, alkaline phosphatase (ALP), urinary levels of protein were observed in the case. These findings were deemed consistent with chronic renal failure. Increased Alkaline phosphatase levels were responsible for the diffuse lytic areas in the bone which were observed radiographically. Based on the above findings, final diagnosis of Oral Manifestations of ROD was given.
Patient was referred to the Department of Orthopaedics for rehabilitation prosthesis and nephrology for dialysis procedure. Before initiating medical treatment, as a part of dental hygiene programme, oral hygiene improvement measures were commenced for the patient. Patient’s full mouth scaling was performed and teeth with mobility and poor prognosis were extracted under antibiotic prophylaxis with oral antibiotics to prevent the future bacterial endocarditis. The medications included oral antifungals Candid-B mouth paint to prevent secondary candidal infections and were advised to continue the diuretics, nifedipine, calcitriol, multivitamins which he was already taking since one year.
Medical management has commenced for the patient with good dental hygiene. Patient has been planned for full mouth rehabilitation after dialysis procedure is done. The patient’s dental followup was uneventful and under regular check up every month during his dialysis procedure.
Discussion
Chronic renal disease (CRD) is a multifactorial syndrome characterized by progressive and irreversible loss of renal mass and function, representing a major health concern. Diabetes mellitus, hypertension, chronic glomerulonephritis, and systemic lupus erythematosus are the most common causes of this disorder [1]. ROD can generate a wide range of oral facial and dental manifestations, such as gingival hyperplasia, periodontal disease, xerostomia, lichen planus, uremic stomatitis, candidiasis, herpes simplex, delayed dental eruption, enamel hypoplasia, dental mobility and ROD [2]. ROD is a multifactorial and complex entity that includes not only the response of bone in CRD but also its response to different therapies. It is an osseous alteration believed to arise from increased parathyroid function associated with inappropriate calcium, phosphorus and vitamin D metabolism [3]. ROD is a common complication of CRD and it is the part of a broad spectrum of disorders of mineral metabolism that occurs in the clinical setting. It occurs early in the course of chronic renal failure and progresses as the kidney function deteriorates [4].
It is the result of variety of complex interrelationships between serum calcium, phosphorus, parathyroid hormone, and 1, 25 –dihydroxyvitamin D. The most common bone lesion is a consequence of secondary hyperparathyroidism leading to changes in bone that are similar to those of fibrous osteitis cystica , and to physeal changes resembling those of rickets [5]. ROD represents a spectrum of microscopically and pathogenetically discrete form of bone disease that can be divided into two broad categories: high turnover disease (osteitis fibrosa ) and low turnover disease (Osteomalacia and adynamic bone disease). Osteitis fibrosa is the most common type of renal osteodystrophy affecting approximately 30% of patients with end stage renal disease [5]. Although adults who have early chronic renal insufficiency may have normal serum levels of 1, 25 – dihydroxyvitamin D, a disturbance of vitamin D is seen early in children who have chronic renal insufficiency. Poor gastrointestinal absorption of calcium due to lack of the dihydroxylated form of vitamin D that is normally produced by healthy kidneys also contributes to the hypocalcaemia and secondary hyperparathyroidism. Secondary hyperparathyroidism affects up to 92% of patients receiving hemodialysis [6]. In our case this was the most common cause for osseous alterations seen in ROD.
Like any other systemic disease, CRD can cause oral manifestations. One of the early symptoms may be an unpleasant odour in the mouth particularly in the morning . This uremic fetor, an ammonical odour is typical sign of all uremic patients caused by high concentration of urea in the saliva. Severe xerostomia is a common finding with a prevalence of 73.2%. If CRF begins early in life enamel hypoplasia may develop which is due to disturbances in calcium and phosphate metabolism. In developing dentition red brown discoloration, delayed or altered eruption may be seen. Tooth mobility and drifting lead to malocclusion. Impaired calcium and phosphorus balance can cause narrowing of pulp chamber and increase the incidence of dental calculus. In some patients marked jaw enlargement is present. Most of the clinical manifestations were present in our case leading to the diagnosis of oral manifestations of ROD [7].
A variety of biochemical markers and radiographic findings have been employed in the diagnosis and monitoring of ROD. Serum parathyroid hormone (PTH) and total alkaline phosphatase (ALP) remain the most widely used biochemical tests for ROD [8]. Increased levels of PTH and total ALP were noted in the present case [1].
Diagnosis of the specific osteodystrophy type is a rather complex process and various biochemical markers and radiographic findings are used so as to facilitate this stage [1]. As a result of dietary control and long term dialysis therapy, many patients with serious renal disease live for extended periods. Hemodialysis is used approximately in 80 % of affected patients .Some recent studies have documented that patients receiving long term hemodialysis may have uremic mixed bone disease with osteitis fibrosa and osteomalacia and it can also be associated with macrognathia [9]. Dental treatment strategy should emphasize oral hygiene and patients should be reinforced frequently in hygiene performance. Symptomatic treatment should include oral antibiotics to prevent the future bacterial endocarditis and oral antifungals should be prescribed to prevent secondary candidal infection [10].
Conclusion
The incidence of CRD continues to rise worldwide and, as a consequence increasing numbers of individuals with such disease will probably continue to require oral health care. In such a scenario, the dentists are frequently encountered with patients who have oral manifestations both due to renal disease and haemodialysis. So, the systemic evaluation of the patient should be done before diagnosing the oral lesions. Also, we can avoid the potential complications that may arise when we treat such patients and provide them good oral hygiene. Hence, we conclude that oral manifestations of systemic diseases are more frequent and as dentists, we have a vital role in treating them accordingly.
[1]. Kalyvas D, Tosios KI, Leventis MD, Localized Jaw enlargement in renal osteodystrophy.Report of a case and review of the literatureJ of Oral Surg Oral. Med Oral Pathol Oral radiol Endod 2004 97:68-74. [Google Scholar]
[2]. Proctor R, Kumar N, Stein A, Moles D, Porter S, Oral and dental aspects of chronic renal failureJ Dent Res 2005 84:199-208. [Google Scholar]
[3]. Damm DD, Neville BW, Kenna Mc, Macrognathia of renal osteodystrophy in dialysis patientsJ of Oral Surg Oral Med Oral Path Oral Radiol Endod 1997 83:489-83. [Google Scholar]
[4]. Mozaffari PM, Amirchaghmaghi M, Mortazavi H, Oral Manifestations of Renal Patients Before and after transplantation: A review of literatureDHJ 2009 11:83-6. [Google Scholar]
[5]. Narula A.S., Jairam A, Baliga K.V., Singh K.J, Pathogenesis and management of renal osteodystrophy. Review articleIndian J of nephrology 2007 17:4-7. [Google Scholar]
[6]. Corte C D, Diaz MLN, Prevention, Prevention, diagnosis and treatment of renal osteodystrophy in Spain. Preliminary results from a multicentre enquiryNephrol Dial Transplant 1998 13(3):51-56. [Google Scholar]
[7]. Kaufman DB, Growth hormone and renal Osteodystrophy : a case reportPediatr Nephrol 1998 12:157-59. [Google Scholar]
[8]. Oppenheim WL, Namba R, Aluminium Toxicity Complicating Renal OsteodystrophyThe J of bone and Dental Surgery 1989 71:446-52. [Google Scholar]
[9]. Hata T, Irei I, Tanaka K, Nagatsuka H, Hosoda M, Macrognathia secondary to dialysisrelated renal osteodystrophy treated successfully by parathyroidectomyInt J Oral Maxillofac Surg 2006 35:378-82. [Google Scholar]
[10]. Benjelloun M, Tarrass F, Alaoui L, Medkouri G, Hachim K, Gharbi MB, Marked facial enlargement in secondary hyperparathyroidismNephrol Dial Transplant 2007 22:3082-83. [Google Scholar]