Primary Pulmonary Ewing’s Sarcoma: Rare Cause of Superior Vena Cava Syndrome in Children
Shibani Mehra1, Swapndeep Singh Atwal2, Umesh Chandra Garga3
1 Associate Professor, Department of Radiology, Dr. Ram Manohar Lohia Hospital and PGIMER, New Delhi, India.
2 Senior Resident, Department of Radiology, Dr. Ram Manohar Lohia Hospital and PGIMER, New Delhi, India.
3 Professor and Head of Department, Department of Radiology, Dr. Ram Manohar Lohia Hospital and PGIMER, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Swapndeep Singh Atwal, 8/4, 3rd Floor, Old Rajender Nagar, New Delhi-110060, India. Phone : 9013837423, E-mail : swapndeepsinghatwal@gmail.com
Ewing’s sarcoma is a common malignant bone tumour presenting in children and young adults. Rarely extra- skeletal soft tissues and visceral organs can also be the site of origin of Ewing’s sarcoma. Primary pulmonary Ewing’s sarcoma is an extremely rare malignancy which occurs in the paediatric population. We report an unusual case of primary pulmonary Ewing’s sarcoma in a nine year old girl who presented with features of superior vena cava syndrome in the emergency department. The diagnosis was confirmed pathologically both by light microscopy and immunohistochemistry. The patient was put on chemotherapy and surgery was planned but the patient expired within three days of starting chemotherapy.
Children, Ewing’s sarcoma, Pulmonary, Superior vena cava (SVC) syndrome
Case Report
A 9-year old female child presented in the emergency with gradually increasing chest pain, dry cough, dyspnoea and weight loss over 3 months, which had worsened since two days. She had developed swelling over the face and neck since 2 days. There was no history of trauma and no other significant history. On physical examination, she had marked facial oedema and prominent neck veins and chest wall veins. A solitary enlarged right axillary lymph node was palpable. Auscultation over the chest showed reduced air entry in the right hemithorax. The haematological investigations revealed marked anaemia with haemoglobin level of 8.7gm/dl. Rest of the biochemical investigations were within normal range.
A chest radiograph frontal view was obtained which revealed complete opacification of the right hemithorax. The trachea and the mediastinum were displaced towards the left hemithorax. However, the left lung fields showed normal aeration with the left cardio- phrenic and costphrenic angles being unremarkable [Table/Fig-1].
Chest radiograph postero-anterior view showing homogenous opacification of right hemithorax and mediastinal shift towards left side

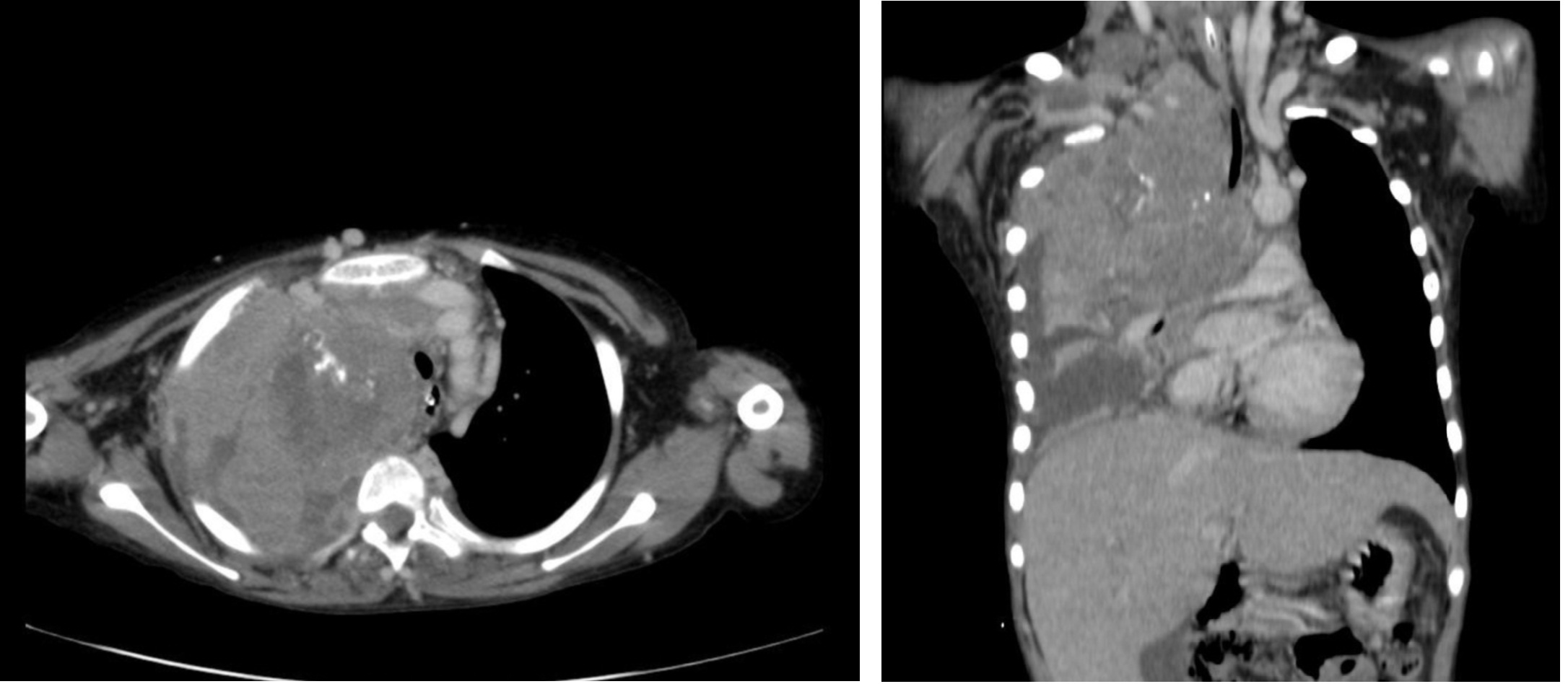
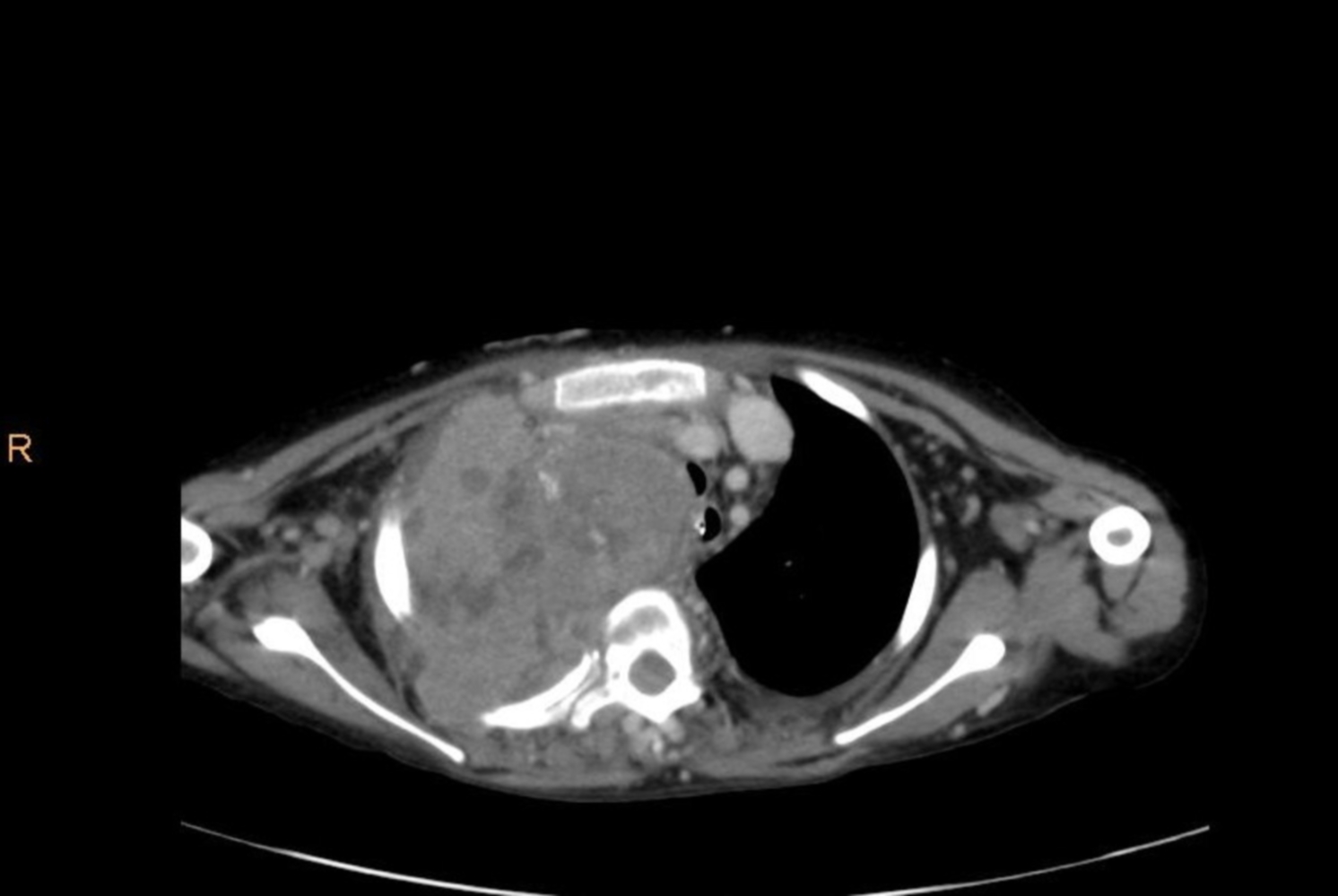
Subsequently contrast enhanced computed tomography (CT) chest was performed on Philips Brilliance multidetector scanner for further evaluation of the lung parenchyma. The images demonstrated a large ill-marginated mass involving the upper lobe of right lung with few specks of calcification seen within. The mass showed moderate enhancement with few necrotic areas [Table/Fig-2a,b].The mass was seen to encase and involve the superior vena cava with encasement of the ascending aorta, the main and right branch of the pulmonary artery [Table/Fig-3]. The trachea was compressed by the mass and displaced to the left. Moderate right pleural effusion with collapse of right middle and lower lobe was evident in the images. There were soft tissue attenuation nodular enhancing pleural based densities suggestive of metastatic subjacent pleural deposits in the right lower chest [Table/Fig-4]. The ribs and vertebrae did not show any lytic areas. A, whole body CT scan was then performed to look for possible metastasis and subsequently an MRI brain was also done. No intracranial or intra-abdominal visceral or peritoneal metastases were found, without any metastatic extra or intra -thoracic skeletal involvement.
Contrast enhanced computed tomography chest (a) axial (b) coronal image in mediastinal window showing a large heterogeneously enhancing mass with non-enhancing necrotic areas within involving upper lobe of right lung invading the mediastinum
Contrast enhanced computed tomography chest axial image. Superior vena cava encased by the mass with encasement of pulmonary trunk and right pulmonary artery
Contrast enhanced computed tomography chest axial image showing nodular enhancing pleural deposits and pleural effusion on the right side

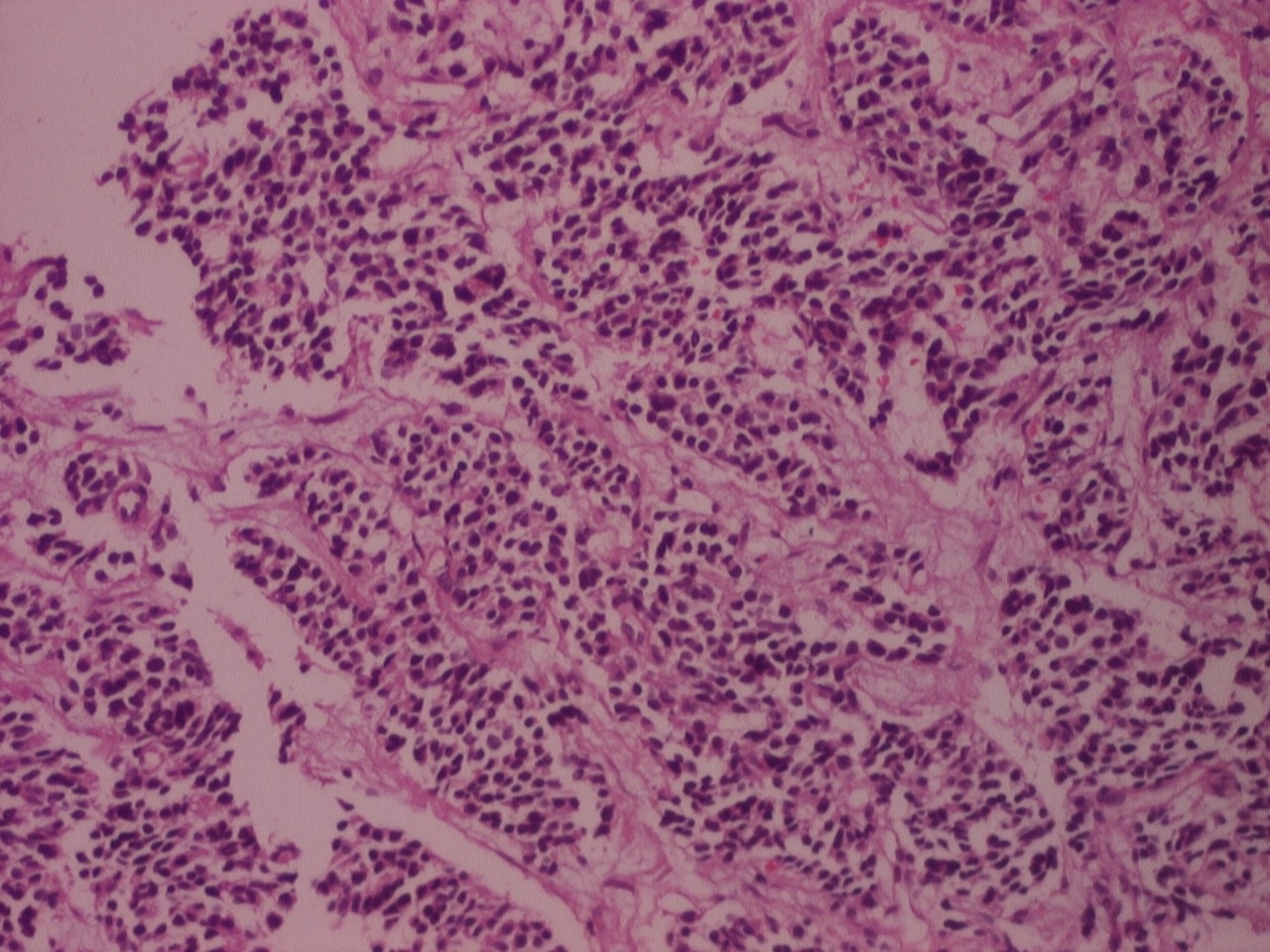
A CT-guided biopsy of the lesion was done with histopathological evaluation of the biopsy specimen. Microscopy revealed nests of pleomorphic small round cells arranged in sheets and clumps, with round -oval to bizarre shaped nuclei, with intervening fibrous strands and engorged blood vessels [Table/Fig-5]. The cells were found to be CD99 positive on immunohistochemistry. This is characteristic of Ewing’s sarcoma as well as primitive neuroectodermal tumours. The patient was initially started on chemotherapy with Vincristin, Actinomycin, and Cyclophosphamide and surgical resection of the mass were planned to relieve the patient from symptoms of Superior Vena Cava obstruction. However, the child died within three days of starting the chemotherapy.
Histopathological slide showing pleomorphic round cells with intervening fibrous strands and engorged vessels
Discussion
Extraosseus Ewing’s sarcoma is a subset of primitive neuro ectod- ermal tumours (PNET) which involves the soft tissues very rarely [1]. Initially, paravertebral soft tissue tumours were described in four patients with histologic appearance resembling Ewing’s sarcoma. Extraosseous Ewing’s tumours were subsequently reported in other organs like ovary, testis, uterus, pancreas, the lung and even in the myocardium [1,2,3]. Primary pulmonary Ewing’s sarcoma is rare and only thirteen cases have been reported in the literature to the best of our knowledge.
In the present case, the patient was a nine years old girl presented with the features of superior vena cava (SVC) syndrome caused by the intrathoracic mass compressing the superior vena cava and also encasing other superior mediastinal vasculature. There were associated pleural deposits. It was confirmed as Ewing’s sarcoma on histopathology and immunohistochemistry. The case highlights that EES of the lung can be a rare cause of SVC syndrome in children. Pulmonary Ewing’s sarcoma has been reported to occur predominantly in adolescents and adult patients as a circumscribed solitary mass showing heterogeneous enhancement with non-enhancing necrotic areas within. Intralesional amorphous calcification and associated pleural effusion has also been reported [4]. Only one case of primary pulmonary Ewing’s has been described in a child of less than ten year age where it presented as a lobulated intraparenchymal discrete mass in the right lung without any vascular encasement or superior vena cava syndrome. There were no pleural deposits in that case [5]. The lungs being extremely rare and unusual location for the extra-osseous variety of Ewing’s sarcoma, and the paediatric age of presentation which has been reported only once so far, prompted us to present and publish this case. Another unusual finding in our case was the presence of superior vena cava syndrome and pleural deposits which have not been reported in literature in association with a pulmonary PNET, although pleural deposits can very well be associated with and have been described with other aggressive round cell sarcomas.
Primary pulmonary neoplasms are rare and few in children. Metastatic pulmonary masses from a primary Wilm’s tumour, a Rhabdomyosarcoma or an Osteogenic sarcoma of the bone which are mostly multifocal have been more common. The primary lung neoplasms in paediatric population are Carcinoids and Blastomas [4,6]. These masses should be considered in differential diagnosis of Primary pulmonary Ewing’s.
The diagnosis of extraosseous Ewings sarcoma is essentially histological and relies on the pathologic features of the specimen. The classical histopathological findings consist of round cells, with irregularly shaped chromatic nuclei surrounded by scanty cytoplasm. Mitotic figures may be seen. The cells often show immuno-histochemical positivity for various neurofilaments such as, CD99, and S-100 [2].
Conclusion
Although Pulmonary Ewing’s is a rare malignancy, it must be considered in the differential diagnosis of any primary lung mass in children and more so should be excluded when Superior vena cava syndrome is encountered in the paediatric age group.
[1]. Lee YY, Kim DH, Lee JH, Choi JS, In KH, Oh YW, Primary Pulmonary Ewing’s Sarcoma/Primitive NeuroectodermalTumor in a 67-year-old ManJ Korean Med Sci 2007 22(Suppl):S159-63.[PMCID: PMC2694395] [Google Scholar]
[2]. Narula MK, Gupta N, Anand R, Kapoor S, Extraosseous Ewing’s sarcoma / primitive neuroectodermaltumor of the sacral nerve plexusIndian J Radiol Imaging 2009 19(2):151-54.[PMCID: PMC2765184] [Google Scholar]
[3]. Tefft M, Vawter GF, Mitus A, Paravertebral “round cell” tumors in childrenRadiology 1969 92:1501-09.[PubMed: 5799839] [Google Scholar]
[4]. Shet N, Stanescu L, Deutsch G, Primary extraosseous Ewing sarcoma of the lung: Case report and literature reviewRadiology Case Reports. (Online) 2013 8:832 [Google Scholar]
[5]. Takahashi D, Nagayama J, Nagatoshi Y, Inagaki J, Nishiyama K, Yokoyama R, Primary Ewing’s sarcoma family tumors of the lung a case report and review of the literatureJapanese Journal of Clinical Oncology 2007 37(11):874-77. [Google Scholar]
[6]. Gladish GW, Sabloff BM, Munden RF, Truong MT, Erasmus JJ, Chasen MH, Primary thoracic sarcomasRadiographics 2002 22(3):621-37.[PubMed] [Google Scholar]