Vanishing Testis Syndrome: Report of Two Cases
Priya Dhandore1, Narendra Narayan Hombalkar2, Prakash Dattatray Gurav3, Mohd Hamid Shafique Ahmed4
1Assistant Professor, Department of Surgery, Government Medical College, Miraj, Maharashtra, India.
2Assistant Professor, Department of Surgery, Government Medical College, Miraj, Maharashtra, India.
3Professor and Head, Department of Surgery, Government Medical College, Miraj, Maharashtra, India.
4Third Year Junior Resident, Department of Surgery, Government Medical College, Miraj, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohd. Hamid Shafique Ahmed, Third Year Junior Resident, Department of Surgery, Government Medical College, Miraj - 416416, Maharashtra, India. Phone : +919224684554, E-mail :khanmohdhamid@gmail.com
Vanishing testis syndrome or Testicular regression syndrome (TRS) is defined as the absence or an incomplete development of the testis of varying degrees in 46XY patients with normal external genitalia.TRS or vanishing testis syndrome may be seen in less than 5% of all patients of cryptorchidism. We report two cases of TRS who underwent surgical exploration with an initial diagnosis of cryptorchidism with impalpable testis. Grossly testicular tissue was not identified and the vas deferens was ending into a nubbin in both the cases. The presumed testicular remnants were sent for histological examination. The histological sections in both the cases showed vascularised fibrous nodule, structure of the spermatic cord and calcification, supporting the diagnosis of TRS.
Testicular regression syndrome, Vanishing testis syndrome, Vascularised Fibrous nodule
Case Report
Case 1
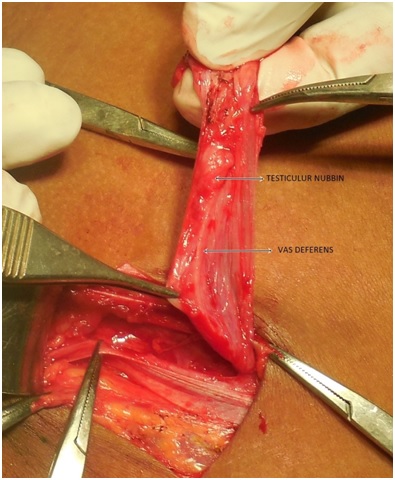
A 11-year-old boy presented with absence of both the testes in scrotal sac since birth. On clinical examination right testis is palpable in inguinal canal while the left testis is not palpable in inguino scrotal region. On ultrasonography the right testis was seen in the inguinal canal and measured 1.4 cm x1.0 cm. The left testis was not visualized along the normal pathway of descent or even in the ectopic locations. Orchidopexy was done on the right site and left inguinal exploration revealed a small hernial sac. There was no evidence of testicular tissue in the inguinal canal but the left sided vas deference was evident. Left sided spermatic cord with small oval testicular nodule at its distal end [Table/Fig-1] were sent for histopathological examination.
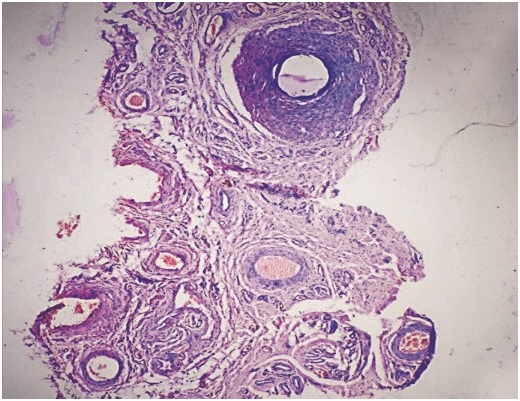
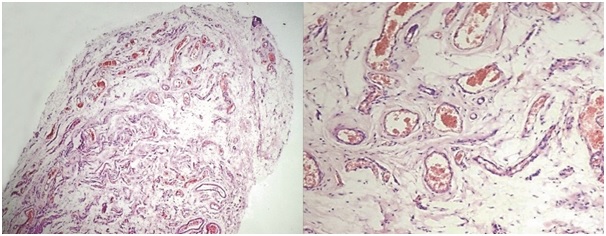
Histopathological examination showed spermatic cord, rudimentary epididymis [Table/Fig-2] and tunica with underlying vascularised fibrous nodule showing few hemosiderophages [Table/Fig-3] . Spermatic tubules, germinal cells, leydig cells and rete testis were not seen. The diagnosis of TRS was made by identification of vascularised fibrous nodule (VFN) in the proximity of spermatic cord and epididymis.
Case 2
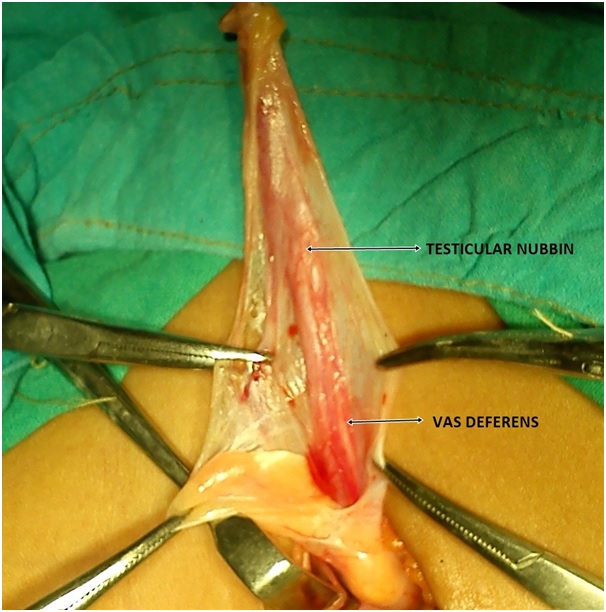
A 6-year-old boy presented with normally descended left testicle and non palpable right testis with an initial diagnosis of right cryptorchidism. On ultrasonography right testis was not visualised along the normal pathway of descent and even in the ectopic locations. The patient underwent right inguinal exploration; right spermatic cord with small oval nodular mass of firm tissue (fibrous nubbin) identified [Table/Fig-4] , was removed and sent for histological analysis.
Histopathological examination showed spermatic cord, unremarkable epididymal tissue and fibrous nodule with variably sized congested blood vessels (VFN). Slit like space lined by mesothelium showing papillary hyperplasia are also seen admixed with fibrous tissue.
left sided spermatic cord with small oval nubbin at distal end
Microscopic examination (H & E) showing spermatic cord and rudimentary epididymis
Microscopic examination (H & E) showing tunica with underlying vascularised fibrous nodule and few hemosiderophage
Presumed left testicular remnants with spermatic cord
Discussion
The non palpable absent testicle when associated with blind ending spermatic cord is referred to as the “vanishing testis syndrome” [1] in the urological literature or “Testicular regression syndrome”[2] in pathological literature. TRS is characterized by partial or total absence of testicular tissue, unilateral or bilateral, with or without rudimentary epididymis and spermatic cord structure in 46XY Sectionindividual with normal external genitalia [3]. Regarding the aetiology of TRS, the theory of an ischemic event in early or late foetal stage is the most accepted because finding such as dystrophic calcification, hemosiderin deposits and giant cells corroborate this hypothesis [4] The presence of spermatic cord structure is evidence of the presence of the testis in early intrauterine life.
The pathological diagnosis of TRS can be established by the presence of the following diagnostic criteria: (1) a vascularised fibrous nodule with calcification and/or hemosiderin. (2) A minimum of a vascularised fibrous nodule with cord element(s) in proximity [3].
As far the management of cases of non palpable testis on physical examination, most surgeons opt for laparoscopic exploration as the primary intervention. The laparoscopy is followed by inguinal exploration in cases where spermatic vessels are seen passing through internal inguinal ring [4,5]. The surgical literature regarding TRS emphasizes the importance of identifying the vascular supply and drainage of the gonad. This is due to the fact that the testis cannot be present in a location absent of gonadal vein and because the vein and pampiniform plexus almost always indicate the location of the testis, regardless of the presence of vas deference and epididymis[3].
Surgical exploration is required to perform the orchidopexy for those cases in which the testis is present but not topic (cryptorchidism). However, there is disagreement regarding the removal of the remnant structures in cases of TRS. These structures were detected in up to 11% of reported cases and among these, cellular atypia was found in up to 26% [4,6]. We found a single case report of malignant transformation of testicular remnants in a cases of TRS [7]. Most authors believe that the removal must be performed because of the lack of data regarding the risk of malignant transformation of testicular or paratesticular remnants containing germ cells. Some authors further claim the surgical fixation of the contra lateral testis in order to reduce the risk of testicular torsion and thus ensuring good chances of fertility for the patients with TRS [8].
Some studies show that the loss or absence of testicles can have negative psychological effects on adult men or children. Therefore, surgery for testicular prosthesis implantation is a solution that minimizes psychological consequences of the absence of the testicle in the scrotum, providing similarity in size, weight and appearance of natural testicle [9].
Furthermore, one should consider the possibility of orchidopexy and testicular prosthesis implantation to minimize the risk of testicular torsion of the viable tissue and negative psychological effect.
[1]. DA Diamond, AA Caldamone, The value of laparoscopy for a 106 impalpable testis relative to clinical presentationJ Urol 1992 148:632-34. [Google Scholar]
[2]. DM Selby, Sexual maldevelopment syndromes. In: Stocker JT, Dehner LP, eds. Pediatric Pathology 1992 PhiladelphiaJB Lippincott Co:117-59. [Google Scholar]
[3]. NM Smith, RW Byard, AJ Borne, Testicular regression syndrome- a pathological study of 77 casesHistopathology. 1991 19:269-72. [Google Scholar]
[4]. MI Beder, R Peeraully, Ba M Ath, J Mcpartland, J Baillie, C Baillie, The testicular regression syndrome- do remnant required routine excision?J Pediatric Surg 2011 46(2):384-86. [Google Scholar]
[5]. A EITayeb, The unilateral impalpable testis: does the order of the procedure affect the outcome?Ann Pediatric Surg 2009 5:115-18. [Google Scholar]
[6]. D Storm, T Redden, M Aguiar, M Wilkerson, G Jordon, J Sumfest, Histologic evaluation of the testicular remnant associated with the vanishing testis syndrome: is surgical management necessary?Urology. 2007 70:1204-06. [Google Scholar]
[7]. TA Rozanski, KJ Wojno, DA Bloom, The remnant orchiectomyJ Urol 1996 155(2):712-14. [Google Scholar]
[8]. M Nistal, R Paniagua, Non-neoplastic diseases of the testis, In: Bostwick DG, Cheng L, editors. Urologic surgical pathology 2008 2nd EditionModby Elsevier:632-35. [Google Scholar]
[9]. D Bodiwala, DJ Summerton, TR Terry, Testicular prosthesis: development and modern usage.Ann R Coll Surg Engl 2007 89(4):349-53. [Google Scholar]